Podcast
Questions and Answers
Which adrenal sex hormone is primarily significant in biological processes?
Which adrenal sex hormone is primarily significant in biological processes?
- Testosterone
- Dehydroepiandrosterone (DHEA) (correct)
- Estradiol
- Dihydrotestosterone (DHT)
What controls the secretion of adrenal sex hormones?
What controls the secretion of adrenal sex hormones?
- Adrenocorticotropic Hormone (ACTH) (correct)
- Luteinizing Hormone (LH)
- Follicle-Stimulating Hormone (FSH)
- Gonadotropin-releasing Hormone (GnRH)
At what age does the secretion of adrenal androgens typically peak?
At what age does the secretion of adrenal androgens typically peak?
- 25-30 years (correct)
- 15-20 years
- 35-40 years
- 45-50 years
Which of the following conditions is NOT a disorder of adrenocortical function?
Which of the following conditions is NOT a disorder of adrenocortical function?
Which hormone does DHEA inhibit to affect the hypothalamic-pituitary-adrenal axis?
Which hormone does DHEA inhibit to affect the hypothalamic-pituitary-adrenal axis?
What is one of the main effects of cortisol during acute stress?
What is one of the main effects of cortisol during acute stress?
How does cortisol affect the reproductive axis?
How does cortisol affect the reproductive axis?
What role does cortisol play in inflammatory and immune responses during stress?
What role does cortisol play in inflammatory and immune responses during stress?
What is a common use of glucocorticoid therapy?
What is a common use of glucocorticoid therapy?
Which hormone stimulates the adrenal cortex to secrete cortisol?
Which hormone stimulates the adrenal cortex to secrete cortisol?
What regulates the secretion of ACTH?
What regulates the secretion of ACTH?
What effect do stress and diurnal rhythm have on cortisol secretion?
What effect do stress and diurnal rhythm have on cortisol secretion?
What hormones does the adrenal cortex produce in both sexes?
What hormones does the adrenal cortex produce in both sexes?
What is a characteristic symptom of secondary hyperaldosteronism?
What is a characteristic symptom of secondary hyperaldosteronism?
Which of the following conditions is primarily characterized by excessive gluconeogenesis and high blood glucose levels?
Which of the following conditions is primarily characterized by excessive gluconeogenesis and high blood glucose levels?
What is the term for adrenal-related tumors that produce excessive amounts of hormones?
What is the term for adrenal-related tumors that produce excessive amounts of hormones?
Which of the following best describes the physical appearance associated with Cushing’s syndrome?
Which of the following best describes the physical appearance associated with Cushing’s syndrome?
What symptom might women experience due to increased adrenal androgens in Cushing's syndrome?
What symptom might women experience due to increased adrenal androgens in Cushing's syndrome?
Which physiological effect is directly caused by excessive glucocorticoid levels?
Which physiological effect is directly caused by excessive glucocorticoid levels?
What hormone is most often secreted in excessive amounts due to adenomas of the anterior pituitary?
What hormone is most often secreted in excessive amounts due to adenomas of the anterior pituitary?
Which of the following is a potential outcome of prolonged excess cortisol secretion?
Which of the following is a potential outcome of prolonged excess cortisol secretion?
What factor primarily stimulates aldosterone production?
What factor primarily stimulates aldosterone production?
Which hormone directly inhibits aldosterone production?
Which hormone directly inhibits aldosterone production?
What physiological process is described as aldosterone escape response?
What physiological process is described as aldosterone escape response?
How does a rise in plasma K+ influence aldosterone production?
How does a rise in plasma K+ influence aldosterone production?
What is one of the metabolic functions of cortisol?
What is one of the metabolic functions of cortisol?
What is a result of chronic elevated ACTH levels concerning aldosterone?
What is a result of chronic elevated ACTH levels concerning aldosterone?
Which of the following plays a permissive role alongside cortisol?
Which of the following plays a permissive role alongside cortisol?
What is the primary action of Atrial Natriuretic Peptide (ANP)?
What is the primary action of Atrial Natriuretic Peptide (ANP)?
What hormone is primarily responsible for sodium retention and potassium elimination in the kidney?
What hormone is primarily responsible for sodium retention and potassium elimination in the kidney?
