Podcast
Questions and Answers
What is the primary metabolic fate of carbon skeletons from degraded amino acids in mammals?
What is the primary metabolic fate of carbon skeletons from degraded amino acids in mammals?
- They are stored as fats.
- They are converted to nitrogenous waste.
- They form ketone bodies exclusively.
- They are converted to glucose or oxidized in the citric acid cycle. (correct)
Which amino acids are classified as solely ketogenic?
Which amino acids are classified as solely ketogenic?
- Methionine and cysteine
- Tyrosine and tryptophan
- Isoleucine and phenylalanine
- Leucine and lysine (correct)
Which condition is primarily associated with deficiencies in cystathionine synthase and cystathionase?
Which condition is primarily associated with deficiencies in cystathionine synthase and cystathionase?
- Phenylketonuria
- Homocystinuria (correct)
- Arginosuccinase deficiency
- Cystathionuria
What metabolic intermediate is produced from glucogenic amino acids?
What metabolic intermediate is produced from glucogenic amino acids?
What is a common result of cystathionuria in adults?
What is a common result of cystathionuria in adults?
Which of the following diseases is NOT associated with amino acid metabolism?
Which of the following diseases is NOT associated with amino acid metabolism?
Which type of amino acids can contribute to the formation of both ketone bodies and glucose?
Which type of amino acids can contribute to the formation of both ketone bodies and glucose?
What effect does the maturation of premature infants have on cystathionine levels in urine?
What effect does the maturation of premature infants have on cystathionine levels in urine?
What is a key metabolic fate of the carbon atoms derived from degraded amino acids?
What is a key metabolic fate of the carbon atoms derived from degraded amino acids?
Which metabolic intermediates can be derived from glucogenic amino acids?
Which metabolic intermediates can be derived from glucogenic amino acids?
Which of the following describes the relationship between leucine and lysine?
Which of the following describes the relationship between leucine and lysine?
What characterizes cystathionuria in adults?
What characterizes cystathionuria in adults?
What is the cause of homocystinuria?
What is the cause of homocystinuria?
What is a possible effect of high levels of homocyst(e)ine in the blood?
What is a possible effect of high levels of homocyst(e)ine in the blood?
What role do isoleucine, phenylalanine, tryptophan, and tyrosine play in amino acid metabolism?
What role do isoleucine, phenylalanine, tryptophan, and tyrosine play in amino acid metabolism?
Which amino acid metabolism-related condition is characterized by presence of cystathione in urine in premature infants?
Which amino acid metabolism-related condition is characterized by presence of cystathione in urine in premature infants?
Flashcards
Amino Acid Degradation
Amino Acid Degradation
The process of breaking down amino acids into smaller molecules and converting their carbon skeletons into key metabolic intermediates.
Metabolic Intermediates from Amino Acids
Metabolic Intermediates from Amino Acids
The breakdown of amino acids produces intermediates that can be used to make glucose or enter the Citric Acid Cycle (for energy).
Ketogenic Amino Acids
Ketogenic Amino Acids
Amino acids that are degraded to acetyl CoA or acetoacetyl CoA. They can be used to produce ketone bodies or fatty acids.
Glucogenic Amino Acids
Glucogenic Amino Acids
Signup and view all the flashcards
Argininosuccinic Aciduria
Argininosuccinic Aciduria
Signup and view all the flashcards
Homocystinuria
Homocystinuria
Signup and view all the flashcards
Cystathionuria
Cystathionuria
Signup and view all the flashcards
Homocystinuria and Cystathionuria
Homocystinuria and Cystathionuria
Signup and view all the flashcards
What is Argininosuccinic Aciduria?
What is Argininosuccinic Aciduria?
Signup and view all the flashcards
What is Homocystinuria?
What is Homocystinuria?
Signup and view all the flashcards
What is Cystathionuria?
What is Cystathionuria?
Signup and view all the flashcards
What is Cystathionuria?
What is Cystathionuria?
Signup and view all the flashcards
What is Homocystinuria?
What is Homocystinuria?
