Podcast
Questions and Answers
Which statement accurately contrasts Entamoeba histolytica and Entamoeba dispar?
Which statement accurately contrasts Entamoeba histolytica and Entamoeba dispar?
- _E. histolytica_ possesses virulence properties, distinguishing it from the morphologically distinct _E. dispar_.
- _E. histolytica_ and _E. dispar_ are genetically identical but differ in their surface antigens.
- _E. histolytica_ causes self-limited infections, while _E. dispar_ is associated with invasive disease.
- _E. histolytica_ has unique surface antigens, is genetically distinct and possesses virulence properties that distinguish it from the morphologically identical _E. dispar_. (correct)
How do E. histolytica trophozoites evade host defenses during intestinal invasion?
How do E. histolytica trophozoites evade host defenses during intestinal invasion?
- By rapidly encysting when exposed to air or stomach acid.
- By digesting antimicrobial peptides with amebic cysteine proteinases. (correct)
- By expressing glutathione and glutathione reductase.
- By neutralizing antimicrobial peptides through the production of interleukins.
What role do commensal bacteria play in the virulence of E. histolytica infections?
What role do commensal bacteria play in the virulence of E. histolytica infections?
- Commensal bacteria increase expression of Gal/GalNAc lectin, increasing virulence.
- Commensal bacteria, like _E. coli_, can attenuate the virulence of _E. histolytica_ by decreasing Gal/GalNAc lectin expression. (correct)
- Commensal bacteria have no impact on the virulence of _E. histolytica_.
- Enteropathogenic bacteria decrease expression of Gal/GalNAc lectin, increasing virulence.
What is the function of prostaglandin E2 in the pathogenesis of amebiasis?
What is the function of prostaglandin E2 in the pathogenesis of amebiasis?
Which defense mechanism against E. histolytica is rendered less effective due to the parasite's enzymatic activity?
Which defense mechanism against E. histolytica is rendered less effective due to the parasite's enzymatic activity?
What role is indicated for Interleukin 10 (IL-10) in the context of amebiasis?
What role is indicated for Interleukin 10 (IL-10) in the context of amebiasis?
How does passive immunity via breastfeeding impact E. histolytica infections in infants?
How does passive immunity via breastfeeding impact E. histolytica infections in infants?
What relevance does the finding of serum Immunoglobulin G (IgG) antibodies have for children from Bangladesh with E. histolytica?
What relevance does the finding of serum Immunoglobulin G (IgG) antibodies have for children from Bangladesh with E. histolytica?
What is the significance of identifying E. histolytica trophozoites with ingested erythrocytes in a stool sample?
What is the significance of identifying E. histolytica trophozoites with ingested erythrocytes in a stool sample?
If a patient is suspected of fulminant colitis, what procedure should be avoided due to the risk of perforation?
If a patient is suspected of fulminant colitis, what procedure should be avoided due to the risk of perforation?
Why are amebic liver abscesses more prevalent in men aged 30-60?
Why are amebic liver abscesses more prevalent in men aged 30-60?
Following successful treatment of an amebic liver abscess, what accounts for persistent abnormalities seen on ultrasound studies?
Following successful treatment of an amebic liver abscess, what accounts for persistent abnormalities seen on ultrasound studies?
In areas with lower rates of malaria transmission, why do some regions see an increase of symptomatic malaria patients during the rainy season?
In areas with lower rates of malaria transmission, why do some regions see an increase of symptomatic malaria patients during the rainy season?
What is the most reliable measure of malaria transmission rate?
What is the most reliable measure of malaria transmission rate?
How does the parasite resist becoming toxic with excessive amounts of heme, following consumption and degradation of proteins in the cell?
How does the parasite resist becoming toxic with excessive amounts of heme, following consumption and degradation of proteins in the cell?
What alteration contributes to necrosis of hepatocytes and explains the fluid variability for patients who have amebic liver abscess?
What alteration contributes to necrosis of hepatocytes and explains the fluid variability for patients who have amebic liver abscess?
How are merozoites attached to erythrocytes?
How are merozoites attached to erythrocytes?
What aspect has to be well maintained to ensure successful transmission of Malaria?
What aspect has to be well maintained to ensure successful transmission of Malaria?
Why specifically is passive resistance a sign for cerebral malaria?
Why specifically is passive resistance a sign for cerebral malaria?
Which is an important function of Primaquine as it pertains to malaria?
Which is an important function of Primaquine as it pertains to malaria?
Select the correct item that influences the clinical syndrome of amebiasis that also has the therapy to resolve.