Which hormone is produced in the greatest daily amount by the adrenal cortex?
Which hormone is produced in the greatest daily amount by the adrenal cortex?
What is the role of corticosteroid-binding globulin (CBG) in hormone regulation?
What is the role of corticosteroid-binding globulin (CBG) in hormone regulation?
What happens when aldosterone binds to its mineralocorticoid receptor (MR)?
What happens when aldosterone binds to its mineralocorticoid receptor (MR)?
What is the effect of excess loss of sodium (Na+) without aldosterone?
What is the effect of excess loss of sodium (Na+) without aldosterone?
Which hormone is synthesized and secreted on demand rather than stored within adrenal cortical cells?
Which hormone is synthesized and secreted on demand rather than stored within adrenal cortical cells?
Which drug can block the epithelial sodium channel (ENaC) proteins and thus impact aldosterone's function?
Which drug can block the epithelial sodium channel (ENaC) proteins and thus impact aldosterone's function?
What type of receptors do steroid hormones like aldosterone interact with to affect gene expression?
What type of receptors do steroid hormones like aldosterone interact with to affect gene expression?
What is a common result of adrenal androgen hypersecretion in adult females?
What is a common result of adrenal androgen hypersecretion in adult females?
What does primary adrenocortical insufficiency primarily affect?
What does primary adrenocortical insufficiency primarily affect?
Which symptom is most life-threatening in primary adrenocortical insufficiency?
Which symptom is most life-threatening in primary adrenocortical insufficiency?
What is the major hormone produced by the adrenal medulla?
What is the major hormone produced by the adrenal medulla?
What condition is primarily caused by a defect in the cortisol pathway?
What condition is primarily caused by a defect in the cortisol pathway?
What effect do catecholamines have during the fight-or-flight response?
What effect do catecholamines have during the fight-or-flight response?
What is a primary treatment for adrenal cortical insufficiency?
What is a primary treatment for adrenal cortical insufficiency?
In infants, what is often observed with adrenal androgen hypersecretion?
In infants, what is often observed with adrenal androgen hypersecretion?
Which of the following occurs as a consequence of excess ACTH in primary adrenocortical insufficiency?
Which of the following occurs as a consequence of excess ACTH in primary adrenocortical insufficiency?
What metabolic effect does adrenaline primarily have during stress?
What metabolic effect does adrenaline primarily have during stress?
What primary metabolic function does cortisol serve during acute stress?
What primary metabolic function does cortisol serve during acute stress?
What is the impact of glucocorticoid therapy on the body's immune system?
What is the impact of glucocorticoid therapy on the body's immune system?
How does cortisol affect the reproductive axis at the hypothalamus level?
How does cortisol affect the reproductive axis at the hypothalamus level?
What role does ACTH play concerning the adrenal cortex?
What role does ACTH play concerning the adrenal cortex?
What physiological effect occurs in response to stress on cortisol secretion?
What physiological effect occurs in response to stress on cortisol secretion?
Which of the following describes the feedback control loop in cortisol secretion?
Which of the following describes the feedback control loop in cortisol secretion?
When is cortisol's plasma concentration generally highest throughout the day?
When is cortisol's plasma concentration generally highest throughout the day?
What happens to the corticoid-secreting cells during prolonged glucocorticoid therapy?
What happens to the corticoid-secreting cells during prolonged glucocorticoid therapy?
How does the secretion of adrenal sex hormones change from puberty to the age of 60?
How does the secretion of adrenal sex hormones change from puberty to the age of 60?
What physiological effect does DHEA primarily have in females?
What physiological effect does DHEA primarily have in females?
Which statement accurately describes the feedback mechanism related to ACTH and adrenal hormones?
Which statement accurately describes the feedback mechanism related to ACTH and adrenal hormones?
What is a potential cause of primary hyperaldosteronism?
What is a potential cause of primary hyperaldosteronism?
What characterizes the relationship between DHEA levels and age?
What characterizes the relationship between DHEA levels and age?
What characterizes the production of steroid hormones like aldosterone in adrenal cortical cells?
What characterizes the production of steroid hormones like aldosterone in adrenal cortical cells?
Which factor prevents bound hormones from entering cells or being excreted?
