Podcast
Questions and Answers
What primarily drives the movement of gases during gas exchange in the lungs and body tissues?
What primarily drives the movement of gases during gas exchange in the lungs and body tissues?
- The speed of blood flow through capillaries
- Partial pressures and matching of perfusion and ventilation (correct)
- Concentration gradients alone
- Active transport of gases across cell membranes
What is the key characteristic of gas exchange?
What is the key characteristic of gas exchange?
- The use of cellular energy to transport gases
- Active movement of gases against concentration gradients
- Passive movement of gases across membranes (correct)
- Movement of fluid
What is the function of external respiration?
What is the function of external respiration?
- Active transport of gases in the blood
- Passive movement of gases across membranes
- The flow of air into the lungs and the transfer of oxygen and carbon dioxide through diffusion (correct)
- Capillary gas exchange in body tissues
What process defines internal respiration?
What process defines internal respiration?
Aside from the 'matching' of ventilation and perfusion, which factor significantly influences alveolar gas exchange?
Aside from the 'matching' of ventilation and perfusion, which factor significantly influences alveolar gas exchange?
What determines the direction of oxygen and carbon dioxide movement across the alveolar membrane?
What determines the direction of oxygen and carbon dioxide movement across the alveolar membrane?
What is the driving force of gas diffusion across the alveolar membrane?
What is the driving force of gas diffusion across the alveolar membrane?
Under normal physiological conditions, how does oxygen move between the alveoli and the blood?
Under normal physiological conditions, how does oxygen move between the alveoli and the blood?
How does carbon dioxide move between the blood and the alveoli?
How does carbon dioxide move between the blood and the alveoli?
What mechanism facilitates the movement of carbon dioxide from the blood into the alveoli during inspiration?
What mechanism facilitates the movement of carbon dioxide from the blood into the alveoli during inspiration?
What determines the amount of gas that dissolves in a liquid?
What determines the amount of gas that dissolves in a liquid?
What is ventilation, in the context of gas exchange?
What is ventilation, in the context of gas exchange?
What is perfusion, in the context of gas exchange?
What is perfusion, in the context of gas exchange?
What primarily controls the diameter of the bronchioles?
What primarily controls the diameter of the bronchioles?
What primarily controls the diameter of the capillaries?
What primarily controls the diameter of the capillaries?
If an alveolus has a high PAO2 and a low PACO2, what physiological response occurs?
If an alveolus has a high PAO2 and a low PACO2, what physiological response occurs?
Why does mixed venous blood have a higher PCO2 and lower PO2 compared to arterial blood?
Why does mixed venous blood have a higher PCO2 and lower PO2 compared to arterial blood?
What are the typical partial pressure values for oxygen and carbon dioxide (PaO2 and PaCO2) in blood leaving the pulmonary capillaries and entering the left heart?
What are the typical partial pressure values for oxygen and carbon dioxide (PaO2 and PaCO2) in blood leaving the pulmonary capillaries and entering the left heart?
During internal respiration, what drives the movement of oxygen from the blood into the tissues?
During internal respiration, what drives the movement of oxygen from the blood into the tissues?
During internal respiration, how does carbon dioxide move from the tissues into the blood?
During internal respiration, how does carbon dioxide move from the tissues into the blood?
Flashcards
Gas exchange
Gas exchange
Passive movement of gases across membranes.
External respiration
External respiration
The flow of air into the lungs coupled with oxygen and carbon dioxide transfer through diffusion.
Internal respiration
Internal respiration
Capillary gas exchange in body tissues.
Partial Pressure Gradient
Partial Pressure Gradient
Signup and view all the flashcards
Ventilation
Ventilation
Signup and view all the flashcards
Perfusion
Perfusion
Signup and view all the flashcards
Partial pressure gradient
Partial pressure gradient
Signup and view all the flashcards
Carbon dioxide diffusion
Carbon dioxide diffusion
Signup and view all the flashcards
Study Notes
- Gas exchange is driven by partial pressures and matching of perfusion and ventilation in lung tissues and the body's tissues.
