Podcast
Questions and Answers
Which of the following best describes Alzheimer's disease?
Which of the following best describes Alzheimer's disease?
- Loss of cognitive function primarily due to stroke.
- A mental disorder characterized by acute confusion.
- A type of reversible cognitive impairment.
- A type of progressive dementia with no known cause. (correct)
What is a distinguishing feature of dementia of the Alzheimer type?
What is a distinguishing feature of dementia of the Alzheimer type?
- Excessive production of serotonin.
- Massive increase in cholinergic neurons.
- Reduction of dopamine receptors.
- Neurofibrillary tangles. (correct)
What is the primary neurotransmitter affected in Alzheimer's disease?
What is the primary neurotransmitter affected in Alzheimer's disease?
- Acetylcholine (correct)
- Serotonin
- GABA
- Dopamine
Which of the following drugs is NOT a centrally acting cholinesterase inhibitor?
Which of the following drugs is NOT a centrally acting cholinesterase inhibitor?
What is the main therapeutic goal of using acetylcholinesterase inhibitors in Alzheimer's disease?
What is the main therapeutic goal of using acetylcholinesterase inhibitors in Alzheimer's disease?
Why is the use of drugs for Alzheimer's disease described as palliative?
Why is the use of drugs for Alzheimer's disease described as palliative?
What is the significance of NMDA-glutamate receptors in Alzheimer's treatment?
What is the significance of NMDA-glutamate receptors in Alzheimer's treatment?
What is the first centrally acting cholinesterase inhibitor approved for the treatment of Alzheimer's disease?
What is the first centrally acting cholinesterase inhibitor approved for the treatment of Alzheimer's disease?
What are common symptoms of multiple sclerosis (MS)?
What are common symptoms of multiple sclerosis (MS)?
What is the purpose of prednisone in treating MS?
What is the purpose of prednisone in treating MS?
Which type of MS medication is Interferon β-1b classified as?
Which type of MS medication is Interferon β-1b classified as?
How does Interferon β-1b affect lymphocytes in MS treatment?
How does Interferon β-1b affect lymphocytes in MS treatment?
What characterizes the relapsing-remitting form of MS?
What characterizes the relapsing-remitting form of MS?
What is a key effect of the immuno-modulatory properties of Interferon β-1b?
What is a key effect of the immuno-modulatory properties of Interferon β-1b?
Which of the following statements is true about the chronic nature of MS?
Which of the following statements is true about the chronic nature of MS?
What potential benefit does Interferon β-1a provide for patients with MS?
What potential benefit does Interferon β-1a provide for patients with MS?
What is the primary mechanism of action of memantine in Alzheimer's disease?
What is the primary mechanism of action of memantine in Alzheimer's disease?
Which of the following is a common adverse effect associated with drugs used for Alzheimer's disease?
Which of the following is a common adverse effect associated with drugs used for Alzheimer's disease?
What is the purpose of caprylidene in the treatment of Alzheimer's disease?
What is the purpose of caprylidene in the treatment of Alzheimer's disease?
Which statement best describes the action of NMDA-glutamate receptor antagonists?
Which statement best describes the action of NMDA-glutamate receptor antagonists?
What is the significance of the combination drug Namzaric?
What is the significance of the combination drug Namzaric?
In the context of Alzheimer's disease, what role does excess intracellular Ca2+ play?
In the context of Alzheimer's disease, what role does excess intracellular Ca2+ play?
How does age-related glucose uptake affect patients with Alzheimer's disease?
How does age-related glucose uptake affect patients with Alzheimer's disease?
What type of condition is multiple sclerosis classified as?
What type of condition is multiple sclerosis classified as?
What is a primary function of Glatiramer in treating multiple sclerosis?
What is a primary function of Glatiramer in treating multiple sclerosis?
Which of the following is a possible adverse effect of Peginterferon β-1a?
Which of the following is a possible adverse effect of Peginterferon β-1a?
What is the mechanism of action of Fingolimod?
What is the mechanism of action of Fingolimod?
Why should Teriflunomide be avoided in pregnant women?
Why should Teriflunomide be avoided in pregnant women?