Which factor prevents bound hormones from entering cells or being excreted?
What effect does the binding of free hormones to their receptors initiate?
What effect does the binding of free hormones to their receptors initiate?
What is the primary long-term role of aldosterone in the body?
What is the primary long-term role of aldosterone in the body?
What characterizes the action of aldosterone regarding extracellular fluid (ECF) volume?
What characterizes the action of aldosterone regarding extracellular fluid (ECF) volume?
How does the adrenal cortex regulate the daily production of cortisol?
How does the adrenal cortex regulate the daily production of cortisol?
What could result from excessive loss of sodium due to the absence of aldosterone?
What could result from excessive loss of sodium due to the absence of aldosterone?
Which statement accurately describes the method by which steroid hormones, such as DHEA, affect cellular functioning?
Which statement accurately describes the method by which steroid hormones, such as DHEA, affect cellular functioning?
What is the primary trigger for the secretion of aldosterone from the adrenal cortex?
What is the primary trigger for the secretion of aldosterone from the adrenal cortex?
Which mechanism contributes to the aldosterone escape response?
Which mechanism contributes to the aldosterone escape response?
How does chronic elevated ACTH affect aldosterone production?
How does chronic elevated ACTH affect aldosterone production?
What indirect effect does Atrial Natriuretic Peptide (ANP) have on aldosterone secretion?
What indirect effect does Atrial Natriuretic Peptide (ANP) have on aldosterone secretion?
What physiological occurrence primarily helps in regulating blood pressure in response to aldosterone levels?
What physiological occurrence primarily helps in regulating blood pressure in response to aldosterone levels?
What action does cortisol have on glucose metabolism during fasting?
What action does cortisol have on glucose metabolism during fasting?
What role does rising potassium levels (K+) play in the secretion of aldosterone?
What role does rising potassium levels (K+) play in the secretion of aldosterone?
Which of the following is NOT a characteristic of the aldosterone escape response?
Which of the following is NOT a characteristic of the aldosterone escape response?
What factor is most life-threatening in primary adrenocortical insufficiency?
What factor is most life-threatening in primary adrenocortical insufficiency?
In adult females, which characteristic is commonly associated with adrenal androgen hypersecretion?
In adult females, which characteristic is commonly associated with adrenal androgen hypersecretion?
Which of the following best describes the adrenal medulla's primary function?
Which of the following best describes the adrenal medulla's primary function?
What symptoms are associated with adrenal androgen hypersecretion in prepubertal males?
What symptoms are associated with adrenal androgen hypersecretion in prepubertal males?
Which condition is characterized by a defect in the cortisol pathway leading to hyperandrogenism?
Which condition is characterized by a defect in the cortisol pathway leading to hyperandrogenism?
What is the primary metabolic effect of adrenaline on the body during stress?
What is the primary metabolic effect of adrenaline on the body during stress?
Which symptom results from excessive adrenal cortex ACTH secretion due to low cortisol levels?
Which symptom results from excessive adrenal cortex ACTH secretion due to low cortisol levels?
During the fight-or-flight response, adrenaline has which physiological effect?
During the fight-or-flight response, adrenaline has which physiological effect?
What type of adrenal insufficiency results solely from insufficient ACTH secretion?
What type of adrenal insufficiency results solely from insufficient ACTH secretion?
Which treatment approach is commonly used for managing primary adrenocortical insufficiency?
Which treatment approach is commonly used for managing primary adrenocortical insufficiency?
Which symptom is least likely to be associated with secondary hyperaldosteronism?
Which symptom is least likely to be associated with secondary hyperaldosteronism?
Which of the following is NOT a mechanism that can lead to Cushing's syndrome?
Which of the following is NOT a mechanism that can lead to Cushing's syndrome?
What characteristic physical change is commonly associated with Cushing's syndrome?
What characteristic physical change is commonly associated with Cushing's syndrome?
Which of the following hormonal imbalances is directly related to high levels of glucocorticoids?
Which of the following hormonal imbalances is directly related to high levels of glucocorticoids?
Which of the following symptoms is particularly indicative of excessive protein breakdown associated with Cushing's syndrome?
Which of the following symptoms is particularly indicative of excessive protein breakdown associated with Cushing's syndrome?
