Podcast
Questions and Answers
What is a common immediate complication of a bowel obstruction?
What is a common immediate complication of a bowel obstruction?
- Infection
- Bowel perforation
- Dehydration (correct)
- Hemorrhage
Which diagnostic study is NOT typically used for a bowel obstruction?
Which diagnostic study is NOT typically used for a bowel obstruction?
- CBC
- MRI (correct)
- Colonoscopy
- Abdominal x-rays
Which symptom is characteristic of a bowel obstruction?
Which symptom is characteristic of a bowel obstruction?
- Black, tarry stools
- Constant severe pain
- Wavelike abdominal crampy pain (correct)
- Bright red blood in stool
What should NOT be done in the case of abdominal evisceration?
What should NOT be done in the case of abdominal evisceration?
For penetrating injuries of the abdomen, which action is essential for care?
For penetrating injuries of the abdomen, which action is essential for care?
Which of the following is classified as a hollow organ?
Which of the following is classified as a hollow organ?
During an abdominal assessment, which of the following findings is considered abnormal?
During an abdominal assessment, which of the following findings is considered abnormal?
What is the correct order of techniques for physical abdominal assessment?
What is the correct order of techniques for physical abdominal assessment?
Deep palpation during an abdominal assessment should be performed when which of the following is present?
Deep palpation during an abdominal assessment should be performed when which of the following is present?
Which abnormal percussion sound may indicate the presence of intra-abdominal tumors?
Which abnormal percussion sound may indicate the presence of intra-abdominal tumors?
Which abdominal assessment technique involves listening to bowel sounds?
Which abdominal assessment technique involves listening to bowel sounds?
Which of the following factors is NOT typically included in a GI history assessment?
Which of the following factors is NOT typically included in a GI history assessment?
Which of the following is an indicator of possible ascites during percussion?
Which of the following is an indicator of possible ascites during percussion?
Which sign is indicative of ruptured spleen associated with left shoulder pain during abdominal palpation?
Which sign is indicative of ruptured spleen associated with left shoulder pain during abdominal palpation?
What is the recommended non-invasive tool for rapid confirmation of an intra-abdominal injury in a stable patient?
What is the recommended non-invasive tool for rapid confirmation of an intra-abdominal injury in a stable patient?
Which of the following signs is associated with retroperitoneal bleeding or pancreatitis that presents as flank ecchymosis?
Which of the following signs is associated with retroperitoneal bleeding or pancreatitis that presents as flank ecchymosis?
After what percentage of blood volume loss do clinical signs of shock typically occur in adults with penetrating abdominal wounds?
After what percentage of blood volume loss do clinical signs of shock typically occur in adults with penetrating abdominal wounds?
In which scenario would a patient likely exhibit a positive Murphy’s sign?
In which scenario would a patient likely exhibit a positive Murphy’s sign?
What percentage of blunt or penetrating abdominal trauma cases typically involve liver injuries?
What percentage of blunt or penetrating abdominal trauma cases typically involve liver injuries?
Which of the following is NOT a clinical manifestation of hepatic injury?
Which of the following is NOT a clinical manifestation of hepatic injury?
What does Balance’s sign indicate in a patient with suspected splenic rupture?
What does Balance’s sign indicate in a patient with suspected splenic rupture?
Which diagnostic aid is NOT commonly used for assessing hepatic injury?
Which diagnostic aid is NOT commonly used for assessing hepatic injury?
Which sign indicates the presence of periumbilical ecchymosis and is associated with blood in the abdomen?
Which sign indicates the presence of periumbilical ecchymosis and is associated with blood in the abdomen?
Patients with blunt abdominal trauma commonly have injuries to which internal organs?
Patients with blunt abdominal trauma commonly have injuries to which internal organs?
What is the primary purpose of gentle and shallow palpation during an abdominal examination?
What is the primary purpose of gentle and shallow palpation during an abdominal examination?
What is a common cause of bowel obstruction?
What is a common cause of bowel obstruction?