Select the correct item that influences the clinical syndrome of amebiasis that also has the therapy to resolve.
Although they improve survival rates for severe cases, what complication is now resulting in quinine treatments?
Although they improve survival rates for severe cases, what complication is now resulting in quinine treatments?
To what do physicians attribute noncardiogenic pulmonary edema?
To what do physicians attribute noncardiogenic pulmonary edema?
According to expert reports, which of the following factors are needed to contain malaria?
According to expert reports, which of the following factors are needed to contain malaria?
A positive PfHRP2 test has a low specificity in identifying malaria. Why?
A positive PfHRP2 test has a low specificity in identifying malaria. Why?
Regarding indications for aspiration of liver abscesses, which of the following statements is true?
Regarding indications for aspiration of liver abscesses, which of the following statements is true?
Which statement captures the implications of multi-drug resistance for Malaria?
Which statement captures the implications of multi-drug resistance for Malaria?
For diagnosis purposes, what is particularly useful in determining diagnosis of a parasite?
For diagnosis purposes, what is particularly useful in determining diagnosis of a parasite?
What is the importance of miltefosine?
What is the importance of miltefosine?
Most of the B mandrillaris infections have been discovered at what locations?
Most of the B mandrillaris infections have been discovered at what locations?
Given the context of Primary Amebic Meningoencephalitis (PAM), when should Naegleria infection be considered?
Given the context of Primary Amebic Meningoencephalitis (PAM), when should Naegleria infection be considered?
When should empiric therapy for an active bacterial infection begin?
When should empiric therapy for an active bacterial infection begin?
What is the implication of positive serologic findings with ameboma, colitis, or liver abscess?
What is the implication of positive serologic findings with ameboma, colitis, or liver abscess?
Flashcards
Amebiasis
Amebiasis
Infection caused by Entamoeba histolytica, ranging from asymptomatic colonization to colitis or liver abscesses.
E. histolytica transmission
E. histolytica transmission
Acquired by ingesting viable cysts in contaminated water/food.
Endemic areas for amebiasis
Endemic areas for amebiasis
Locations with poor sanitation where E. histolytica is common.
Asymptomatic amebiasis
Asymptomatic amebiasis
Signup and view all the flashcards
Invasive amebiasis
Invasive amebiasis
Signup and view all the flashcards
Trophozoite invasion
Trophozoite invasion
Signup and view all the flashcards
Necrotic abscesses in amebiasis
Necrotic abscesses in amebiasis
Signup and view all the flashcards
E. moshkovskii
E. moshkovskii
Signup and view all the flashcards
Trophozoite virulence factors
Trophozoite virulence factors
Signup and view all the flashcards
Phagocytosis in E. histolytica
Phagocytosis in E. histolytica
Signup and view all the flashcards
Cathelicidins
Cathelicidins
Signup and view all the flashcards
Intestinal IgA.
Intestinal IgA.
Signup and view all the flashcards
Maternal parasite-specific IgA
Maternal parasite-specific IgA
Signup and view all the flashcards
Earliest Intestinal Lesions
Earliest Intestinal Lesions
Signup and view all the flashcards
Flask-shaped ulcer
Flask-shaped ulcer
Signup and view all the flashcards
Time to amebic liver abscess after leaving endemic area
Time to amebic liver abscess after leaving endemic area
Signup and view all the flashcards
Intestinal mass lesion in amebiasis
Intestinal mass lesion in amebiasis
Signup and view all the flashcards
Most frequent complication of amebic liver abscess
Most frequent complication of amebic liver abscess
Signup and view all the flashcards
Most important diagnostic procedure for amebiasis
Most important diagnostic procedure for amebiasis
Signup and view all the flashcards
Immunoassay detection of the Gal/GalNAc lectin
Immunoassay detection of the Gal/GalNAc lectin
Signup and view all the flashcards
Serology Enzyme-linked immunosorbent assay
Serology Enzyme-linked immunosorbent assay
Signup and view all the flashcards
asymptomatic cyst passage
asymptomatic cyst passage
Signup and view all the flashcards
amebomas
amebomas
Signup and view all the flashcards
Amebic liver abscess
Amebic liver abscess
Signup and view all the flashcards
Differential diagnosis
Differential diagnosis
Signup and view all the flashcards
What are Luminal amebicides?
What are Luminal amebicides?
