Podcast
Questions and Answers
What is the primary aim of Phase I in the Damage Control Surgery process?
What is the primary aim of Phase I in the Damage Control Surgery process?
- Correct anatomy, close abdomen
- Stop bleeding, prevent contamination (correct)
- Resuscitate the patient
- Identify patients for DCS
Early Total Care (ETC) allows for definitive management of injuries to be shifted to Damage Control Surgery (DCS) if the patient remains stable.
Early Total Care (ETC) allows for definitive management of injuries to be shifted to Damage Control Surgery (DCS) if the patient remains stable.
False (B)
List two components of the Terrible Triad in Damage Control Surgery.
List two components of the Terrible Triad in Damage Control Surgery.
Hypothermia, Acidosis, Coagulopathy
What is a disadvantage of using active space in abdominal trauma assessment?
What is a disadvantage of using active space in abdominal trauma assessment?
A patient presenting with peritonitis may require an _________ for diverting stoma or colostomy.
A patient presenting with peritonitis may require an _________ for diverting stoma or colostomy.
Exploratory laparotomy is always needed if peritonitis is present.
Exploratory laparotomy is always needed if peritonitis is present.
What should be done if a pseudoaneurysm or arterial blush is detected on a CT scan?
What should be done if a pseudoaneurysm or arterial blush is detected on a CT scan?
Match the following phases of Damage Control Surgery with their descriptions:
Match the following phases of Damage Control Surgery with their descriptions:
If a person has a peritoneal breach, signs may include ____, rebound tenderness, and rigidity.
If a person has a peritoneal breach, signs may include ____, rebound tenderness, and rigidity.
Match the following symptoms with their meanings in the context of penetrating abdominal trauma assessment:
Match the following symptoms with their meanings in the context of penetrating abdominal trauma assessment:
What is the primary goal of the Pringle's maneuver during surgery?
What is the primary goal of the Pringle's maneuver during surgery?
If bleeding continues after performing the Pringle's maneuver, the source of bleeding is likely from the Portal vein.
If bleeding continues after performing the Pringle's maneuver, the source of bleeding is likely from the Portal vein.
What are the contents that are compressed during the Pringle's maneuver?
What are the contents that are compressed during the Pringle's maneuver?
The Pringle's maneuver typically involves compressing the hepatic pedicle for _____ minutes.
The Pringle's maneuver typically involves compressing the hepatic pedicle for _____ minutes.
What is the management for a transverse tear in the mesentery?
What is the management for a transverse tear in the mesentery?
Match the potential complications with their corresponding type:
Match the potential complications with their corresponding type:
A duodenal hematoma is considered the most severe type of duodenal injury.
A duodenal hematoma is considered the most severe type of duodenal injury.
What is the most important prognostic factor in pancreatic injury?
What is the most important prognostic factor in pancreatic injury?
In the case of a bile leak, the management involves ligating the ______ and repairing over a T-tube.
In the case of a bile leak, the management involves ligating the ______ and repairing over a T-tube.
Match the following pancreatic injuries with their management strategies:
Match the following pancreatic injuries with their management strategies:
What imaging technique is used to monitor vascular injuries that may present with an arterial blush?
What imaging technique is used to monitor vascular injuries that may present with an arterial blush?
Active bleeding from a vascular injury does not show an increase in arterial blush in delayed imaging.
Active bleeding from a vascular injury does not show an increase in arterial blush in delayed imaging.
What is the recommended management for a patient with Grade IV splenic injury who is unstable?
What is the recommended management for a patient with Grade IV splenic injury who is unstable?
The complication of splenectomy characterized by amylase-rich secretions is called a __________.
The complication of splenectomy characterized by amylase-rich secretions is called a __________.
Match the following complications of splenectomy with their descriptions:
Match the following complications of splenectomy with their descriptions:
Which of the following is a common cause of blunt thoracic trauma?
Which of the following is a common cause of blunt thoracic trauma?
Tension pneumothorax is classified under life-threatening injuries during the initial survey.
Tension pneumothorax is classified under life-threatening injuries during the initial survey.
What is the primary investigation used to assess thoracic trauma?
What is the primary investigation used to assess thoracic trauma?
In cases of rib fractures, the most commonly fractured ribs during CPR are the ________ ribs.
In cases of rib fractures, the most commonly fractured ribs during CPR are the ________ ribs.
Match the following types of thoracic trauma with their associated injuries:
Match the following types of thoracic trauma with their associated injuries:
What is the increase in Intra-abdominal Pressure (IAP) that signifies Intra-abdominal Hypertension (IAH)?
What is the increase in Intra-abdominal Pressure (IAP) that signifies Intra-abdominal Hypertension (IAH)?
Abdominal Compartment Syndrome (ACS) occurs when the IAP is 15 mmHg or higher.
Abdominal Compartment Syndrome (ACS) occurs when the IAP is 15 mmHg or higher.
What urinary procedure is used to measure intra-abdominal pressure?
What urinary procedure is used to measure intra-abdominal pressure?