Which condition is characterized by increased cortisol levels due to adrenal cortex adenomas?
Which condition is characterized by increased cortisol levels due to adrenal cortex adenomas?
What metabolic consequence can result from excessive glucocorticoid levels?
What metabolic consequence can result from excessive glucocorticoid levels?
Which symptom signifies mineralocorticoid effects due to elevated glucocorticoid levels in a patient with Cushing's syndrome?
Which symptom signifies mineralocorticoid effects due to elevated glucocorticoid levels in a patient with Cushing's syndrome?
Flashcards
Primary Hyperaldosteronism/Conn's Syndrome
Primary Hyperaldosteronism/Conn's Syndrome
A condition where the adrenal gland produces too much aldosterone, a hormone that regulates blood pressure and electrolyte balance.
Secondary Hyperaldosteronism
Secondary Hyperaldosteronism
A condition where the adrenal gland produces too much aldosterone due to an overactive RAAS (renin-angiotensin-aldosterone system).
Adrenogenital Syndrome
Adrenogenital Syndrome
A rare genetic disorder where the adrenal gland produces too much cortisol and androgen, leading to symptoms like weight gain, high blood pressure, and changes in appearance.
Addison's Disease (Primary Adrenocortical Insufficiency)
Addison's Disease (Primary Adrenocortical Insufficiency)
Signup and view all the flashcards
Secondary Adrenocortical Insufficiency
Secondary Adrenocortical Insufficiency
Signup and view all the flashcards
Aldosterone
Aldosterone
Signup and view all the flashcards
Aldosterone Escape Response
Aldosterone Escape Response
Signup and view all the flashcards
Atrial Natriuretic Peptide (ANP)
Atrial Natriuretic Peptide (ANP)
Signup and view all the flashcards
Direct Stimulation of Adrenal Cortex by Rising Potassium
Direct Stimulation of Adrenal Cortex by Rising Potassium
Signup and view all the flashcards
ACTH (Adrenocorticotropic Hormone)
ACTH (Adrenocorticotropic Hormone)
Signup and view all the flashcards
Angiotensin II
Angiotensin II
Signup and view all the flashcards
Renin-Angiotensin-Aldosterone System (RAAS)
Renin-Angiotensin-Aldosterone System (RAAS)
Signup and view all the flashcards
Cortisol
Cortisol
Signup and view all the flashcards
Cortisol's Catabolic Effect
Cortisol's Catabolic Effect
Signup and view all the flashcards
Cortisol's Impact on Reproduction
Cortisol's Impact on Reproduction
Signup and view all the flashcards
Cortisol's Anti-inflammatory Role
Cortisol's Anti-inflammatory Role
Signup and view all the flashcards
Glucocorticoid Therapy
Glucocorticoid Therapy
Signup and view all the flashcards
Hypothalamus-Pituitary-Adrenal (HPA) Axis
Hypothalamus-Pituitary-Adrenal (HPA) Axis
Signup and view all the flashcards
ACTH's Role in Cortisol Production
ACTH's Role in Cortisol Production
Signup and view all the flashcards
Cortisol's Diurnal Rhythm
Cortisol's Diurnal Rhythm
Signup and view all the flashcards
Stress and Cortisol Secretion
Stress and Cortisol Secretion
Signup and view all the flashcards
Cushing's Syndrome
Cushing's Syndrome
Signup and view all the flashcards
Cushing's Disease
Cushing's Disease
Signup and view all the flashcards
Ectopic ACTH Secretion
Ectopic ACTH Secretion
Signup and view all the flashcards
Hypothalamic Dysfunction
Hypothalamic Dysfunction
Signup and view all the flashcards
Adrenal Cortex Adenoma
Adrenal Cortex Adenoma
Signup and view all the flashcards
Exogenous Corticosteroids
Exogenous Corticosteroids
Signup and view all the flashcards
Gluconeogenesis
Gluconeogenesis
Signup and view all the flashcards
Dehydroepiandrosterone (DHEA)
Dehydroepiandrosterone (DHEA)
Signup and view all the flashcards
Adrenocortical Hormones
Adrenocortical Hormones
Signup and view all the flashcards
Plasma Protein Binding of Adrenocortical Hormones
Plasma Protein Binding of Adrenocortical Hormones
Signup and view all the flashcards
Hormone-Receptor Interaction
Hormone-Receptor Interaction
Signup and view all the flashcards
Aldosterone Function
Aldosterone Function
Signup and view all the flashcards
Stimulators of Aldosterone Production
Stimulators of Aldosterone Production
Signup and view all the flashcards
Spironolactone
Spironolactone
Signup and view all the flashcards
Adrenal Androgen Hypersecretion
Adrenal Androgen Hypersecretion
Signup and view all the flashcards
Adrenal Estrogen Hypersecretion
Adrenal Estrogen Hypersecretion