What is a common adverse effect of Dimethyl fumarate?
What is a common adverse effect of Dimethyl fumarate?
What does the PEGylation process achieve in Peginterferon β-1a?
What does the PEGylation process achieve in Peginterferon β-1a?
Which aspect of Teriflunomide's action relates to immune cell activity?
Which aspect of Teriflunomide's action relates to immune cell activity?
What is an effect associated with the first dose of Fingolimod?
What is an effect associated with the first dose of Fingolimod?
What is the estimated lifespan following an ALS diagnosis?
What is the estimated lifespan following an ALS diagnosis?
Which drug is known for its role in managing ALS by potentially prolonging survival time?
Which drug is known for its role in managing ALS by potentially prolonging survival time?
Which mechanism best describes how Riluzole functions in ALS treatment?
Which mechanism best describes how Riluzole functions in ALS treatment?
What is the primary characteristic of Edaravone in the treatment of ALS?
What is the primary characteristic of Edaravone in the treatment of ALS?
Which medication is specifically indicated for controlling spasticity associated with neurological diseases like MS and ALS?
Which medication is specifically indicated for controlling spasticity associated with neurological diseases like MS and ALS?
What is one of the effects of Baclofen when used to treat muscle spasticity?
What is one of the effects of Baclofen when used to treat muscle spasticity?
Which of the following statements about Gabapentin is correct?
Which of the following statements about Gabapentin is correct?
What important aspect of ALS treatment involves symptomatic management?
What important aspect of ALS treatment involves symptomatic management?
Flashcards are hidden until you start studying
Study Notes
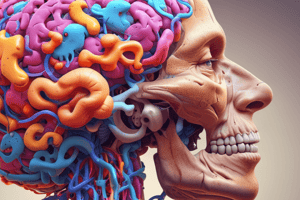
Alzheimer's Disease
- Alzheimer's disease (AD) is a progressive dementia with no known cause or cure.
- It is a common age-related dementia distinct from vascular dementia caused by brain infarction, stroke, trauma or alcohol.
- AD is associated with brain shrinkage and localized loss of neurons, primarily in the hippocampus and basal forebrain.
- AD has a devastating impact on patients and families due to its effects on cognitive, emotional, and physical function.
Features of Alzheimer's Disease
- AD has three distinguishing features:
- Accumulation of senile plaques (β-amyloid accumulations)
- Formation of numerous neurofibrillary tangles
- Loss of cortical neurons, particularly cholinergic neurons
- Patients with AD have a deficit in cholinergic neurotransmission due to the destruction of neurons producing acetylcholine.
- Pharmacologic interventions for AD are palliative and provide modest short-term benefit.
Treatment Goals
- Current therapies for AD aim to:
- Improve cholinergic transmission within the CNS
- Prevent excitotoxic actions resulting from overstimulation of NMDA-glutamate receptors
Acetylcholinesterase Inhibitors
- Donepezil, Galantamine, Rivastigmine, and Tacrine are examples of acetylcholinesterase inhibitors.
- These drugs are used to improve cholinergic neurotransmission in the affected areas of the brain.
- While they may slow cognitive deterioration, they don't affect the underlying neurodegenerative process.
Tacrine (Cognex®)
- The first centrally acting cholinesterase inhibitor approved for AD treatment.
- Slows the progression of AD.
- Common adverse effects include nausea, diarrhea, vomiting, anorexia, tremors, bradycardia, and muscle cramps.
Memantine (Namenda®)
- An NMDA-glutamate receptor antagonist approved for AD treatment.
- It works by attenuating the excitotoxic effects of glutamate, implicated in neuronal loss in AD.
- It is excreted largely unchanged.
- Namzaric®, a combination of memantine extended-release and donepezil, is available.
Caprylidene (Axona®)
- A medical food metabolized into ketone bodies, which the brain can use for energy when glucose processing is impaired.
- MRI scans of the elderly and those with AD reveal decreased glucose uptake, the brain's preferred energy source.
- Caprylidene aims to replace depleted glucose levels for patients with age-associated memory impairment and AD.
Multiple Sclerosis (MS)
- An autoimmune inflammatory demyelinating disease of the CNS with variable course.