Signup and view all the flashcards
Study Notes
Amino Acid Metabolism 3
- Excess nitrogen, in mammals, is converted to urea and excreted
- Carbon atoms from degraded amino acids become major metabolic intermediates
- These intermediates can be converted to glucose or oxidized via the citric acid cycle
- Examples of intermediates include pyruvate, acetyl CoA, acetoacetyl CoA, α-ketoglutarate, succinyl CoA, fumarate, and oxaloacetate
- Some amino acids are purely ketogenic
- Others are solely glucogenic
- Some amino acids are both glucogenic and ketogenic
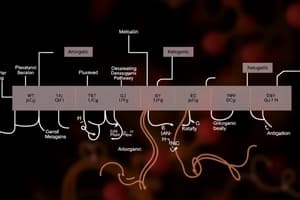
Ketogenic and Glucogenic Amino Acids
- Ketogenic amino acids are degraded to acetyl CoA or acetoacetyl CoA
- These can lead to ketone bodies or fatty acids
- Glucogenic amino acids are degraded to pyruvate, α-ketoglutarate, succinyl CoA, fumarate, or oxaloacetate
- These can be used to produce glucose
- Only leucine and lysine are solely ketogenic
- Isoleucine, phenylalanine, tryptophan, and tyrosine are both ketogenic and gluconeogenic
Diseases Associated with Amino Acid Metabolism
- Inborn Errors of amino acid metabolism
- Diseases caused by enzyme deficiencies
- Examples:
- Citrullinemia (Arginosuccinate lyase deficiency)
- Tyrosinemia (various tyrosine degradation enzyme deficiencies)
- Albinism (Tyrosinase deficiency)
- Homocystinuria (Cystathionine β-synthase deficiency)
- Hyperlysinemia (α-aminoadipic semialdehyde dehydrogenase deficiency)
Detailed Analysis of Specific Diseases
Cystathionuria
- Cystathionuria is relatively common in premature infants
- In adults, genetic deficiency of cystathionase can cause cystathionuria
- Benign condition
Homocystinuria
- Deficiencies in cystathionine and cystathionine synthase enzymes cause this condition
- Results in increased homocystine and methionine in the blood
- Type III and II are caused by deficiencies of 5-methyltetrahydrofolate and vitamin B12, respectively
- Eye problems, bone problems, vascular damage, thrombi, and emboli are potential complications
- Zonal fibres in the eye may fray and break leading to dislocation of the lens
- Osteoporosis and spine curvature can occur
- Long bones may elongate
- High homocysteine correlates with atherosclerosis and heart attack
Phenylketonuria (PKU)
- Autosomal recessive disorder, defect in phenylalanine hydroxylase
- Deficiency in phenylalanine hydroxylase, B6, tetrahydrobiopterin, or tetra hydrobiopterin reductase
- Increased phenylalanine levels in patients, normal levels are <1-2mg/dL
- Mental retardation, delayed psychomotor maturation, tremors, seizures, eczema, and hyperactivity
- Special semi-synthetic preparations such as Lofenalac (casein substitute) are used to restrict dietary phenylalanine
Tyrosinaemia
- Frequently observed in premature newborns. Conditions appear benign. Dietary restrictions return tyrosine to normal levels
- Tyrosinaemia II results from a deficiency of tyrosine aminotransferase- May involve eye and skin lesions as well as neurological problems.
- Tyrosinaemia I (tyrosinosis) is caused by the genetic deficiency of fumarylacetoacetate hydrolase- Acute form is associated with liver failure and a cabbage-like odour, and death within the first year of life.
- Tyrosinaemia I symptoms potentially include a cabbage-like odour
Alcaptonuria
- Occurs when homogentisate can't be further oxidized (homogentisate oxidase)
- Homogentisate accumulates and auto-oxidizes, forming dark pigment that discolors urine
- Chronic accumulation in cartilage can cause arthritic joint pain
- Urine can become black upon standing, or turn red-brown if exposed to air or alkali
Maple Syrup Urine Disease (MSUD)
- Due to a deficiency in α-keto acid dehydrogenase in branched-chain amino acids.
- Leads to mental and physical retardation.
- Urine has a distinctive maple syrup odor
Screening for MSUD
- Screening of newborn urine using 2,4-dinitrophenylhydrazine
- Reacts with α-ketoacids to form 2,4-dinitrophenylhydrazone derivatives
Amino Acids as Precursors to Other Biomolecules
- Amino acids are precursors for various biomolecules such as:
- Adenine, Cytosine, Histamine, Serotonin, Thyroxine, Epinephrine, Creatine.
- These include important neurotransmitters and nucleotides
- Tyrosine is a precursor to thyroid hormones, catecholamines (e.g., dopamine, norepinephrine, adrenaline), and melanin
- Tryptophan is a precursor to serotonin and melatonin
- Amino acids are precursors to important molecules like haem, neurotransmitters, and nucleotide bases
Creatine Biosynthesis
- Synthesized in the liver by methylation of guanidoacetate
- Guanidoacetate is produced in the kidneys from arginine and glycine
- Creatine is used as a storage form of high-energy phosphate.
- Creatine phosphate donates phosphate to ADP when energy demand is high.
- Creatinine is formed in muscles from spontaneous creatine phosphate breakdown through a non-enzymatic dehydration and phosphate loss. Creatinine production is relatively steady, around 1.8 g per day. The SLC6A8 transporter brings creatine into cells (with 2Na+ and a Cl−). The transporter is insulin-sensitive.
Porphyrins
- The first step involves Gly combining with succinyl CoA.
- Catalyzed by the mitochondrial PLP enzyme δ-aminolevulinate synthase
- The carboxyl group of Gly is lost as CO2
Porphyrias
- Inherited or acquired disorders caused by enzyme deficiency in heme biosynthesis pathway
- Examples include congenital erythropoietic porphyria, caused by insufficient cosynthase; symptoms include red urine and skin sensitive to UV light
- Symptoms vary depending on the specific enzyme deficiency
Acute Intermittent Porphyria
- Characterized by overproduction of porphobilinogen and δ-aminolevulinate
- Due to the deficiency in porphobilinogen deaminase
- Severe abdominal pain and neurological dysfunction
- Attacks can be triggered by drugs like barbiturates which increases the synthesis of hepatic CytP450
Biosynthesis of Purines and Pyrimidines
- Amino acids are needed for purines and pyrimidines biosynthesis
Purine Degradation
- Source of NH4+ and uric acid
- Enzymes involved include adenosine deaminase, hypoxanthine guanine phosphoribosyltransferase, purine nucleotide phosphorylase, xanthine oxidase and others.
- Allopurinol inhibits xanthine oxidase
Diseases with Purine Degradation
- Severe combined immunodeficiency (SCID) is an inborn error of metabolism involving adenosine deaminase, leading to reduced T and B lymphocytes and impairments in DNA synthesis.
- Self-mutilation behaviours can be observed
- Gout involves excessive uric acid in circulation, which can crystalize out and cause inflammation.
- Treated with Allopurinol to inhibit xanthine oxidase
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.