Signup and view all the flashcards
Addison's Disease
Addison's Disease
Signup and view all the flashcards
Primary Hyperaldosteronism
Primary Hyperaldosteronism
Signup and view all the flashcards
Adrenal Medulla
Adrenal Medulla
Signup and view all the flashcards
Chromaffin cells
Chromaffin cells
Signup and view all the flashcards
Adrenaline
Adrenaline
Signup and view all the flashcards
Noradrenaline
Noradrenaline
Signup and view all the flashcards
Study Notes
Adrenal Glands Introduction
- The human body needs a well-regulated extracellular environment
- Adrenal glands play a vital role in maintaining this environment
- Two adrenal glands, each weighing approximately 4 grams
- Each gland is made up of two endocrine organs: the adrenal cortex (80%) and the adrenal medulla (20%)
- The adrenal cortex develops from mesoderm, while the adrenal medulla develops from neural crest
- Each gland secretes hormones belonging to different chemical categories
- These hormones differ in function, mechanism of action, and regulation
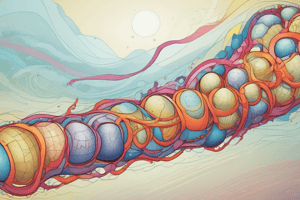
Adrenal Cortex Introduction
- The adrenal cortex is made up of three layers: Zona glomerulosa, Zona fasciculata and Zona reticularis
- The cortex produces adrenocortical hormones. The distribution of enzymes differs throughout the layers
- Mineralocorticoids: Primarily aldosterone (Zona glomerulosa)
- Glucocorticoids: Primarily cortisol (Zona fasciculata and Zona reticularis)
- Sex hormones: Primarily DHEA (Zona fasciculata and Zona reticularis), produced in greater abundance in the gonads
Adrenocortical Hormones Introduction
- Adrenocortical cells release only small amounts of aldosterone, cortisol, and DHEA at any given time
- The cells produce and release these hormones on demand rather than storing them
- These hormones are lipophilic and diffuse into the bloodstream after synthesis
- Steroid hormones are extensively bound to plasma proteins such as CBG and albumin, which prevents hormone entry into cells and excretion
- Unbound hormones interact with cell receptors, and are then cleared from the bloodstream
- Bound hormone dissociates from the binding protein, replenishing the pool of circulating free hormone
- Free hormone binding makes a hormone-receptor complex move to the nucleus and bind to complementary hormone response elements on DNA
- This process initiates gene transcription and the synthesis of new proteins
Average Daily Production of Hormones by Adrenal Cortex
- The average daily production amounts for hormones are different
- Cortisol: 20 mg/day
- Aldosterone: 0.1 mg/day
- DHEA: 30 mg/day
- Hormone amounts can vary based on physiological state
Aldosterone Function
- Aldosterone works in the distal and collecting tubules of the kidney
- It regulates sodium and potassium elimination during urine formation
- It promotes sodium retention, which secondarily increases the osmotic retention of water, expanding ECF volume
- Aldosterone is essential for long-term blood pressure regulation
Aldosterone Production and Secretion
- Factors stimulating renin-angiotensin-aldosterone system (RAAS) activation are related to a decrease in sodium and drop in blood pressure
- Angiotensin II is a potent stimulator of aldosterone production
- Other stimulating factors include:
- Rise in plasma potassium which depolarizes glomerulosa cells, opens voltage-sensitive calcium channels, and stimulates aldosterone production
- Acute elevated ACTH
- Inhibitory factors include:
- Atrial natriuretic peptide (ANP), which is secreted by the heart, acts directly on zona glomerulosa cells to inhibit aldosterone production
- Chronic elevated ACTH
- Aldosterone escape response is a physiological process to limit fluid retention and prevent hypertension despite high levels of aldosterone
Cortisol Function
- Metabolic: Increases blood glucose, at the expense of protein and fat, in response to fasting, inhibits glucose uptake by many tissues (especially sparing the brain), and increases hepatic gluconeogenesis (particularly important to replenish hepatic glycogen stores between meals)
- Metabolic: Stimulates protein degradation, especially in the muscles, providing amino acids for gluconeogenesis, and facilitates lipolysis (increasing free fatty acids and glycerol)
- Permissive Actions: Increases the responsiveness of cells to glucagon and catecholamines.