- Demyelination disrupts nerve transmission, leading to inflammation and plaque formation in the brain and spinal cord.
MS Symptoms & Treatment
- Symptoms include pain, spasticity, weakness, ataxia, fatigue, and problems with speech, vision, gait, and bladder function.
- Many patients experience relapses and remissions, but some have progressive disease.
- Acute exacerbations are treated with prednisone, which shortens exacerbations and ameliorates symptoms.
- Prednisone is administered orally in milder cases and parenterally in more severe cases.
Disease-Modifying Therapies
- Drugs approved for MS aim to reduce relapse rates and prevent disability accumulation.
- These medications modify the immune response by inhibiting white blood cell-mediated inflammatory processes that damage myelin sheaths.
Interferon β-1b & Interferon β-1a (Betaseron®)
- Interferon β-1b was the first drug to demonstrate the ability to halt and even reverse the progression of MS.
- It reduces inflammatory responses that lead to demyelination.
- Clinical studies showed it reduced relapse frequency and new lesions in patients with relapsing-remitting MS.
Interferon β-1b Mechanism of Action
- Increases natural killer cell cytotoxicity and macrophage phagocytic activity.
- Reduces interferon-γ secretion by activated lymphocytes, which may halt MS progression.
Interferon β-1a
- Approved for relapsing MS and is a synthesized recombinant protein.
- Peginterferon β-1a, a PEGylated derivative, provides longer action.
- Adverse effects may include depression, injection site reactions, hepatic enzyme elevations, and flu-like symptoms.
Glatiramer (Copaxone®)
- A synthetic polypeptide mimicking myelin basic protein, a component of myelin sheaths.
- May act as a decoy to T-cell attack.
- Clinical trials showed reduced relapse episodes compared to placebo.
- Post-injection reactions with flushing, chest pain, anxiety, and itching can occur.
Fingolimod (Gilenya®)
- An oral drug that alters lymphocyte migration, reducing their presence in the CNS.
- Used for relapsing MS patients.
- Exact mechanism unknown, but it is a sphingosine-1-phosphate receptor modulator.
- Prevents lymphocyte egress from lymph nodes, lowering peripheral blood levels and reducing CNS lymphocyte migration.
- May cause first-dose bradycardia and increased risk of infection and macular edema.
- Siponimod and Ozanimod are similar drugs on the market.
Teriflunomide (Aubagio®)
- A pyrimidine synthesis inhibitor used to treat relapsing MS.
- Reduces proliferation and concentration of active lymphocytes in the CNS.
- May elevate liver enzymes and cause hepatic toxicity.
- Avoid during pregnancy.
Dimethyl Fumarate (Tecfidera®)
- Oral drug for relapsing MS that reduces oxidative stress to diminish disease progression.
Amyotrophic Lateral Sclerosis (ALS)
- Characterized by muscle wasting, weakness, respiratory failure, and death within 2-5 years.
- Cause is unknown but involves a defect in superoxide dismutase, an enzyme that scavenges superoxide radicals.
- Treatment for ALS is largely symptomatic.
- Riluzole and Edaravone are indicated for ALS management.
- Baclofen and Gabapentin are used to control spasticity.
Riluzole (Rilutek®)
- The first drug approved for ALS treatment.
- Exact mechanism of action unclear, but it is an NMDA receptor antagonist and may inhibit glutamate release and sodium channels.
- May improve survival time in ALS patients.
- Prolongs time before tracheotomy and extends life by approximately 3 months.
Edaravone (Radicava®)
- A neuroprotective agent that reduces neuronal damage due to oxidative stress, potentially slowing ALS progression.
- FDA-approved for ALS treatment.
Anti-Spastic Agents for MS & ALS
- Used to treat skeletal muscle spasms that may occur from injury or neurological diseases.
- Physical therapy is used for spasticity, but anti-spastic drugs may be helpful in severe cases.
Baclofen (Lioresal®)
- A GABAB receptor agonist that reduces motor neuron excitability.
- Useful for reducing MS-related spasticity, particularly flexor spasms, pain, clonus, and muscle rigidity.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.