Definitions
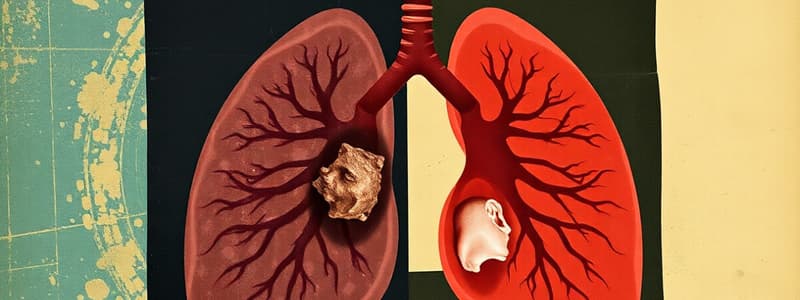
- Gas exchange is the passive movement of gases across membranes.
- External respiration involves the flow of air into the lungs and the transfer of oxygen and carbon dioxide through diffusion.
- Internal respiration is capillary gas exchange in body tissues.
Mechanisms of Alveolar Gas Exchange
- Gas exchange is comprised of three components
- The surface area of the alveolo-capillary membrane.
- The partial pressure gradients of the gasses
- The matching of ventilation and perfusio
Gas Exchange Across Alveolo-Capillary Membrane
- Partial pressure gradients refer to the difference between the partial pressure of gas in the alveolar sac and the partial pressure of gas in the blood .
- This difference is the driving force of gas diffusion across the membrane.
- The partial pressure gradient can also be called the partial pressure gradient, but it is not the concentration difference.
- Partial pressure of a gas in the alveolar sac: PA
- Partial pressure of a gas in the blood: Pa
Movement of Oxygen
- Oxygen diffuses from an area of high partial pressure to an area of low partial pressure.
- PAO2 > PaO2 (Pressure gradient = 60mmHg), moving oxygen into the blood from the alveoli.
Movement of Carbon Dioxide
- Carbon dioxide diffuses from an area of high partial pressure to an area of low partial pressure.
- PACO2 < PaCO2 (Pressure gradient is 5 mmHg) moving carbon dioxide from capillary into alveoli.
Movement of a Gas Between Air and a Liquid (Blood)
- The exchange of carbon dioxide from the blood into the alveoli during inspiration is facilitated.
- The amount of a gas that dissolves in a liquid is directly proportional to the partial pressure of that gas in the air above it.
- Gases can be forced to dissolve into a liquid if enough pressure is applied, or leave if the pressure outside is low.
- Decreasing alveolar pressure causes carbon dioxide dissolved in the blood to leave and return to its gaseous state.
Matching of Ventilation and Perfusion
- Ventilation: Gas reaching alveoli
- Perfusion: Blood flow in pulmonary capillaries servicing those alveoli
- Airways: Diameter of bronchioles, controlled by PACO2
- Blood: Diameter of capillaries, controlled by PAO2
- Alveoli with high PAO2 and low PACO2 cause bronchioles to constrict and pulmonary capillaries to dilate.
- Alveoli with low PO2 and high PCO2 cause bronchioles to dilate and pulmonary capillaries constrict, directing blood to alveoli with more O2.
External Respiration Summary
- Mixed venous blood returns to the right heart from tissues.
- Blood is pumped into the pulmonary artery from the right ventricle, and then delivered to the pulmonary capillaries.
- The PCO2 level in the blood is 45 mm Hg, and PO2 is 40 mm Hg, reflecting the tissues' metabolic activity, where PCO2 > PO2 due to cellular activity.
- O2 and CO2 exchange between alveolar air and pulmonary capillary blood.
- Blood leaving the pulmonary capillaries has the same PO2 and PCO2 as alveolar air (PaO2 is 100 mm Hg; PaCO2 is 40 mm Hg, same as PAO2 and PACO2).
- Blood returns to the left heart and is pumped into the aorta.
Internal Respiration
- Partial pressure of oxygen in tissues is low (40 mm Hg) while it is high in the blood (100 mm Hg).
- An oxygen diffusion gradient causes oxygen to diffuse out of the blood and enter the tissue.
- Partial pressure of carbon dioxide is lower in the blood than in the tissue, so carbon dioxide diffuses out of the tissue and into the blood.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.