- Stress Adaptation: In acute situations, cortisol's catabolic mechanisms provide energy to the body. Reproduction involves substantial energy expenditure, and cortisol reduces reproductive axis function at the hypothalamus, pituitary, and gonads..
- Anti-inflammatory & Immunosuppressive Effects: Cortisol holds immune responses in balance, excessive responses can cause harm.
- Glucocorticoid Therapy / Rheumatoid Arthritis & Prevention of Organ Transplant Rejection: Used only when warranted. Suppresses the body’s immune system but involves troublesome side effects and potentially irreversible atrophy of cortisol-secreting cells.
Cortisol Secretion
- ACTH stimulates growth and secretory output of the zona fasciculata and zona reticularis
- ACTH secretion is controlled by hypothalamic CRH
- Feedback mechanisms using cortisol inhibit ACTH and CRH
- Diurnal rhythm and stress influence hypothalamic CRH secretion
Adrenal Cortex & Sex Hormones
- Both sexes produce androgens and estrogens in the adrenal cortex although, normally in smaller quantities
- Under normal conditions, these levels are not high enough to induce significant effects, but DHEA is the adrenal sex hormone with biological significance
- Males have very high testosterone levels so adrenal androgens have limited significance
- In females, DHEA is a precursor for intracellular estrogen and androgen production, hence important for androgen-dependent processes
Adrenal Sex Hormones Secretion
- ACTH controls adrenal secretion of sex hormones, but adrenal sex hormones do not feed back on the hypothalamus-pituitary-adrenal (HPA) axis
- DHEA inhibits gonadotropin-releasing hormone (not CRH)
- There is a surge of adrenal androgen secretion at puberty, peaking between 25-30 years of age. Levels decline later in life.
Disorders of the Adrenal Cortex
- Many disorders of adrenal cortex function exist, but are generally uncommon
- Hormone levels can be too high or too low
- Specific disorders for discussion include:
- Aldosterone hypersecretion
- Cortisol hypersecretion (Cushing's syndrome)
- Adrenogenital syndrome
- Adrenocortical insufficiency
Aldosterone Hypersecretion Causes & Symptoms
- Causes:
- Primary hyperaldosteronism (Conn's syndrome) - hypersecreting adrenal tumor
- Secondary - inappropriately high activity of RAAS (renin-angiotensin-aldosterone system).
- Symptoms:
- Increased whole body sodium, fluid, and circulating blood volume
- Excessive potassium depletion (hypokalemia)
- Weakness and fatigue
- Hypertension (high blood pressure)
Cortisol Hypersecretion (Cushing Syndrome)
- Causes:
- Pituitary adenomas secreting excessive ACTH leading to adrenal hyperplasia and excess cortisol secretion
- Ectopic ACTH secretion, e.g from tumors (especially lung tumors)
- Adrenal cortical adenomas (tumors)
- Exogenous corticosteroid use
- Symptoms
- Related to the exaggerated physiological effects of glucocorticoids
- Excessive gluconeogenesis, hyperglycemia (high blood glucose) and glucosuria (glucose in urine)
- Adrenal diabetes
- Protein shortage
- Body fat deposition (characteristic locations like abdomen, above shoulder blades, face)
- Muscle wasting
- Tendency to weight gain
- Muscle weakness and fatigue
- Other skin, blood vessel and skeletal effects
- Related to the exaggerated physiological effects of glucocorticoids
Adrenogenital Syndrome
- Adrenal androgen hypersecretion, a masculinizing condition seen more frequently than excess adrenal estrogen secretion
- Symptoms depend on the age and sex of the individual when hyperactivity begins
- Cause: Inherited defect in the cortisol pathway
- Symptoms in newborn females and adult females include:
- Infants manifest male-type external genitalia. This can become a major cause of female pseudohermaphroditism.