Signup and view all the flashcards
Tissue amebicides
Tissue amebicides
Signup and view all the flashcards
Luminal agent
Luminal agent
Signup and view all the flashcards
Amebic liver treatment
Amebic liver treatment
Signup and view all the flashcards
Amebic infection
Amebic infection
Signup and view all the flashcards
Disinfection against amebiasis.
Disinfection against amebiasis.
Signup and view all the flashcards
pathogens of are free-living amebae
pathogens of are free-living amebae
Signup and view all the flashcards
Primary amebic meningoencephalitis (PAM)
Primary amebic meningoencephalitis (PAM)
Signup and view all the flashcards
Granulomatous Amebic Encephalitis
Granulomatous Amebic Encephalitis
Signup and view all the flashcards
Study Notes
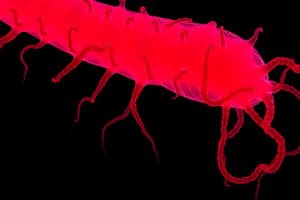
- Amebiasis results from infection by the intestinal protozoan Entamoeba histolytica.
- Clinical syndromes range from asymptomatic colonization to invasive amebiasis.
- Invasive amebiasis manifests as intestinal colitis or extraintestinal amebiasis, with liver abscesses more common than lung or brain involvement.
Life Cycle and Transmission
- E. histolytica spreads through ingesting viable cysts from contaminated water, food, or hands.
- Food-borne transmission is the most common, occurring via shedding cysts by food handlers or growing food with contaminated soil.
- Less common methods include oral-anal sex and direct rectal inoculation.
- Trophozoites are released from cysts in the small intestine, remaining harmlessly in the large bowel in most cases.
- Encystation occurs, and infectious cysts are shed in stool which can survive for weeks in moist environments.
- Trophozoites invade bowel mucosa, causing colitis, or enter the bloodstream.
- Trophozoites do not encyst in active dysentery patients, and hematophagous trophozoites are often in fresh stools.
- Trophozoites are rapidly killed by air or stomach acid and cannot transmit infection.
Epidemiology
- E. histolytica disproportionately impacts underdeveloped tropical regions due to inadequate sanitation and hygiene, often affecting children under 5.
- Regions with high prevalence include the Indian subcontinent, Africa, parts of East Asia (Thailand), and Central and South America (Mexico & Colombia).
- In 2016, amebiasis caused 26,748 deaths of all ages, including 4,567 children under 5 globally.
- In contrast, developed countries primarily see amebiasis in returning travelers, recent immigrants, MSM, military personnel, and institutional inmates.
- GeoSentinel Surveillance Network data (1997-2011) indicates E. histolytica is a common cause of diarrhea in long-term travelers exceeding six months.
- Amebiasis is emerging in developed countries like Japan, especially among HIV-positive patients and MSM.
- Globally, E. histolytica ranks as the second leading parasitic cause of death after malaria.
- Invasive colitis and liver abscesses are more frequent in men, linked to differences in complement-mediated killing and testosterone's effect on interferon y secretion.
- The clinical diversity of Entamoeba infections is due to differences between E. histolytica and E. dispar, with only E. histolytica being truly virulent.
- Most asymptomatic carriers, such as MSM and AIDS patients, harbor E. dispar, resulting in self-limited infections.
- New species of Entamoeba, E. moshkowskii and E. bangladeshi, have been identified and are microscopically identical to E. histolytica.
Pathogenesis and Pathology
- Trophozoites attach to colonic mucus and epithelial cells using Gal/GalNAc adherence lectin, releasing glycosidases and proteases, causing degradation of mucous polymers.
- Cysteine proteinases degrade collagen, elastin, IgA, IgG, and anaphylatoxins C3a and C5a.
- Mucosa damage occurs through contact-dependent (apoptosis, trogocytosis) and contact-independent cytotoxicity.
- Contact-independent cytotoxicity results from production of inflammatory mediators like prostaglandin E2, leading to increased ion permeability of intercellular tight junctions.
- E. histolytica resists reactive oxygen and nitrogen species via hydrogen peroxide-regulatory motif-binding protein overexpression.
- The thioredoxin-thioredoxin reductase system is essential due to the lack of glutathione and glutathione reductase.
- Metronidazole's antiparasitic effect is likely tied to inhibition of this antioxidant system.
- Auranofin, an approved rheumatoid arthritis drug, inhibits thioredoxin reductase and is effective in vitro and in vivo.
- Phagocytosis is a virulence factor, where trophozoites phagocytose intestinal bacteria for nutrients.
- Commensal bacteria like E. coli can reduce E. histolytica's virulence by decreasing Gal/GalNAc lectin expression.