In order to assess renal function in abdominal trauma, there is a decrease in __________.
In order to assess renal function in abdominal trauma, there is a decrease in __________.
Match the following effects of intra-abdominal pressure elevation with their corresponding functions:
Match the following effects of intra-abdominal pressure elevation with their corresponding functions:
What is a positive result in a Diagnostic Peritoneal Lavage indicated by the presence of blood?
What is a positive result in a Diagnostic Peritoneal Lavage indicated by the presence of blood?
A positive Kehr sign is associated with splenic trauma.
A positive Kehr sign is associated with splenic trauma.
What is the minimum blood count of RBC per cubic millimeter that indicates a positive result in Diagnostic Peritoneal Lavage?
What is the minimum blood count of RBC per cubic millimeter that indicates a positive result in Diagnostic Peritoneal Lavage?
Fracture of the _____ ribs on the left side is an indication of splenic trauma.
Fracture of the _____ ribs on the left side is an indication of splenic trauma.
Match the grade of splenic trauma with its description:
Match the grade of splenic trauma with its description:
In blunt abdominal trauma, which organ is most likely to be injured?
In blunt abdominal trauma, which organ is most likely to be injured?
The eFAST procedure only assesses the abdominal cavity for free fluid.
The eFAST procedure only assesses the abdominal cavity for free fluid.
Name one advantage of using FAST in trauma assessment.
Name one advantage of using FAST in trauma assessment.
In cases of penetrating trauma, the order of organ injuries is often liver > _________.
In cases of penetrating trauma, the order of organ injuries is often liver > _________.
Match the imaging techniques with their primary usage:
Match the imaging techniques with their primary usage:
What is the primary focus of the FAST procedure?
What is the primary focus of the FAST procedure?
Gunshot wounds primarily affect the small intestine before the liver.
Gunshot wounds primarily affect the small intestine before the liver.
The site targeted in the left upper quadrant ultrasound is primarily around the ________.
The site targeted in the left upper quadrant ultrasound is primarily around the ________.
What is the most common encapsulated bacteria responsible for OPSI?
What is the most common encapsulated bacteria responsible for OPSI?
OPSI is more frequently observed in adults than children.
OPSI is more frequently observed in adults than children.
What is the time frame in which OPSI is commonly seen after splenectomy?
What is the time frame in which OPSI is commonly seen after splenectomy?
The vaccination for Pneumococcal should be repeated every ___ years.
The vaccination for Pneumococcal should be repeated every ___ years.
Match the grades of liver trauma with their features:
Match the grades of liver trauma with their features:
Which of the following vaccinations needs to be administered yearly?
Which of the following vaccinations needs to be administered yearly?
A laceration classified as Grade 3 involves active bleeding breaching the liver parenchyma into the peritoneum.
A laceration classified as Grade 3 involves active bleeding breaching the liver parenchyma into the peritoneum.
What happens to the grade classification for liver trauma if multiple injuries are present?
What happens to the grade classification for liver trauma if multiple injuries are present?
Flashcards are hidden until you start studying
Study Notes
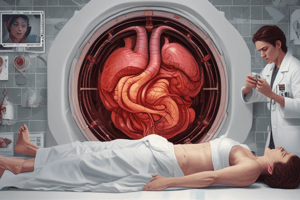
Abdominal Trauma Assessment
- Active space: a tool used to detect free blood in the abdomen, but it has limitations. It cannot reliably detect free blood less than 100 ml, does not identify hollow viscous injuries, and is not accurate for retroperitoneal assessment.
- Blunt abdominal trauma: Patients should be examined. If there is peritonitis or hemodynamic instability, an exploratory laparotomy is needed. If there is no peritonitis and no hemodynamic instability, an abdominal CT scan is performed.
- Hollow organ injury: If present, proceed to exploratory laparotomy. If not, assess for solid organ injury.
- Solid organ injury: If present, proceed to exploratory laparotomy or diagnostic laparoscopy. If not, manage other injuries.
- Pseudoaneurysm or arterial blush: In CT scan, if present refer to interventional radiology for evaluation. If not, opt for non-operative management.
- Penetrating abdominal trauma: Never remove sharp objects from the body.
- Penetrating abdominal trauma -- superficial to peritoneum: Conduct a local examination. If a peritoneal breach is suspected, perform a midline laparotomy (no further imaging needed).
- Colon & rectal injury: This can lead to peritonitis. Emergency laparotomy may require diverting stoma/colostomy or a Hartman procedure.
- Early Total care (ETC): Definitive management of injuries within 36 hours. If the patient deteriorates, shift to damage control surgery (DCS).
- Damage control surgery (DCS): Simultaneous resuscitation with early rapid life and limb-saving surgery. Definitive surgery is delayed until the patient stabilizes.
- Terrible Triad: Hypothermia, acidosis, coagulopathy.
- ETC: Stable haemodynamics, no hypoxaemia/hypercapnia, no acidosis, normal coagulation.