- Hirsutism (excessive hair growth) in adult females
- Other male secondary sexual characteristics
- Symptoms in Prepubertal males and adult males include:
- Precocious pseudopuberty (abnormally early puberty)
- Males may also show very high testosterone levels
Adrenocortical Insufficiency
- One gland becomes non-functional/removed, sometimes the other can take over via hypertrophy/hyperplasia
- Both glands must be affected for the disease to manifest
- Primary Adrenocortical Insufficiency (Addison's Disease):
- All layers of the cortex under-secrete
- Aldosterone and cortisol levels are deficient
- Cause: Autoimmune destruction of the adrenal cortex
- Secondary Adrenocortical Insufficiency:
- Pituitary or hypothalamic abnormality
- Insufficient ACTH (adrenocorticotropic hormone) secretion
- Only cortisol is deficient
Primary Adrenocortical Insufficiency (Addison's Disease) Symptoms
- Aldosterone deficiency
- Most life-threatening
- Primarily loss of adrenal function develops slowly
- Retention of potassium (hyperkalemia) reducing loss in the urine
- Disturbs cardiac rhythm
- Sodium depletion (hyponatremia)
- Excessive urinary loss of sodium
- Reduced ECF blood volume
- Low blood pressure (hypotension)
Primary Adrenocortical Insufficiency/Addison's Disease Symptoms & Treatment
- Cortisol deficiency
- Reduced response to stress
- Hypoglycemia (Low blood glucose)
- Reduced gluconeogenesis
- Darkening of the skin (hyperpigmentation)
- Excessive ACTH resulting from the absence of cortisol
- ACTH binds to related α-MSH receptors rather than intended receptors
- Combined lack of glucocorticoid and mineralocorticoid can lead to life-threatening complications
- Treatment:
- Reversal of hypotension, electrolyte abnormalities
- Administration of saline, dextrose in saline
- Administration of Cortisol and mineralocorticoid replacement therapy
Adrenal Medulla Introduction
- The adrenal medulla consists of modified postganglionic sympathetic neurons called chromaffin cells
- Chromaffin cells do not have axonal fibers terminating on effector organs
- The cells release adrenaline (80%) and noradrenaline directly into the circulatory system after preganglionic stimulation
- Adrenaline is produced exclusively by the adrenal medulla; noradrenaline is mostly produced by sympathetic postganglionic fibers
Function of Catecholamines: Effects on Organ Systems
- The sympathetic nervous system and adrenomedullary adrenaline participate in the "fight-or-flight" response, increasing heart rate and cardiac output, blood pressure, and reducing digestive activity, and inhibiting bladder emptying.
- Adrenaline and noradrenaline dilate coronary and skeletal muscles blood vessels and dilate airways.
Function of Catecholamines: Metabolic Effects
- Catecholamines prompt the mobilization of stored carbohydrates and fats to provide energy for muscular work. These include hepatic gluconeogenesis and glycogenolysis, muscle glycogenolysis, lipolysis, and the inhibition of insulin release with concurrent stimulation of glucagon release to provide adequate fuel.
Function of Catecholamines: Other Effects
- Catecholamines promote arousal, increased alertness, and sweating to reduce body temperature
- Catecholamine secretion is triggered by sympathetic input to the gland, in response to injury, anger, anxiety, pain, cold, strenuous exercise, and hypoglycemia.
- Chromaffin cells release hormones into the circulatory system when stimulated
Summary: Adrenal Hormones
- Adrenal Cortex: Regulates sodium, potassium, and blood pressure via RAAS; cortisol increases glucose and has anti-inflammatory actions; abnormalities can lead to Cushing's syndrome. DHEA is a significant androgen precursor.
- Adrenal Medulla: Secretes adrenaline and noradrenaline (catecholamines); these hormones regulate stress responses, increasing heart rate, blood pressure and glycogenolysis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.