- Enteropathogenic bacteria like E. coli and Shigella dysenteriae increase Gal/GalNAc lectin expression and E. histolytica cysteine protease activity.
- E. histolytica can alter gut microbiota, decreasing Bacteroides, Clostridium coccoides and leptum subgroups, Lactobacillus and Eubacterium, while increasing Bifidobacterium.
- High parasite burden early in life correlates with expansion of Prevotella copri in gut microbiota and presence of diarrhea.
- Cathelicidins, innate immunity peptides, are induced by intestinal invasion in mice.
- IgA is critical in acquired immunity, reducing new E. histolytica infection risk by 64% via intestinal response to Gal/GalNAc.
- Serum IgG antibody is not protective; higher titres are associated with longer duration of illness rather than decreased disease severity.
- Maternal parasite-specific IgA via breastfeeding results in 39% reduced infection risk and 64% reduced diarrheal disease risk from E. histolytica.
- MHC class II allele DQB1*0601 heterozygosity protects against amebic intestinal disease.
- Adipocyte leptin receptors (LEPRs) on intestinal epithelial cells prevent apoptosis, promote tissue repair, and may decrease neutrophil infiltration.
- Micro-ulcerations initially form on mucosa of the cecum, sigmoid colon, or rectum, releasing erythrocytes, inflammatory cells, and epithelial cells.
- Colonoscopies show small ulcers with raised edges and normal intervening mucosa.
- Submucosal extension under viable-appearing surface mucosa prompts classic flask-shaped ulcers containing trophozoites.
- Human intestinal infection has few inflammatory cells because trophozoites kill neutrophils.
- Treated ulcers typically heal with little or no scarring.
- Rarely, amebomas, or mass lesions, form in the bowel lumen, characterized by exuberant granulation tissue.
- Amebic liver abscesses are more common by ~10-12 times in men aged 30-60, a rate demonstrated by studies to modulate interferon y secretion by natural killer T cells.
- Liver abscesses are preceded by intestinal colonization, where blood vessels may be compromised by lysis and thrombus formation.
- Trophozoites resist complement-mediated lysis, and inoculation into the hamster portal system results in acute cellular infiltrate consisting predominantly of neutrophils before toxins released by neutrophils induce hepatocytes.
- The liver parenchyma is replaced by sterile granular necrotic material adjacent to thin capsulated congested tissues.
Clinical Syndromes
- Even in highly endemic regions, most patients pass asymptomatic cysts, usually harboring E. dispar.
- Symptomatic amebic colitis develops 2-6 weeks following cyst ingestion, progressing from mild lower abdominal distress and diarrhea to malaise, weight loss, and lower back pain.
- Patients with full-blown dysentery may pass 10-12 stools per day, consisting mainly of blood and mucus with little fecal material.
- Fewer than 40% of dysentery patients have fever, whereas heme-positive stools are present in the majority.
- Rare fulminant intestinal infection with severe abdominal suffering, elevated temperature, and diarrhea may occur in children or those having glucocorticoids, with a risk for toxic megacolon.
- An occasional patient may have an ameboma, which is easily confused with cancer during barium studies.
- Tropical environmental enteropathy is observed in tropical developing areas with endemic enteric infections, leading to gastrointestinal impairment causing malnutrition and stunted growth in children <2 years old.
- Symptomatic E. histolytica infections associated with significantly higher rates of malnourishment.
- Extraintestinal infection most often involves the liver, where most travelers having abscesses after leaving endemic areas do so within 5 months.
- Young patients with amebic liver abscesses are more likely vs. older patients to present in an acute phase (<10 days' duration) along with fever and right-upper-quadrant pain.
- Older patients from endemic areas are more likely to have a subacute course lasting >6 months, with weight loss and hepatomegaly.
- About a third of chronic presentation patients are febrile, such that the diagnosis may depend on suspected "fever of unknown origin".
Complications of Amebic Liver Abscess
- Pleuropulmonary involvement, reported in 20-30% of patients, is the most frequent complication of amebic liver abscess.
- A hepatobronchial fistula may cause cough productive of large amounts of necrotic material that may contain amebae.
- Abscesses might also rupture into the peritoneum or pericardium.
- Genitourinary tract may become involved by direct extension of amebiasis from the colon or by hematogenous spread of the infection.
- Cerebral involvement has been reported in fewer than 0.1% of patients.