- Phases of DCS (ACS guidelines): Phase 0: Resuscitate, phase I: Emergency laparotomy, phase II: Correction of physiology, phase III: Re-laparotomy.
- Stage 1 Abdominal Compartment Syndrome: Can be caused by massive burns or bowel obstruction.
- Abdominal trauma complications: Bleeding, bile leak, liver abscess, strictures in the common bile duct, AV malformations, vascular injury to the portal vein.
- Mesenteric injury: Longitudinal tear: repair the tear. Transverse tear: resection and anastomosis.
- Duodenal and pancreatic injury: Duodenal hematoma: keep the patient NPO (nothing by mouth) and on bowel rest. Pancreatic injury: Injury to the main pancreatic duct is the most significant prognostic factor. Duodenal perforation: features of peritonitis, X-ray shows gas under the diaphragm. Management: Omental patch repair.
- Injury to the main pancreatic duct: If yes, proceed with conservative management: Body and tail of the pancreas: Distal pancreatectomy. Head and neck of the pancreas: Begger's procedure.
- Pringle's maneuver: This procedure involves compressing the hepatic pedicle for 15-20 minutes, to control bleeding and locate its source.
- Packing procedure: Cut right and left triangular ligaments, separate the liver from the diaphragm, place mops above and below the liver. This is used to control bleeding for 24-48 hours by tamponading.
- Trauma Management - Vascular Injury:
- Grade I & II: Monitor vitals, hematocrit, and do serial 24-hour CECT. If contrast blush increases, perform angioembolization.
- Grade III: Manage as per Grade I & II. If unstable, manage as per Grade IV & V.
- Grade IV & V: If FAST positive, perform laparotomy. Splenectomy is often necessary.
- Splenectomy complications: Hemorrhage, pancreatic fistula, hematological changes.
- Thoracic trauma: Most common in polytrauma patients. The most common cause of death.
- Blunt thoracic trauma: Tracheobronchial injury. Penetrating thoracic trauma: Hemothorax, pulmonary laceration.
- Life-threatening thoracic trauma: Airway obstruction, tracheobronchial tree injury, tension pneumothorax, open pneumothorax, massive hemothorax, cardiac tamponade, traumatic circulatory arrest.
- Thoracic trauma investigation: Chest X-ray, eFAST, pulse oximetry.
- Rib fractures and flail chest: The most common type of thoracic trauma. Usually caused by CPR.
- Intra-abdominal pressure measurement: Insert saline via Foley catheter to measure bladder pressure (indicative of abdominal pressure).
- Intra-abdominal pressure grades: Intra-abdominal hypertension (IAH): IAP > 12 mmHg. Abdominal compartment syndrome (ACS): 20 mmHg with new organ dysfunction.
- Intra-abdominal pressure effects: ↓ GFR, ↓ venous return, ↓ SBP, ↓ Cardiac output, ↓ Urine output, ↓ Inspiratory volumes & capacities, ↓ visceral perfusion, ↑ intracranial tension.
- Retroperitoneal trauma: Involves the kidney, ureter, renal vessels.
- Retroperitoneal trauma management: In unstable cases: Angiogram. Stable cases: CECT. Unstable cases: Single shot IV urogram. Pelvic structures: most commonly injured zone.
- Left lower lobe atelectasis/pneumonia: Decreased expansion of the left side of the chest. OPSI (Opportunistic/Overwhelming Post Splenectomy Infection)
- OPSI: Etiology: Encapsulated bacteria (Pneumococcus, meningococcus, H. influenzae). Most frequent in children. Commonly seen within the first 2 years after splenectomy. High mortality rates are often associated with hematological conditions and trauma.
- OPSI prevention: Vaccination with pneumococcal, meningococcal, H. influenzae, and annual influenza vaccine.
- Liver trauma grades: Grades 1-5 classified based on Hematoma, Laceration, and Vascular injury. Advance one grade for multiple injuries up to grade 111.
- Diagnostic Peritoneal Lavage (DPL): Used when FAST is not available. Interpretation: Decompress stomach and bladder. Insert a needle and aspirate just below the umbilicus.
- DPL Results: Positive if blood > 10cc. Other positive indicators: RBC > 1 lakh/cumm, WBC > 500/cumm, amylase > 175 IU/L, fecal content present.
- Splenic trauma: Indications for splenic trauma: Fracture of 9–11th ribs on the left side, bruising of the left lower chest wall, Positive Kehr sign.
- Splenic trauma grades: Grades 1-5 classified based on subcapsular hematoma and vascular injury.
- Abdominal trauma: Mechanism of injury: Spleen is most common overall, liver most common in blunt trauma.
- Blunt abdominal trauma: Hemodynamically stable patients: Perform FAST scan. Hemodynamically unstable patients: Perform FAST scan and CECT.
- Management: Midline laparotomy, FAST scan in the ER.
- FAST Procedure: Epigastrium, right upper quadrant, left upper quadrant, suprapubic.
- eFAST: FAST + assessment of the thoracic cavity.
- Advantages: FAST detects free fluid in the abdomen or pericardium.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.