Diagnostic Tests
- Stool examination, serologic tests, and noninvasive imaging are the most key in diagnostics. Positive fecal findings include heme, absent neutrophils, cysts, or trophozoites.
- The definite diagnosis of amebic colitis hinges on identifying hematophagous E. histolytica trophozoites in at least three fresh specimens examined via wet mount, iodine-stained concentrate, and trichrome-stained preparations.
- Cultures can be more sensitive but aren't readily available.
- If stool exams are unrevealing, sigmoidoscopy with ulcer edge biopsy might assist, albeit with fulminant colitis perforation risks.
- Diagnostic accuracy mandates experience since trophozoites might be confused with neutrophils, and E. hartmanni, E. coli, and Endolimax nana cysts require distinction vs E. histolytica.
- The microscopic diagnosis mandates detecting Entamoeba trophozoites that ingested erythrocytes to rule out E. dispar, E. moshkovskii, or E. bangladeshi.
- Enzyme immunoassay stool tests for E. histolytica Gal/GalNAc lectin and multiplex PCR panels are more sensitive and specific.
- Serology is an important addition for invasive amebiasis.
- Positive enzyme-linked immunosorbent and agar gel diffusion assays in >90% of colitis, ameboma, or liver abscess cases suggest active disease because serologic findings usually revert to negative within 6-12 months.
- Repeat negative serologic testing after 1 week in cases of suspected acute amebic liver abscess if initial results are negative.
Radiographic Studies
- Amebomas are usually identified first by barium enema, but biopsy is necessary for differentiation from carcinoma.
- Ultrasonography, CT, and MRI techniques can assess location due to round/oval hypoechoic cyst observation.
- More than 80% of patients having symptoms for >10 days have solitary abscesses of the right liver lobe.
Treatment
- Drugs used to treat intestinal disorders are classified according to the site of action.
- Luminal amebicides are nonabsorbed and reach high bowel concentrations, limiting to cysts as well as those near mucosal surface, including iodoquinol and paromomycin; tissue amebicides such as Metronidazole/Tinidazole for treating Colitis.
- Tinidazole has a greater potency and is versatile for long-term periods.
- Full therapy required, since Matronidazole does not eradicate cysts.
- Shorter Nitroimidazole also proven efficacy (tinidazole/ornidazole).
- A reduction of appropriate doses or durations of therapy promotes tolerance to infection from lower antibiotic properties and failure to heal.
- Metronidazole is the drug of choice for treating amebic liver disorders.
- Studies have demonstrated how nearly 72% individuals that do not have intestinal problems are exposed to E. Histolytica, which is essential to include in all treatment regimens.
- Longer treatments decrease severity rapidly.
- Indications for liver tapping due to Pyogenic reasons, those with multiple lesions, lack of swift healing times, and threat of rupturing lobe.
- Aspiration does not accelerate healing times.
- Surgery must handle bowel ruptures.
- Prevention focuses on ingestion of fecally introduced food and/or water.
- Avoid unpeeled fruits/vegetables.
- No effective prophylaxis exists.
Infection with Free-Living Amebae
- Involves multiple genera, but major human pathogens are Acanthamoeba, Naegleria, and Balamuthia.
- Acanthamoeba is also resistant to protozoa protections from heat shock proteins.
- Multiple studies also suggest water is the origin, but Naegleria's is soil.
- Naegleria contains fulminant CNS infections and Balamuthia contains granulomatous amebic.
- These pathogens include pseudomonas aeruginosa, non-tuberculosis mycobacterium, chlelona, and viruses.
Naegleria Infections
- In the US alone, 138+ cases were reported since 1962, spanning through 2015.
- Reported cases annually have remained roughly stable (0-8).
- Northernmost state cases came from Minnesota, Indiana, and Kansas during 2011-2012.
- 63%+ of samples have shown female presence, with a median age near 11.
- Occurrences happen when aspirations of water become contaminated with trophozites and cysts, plus olfactory neuroepithelium intrusion.
- Incubation spans from 2-15 days.
- A diagnostic PCR test is available through CDC.
- Number of antimicrobial agents, such as azoles, azithromycin, and rifampin, are given throughout samples.
- Miltefosine had been shown success, along with neurologic compilations.
Acanthamoeba infections
- Comes from immunosuppressed or debilitated patients.
- Typically can reach CNS through the primary focus in the skin, sinuses, and lungs.
- Biopsy specimens can test positive regarding protoplasm through non-nutrient agar.
- Includes Balamuthia Madillaris first found in California in 1986.
- Patients are often treated with macrocodes and sulfa-diazine.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.