Which clinical sign involves pain in the right lower quadrant when palpating the left lower quadrant, suggesting appendicitis?
Which clinical sign involves pain in the right lower quadrant when palpating the left lower quadrant, suggesting appendicitis?
Upon auscultation of the abdomen, which finding would indicate early bowel obstruction?
Upon auscultation of the abdomen, which finding would indicate early bowel obstruction?
What symptom is characteristic of bowel obstruction?
What symptom is characteristic of bowel obstruction?
Which symptom is NOT commonly associated with cholecystitis?
Which symptom is NOT commonly associated with cholecystitis?
What is the preferred patient position for someone suspected of having appendicitis?
What is the preferred patient position for someone suspected of having appendicitis?
Which assessment is most indicative of appendicitis?
Which assessment is most indicative of appendicitis?
Which of the following laboratory studies would most likely be ordered for a diagnosis of cholecystitis?
Which of the following laboratory studies would most likely be ordered for a diagnosis of cholecystitis?
What symptom might suggest a complication from appendicitis?
What symptom might suggest a complication from appendicitis?
Which option best describes the primary cause of dehydration in pediatric patients?
Which option best describes the primary cause of dehydration in pediatric patients?
Which dietary recommendation is commonly suggested for a patient with cholecystitis?
Which dietary recommendation is commonly suggested for a patient with cholecystitis?
Recognizing the signs of which condition is vital to address dehydration in children due to GI issues?
Recognizing the signs of which condition is vital to address dehydration in children due to GI issues?
Study Notes
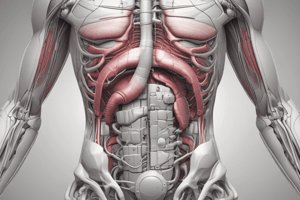
Abdominal Anatomy
- Hollow organs include the stomach, intestines, and bladder.
- Solid organs include the liver, spleen, kidneys, and pancreas.
GI & GU Assessment
- History:
- Chief complaint
- Signs and symptoms
- Risk factors
- Current and significant past medical history
- Medications
- Drug and alcohol use
- Allergies
- Physical Assessment:
- Inspection:
- Skin color
- Appearance of the abdomen (size, shape, color, symmetry, distention, protuberance, rash, scarring, pulsation)
- Patient positioning and expression
- Stool and urine character, odor, color, and presence of blood
- Auscultation:
- Bowel sounds in all four quadrants
- Friction rub over the liver and spleen
- Bruits over the abdominal aorta
- Percussion:
- Normal sounds:
- Dullness over solid organs and muscles
- Tympany over most portions of the abdominal cavity
- Abnormal sounds:
- Dullness may be caused by intra-abdominal tumors or masses
- Shifting dullness: may indicate the presence of ascites
- Normal sounds:
- Palpation:
- Gentle and shallow palpation while warning the patient and making them comfortable
- Palpate for:
- Rigidity
- Guarding
- Pain or tenderness
- Rebound tenderness
- Masses
- Hernias
- Inspection:
- Deep Palpation:
- Used to assess for liver and spleen enlargement
- Liver Palpation:
- Palpate the liver by placing the hand below the right costal margin and having the patient inhale deeply.
Acute Abdomen
- Inflammation of the peritoneum (abdominal lining)
- Signs and symptoms include:
- RUQ pain aggravated by deep breathing and increased WBC
- Referred pain to right scapula and shoulder
- Murphy's sign (inhibition of inspiration on RUQ palpation) and temperature
- Causes:
- Cholecystitis
- Appendicitis
- Peritonitis
Cholecystitis
- Inflammation of the gallbladder
- Signs and symptoms:
- Sudden onset of epigastric pain that radiates to the RUQ (especially following ingestion of fried or greasy foods)
- Localized pain on palpation with rebound tenderness
- Referred pain to the right scapula
- Anorexia
- Nausea and vomiting
- Low-grade fever (38°C)
- Jaundice
- Murphy's sign (inhibition of inspiration on RUQ palpation)
- Diagnostic studies:
- Ultrasound
- Abdominal CT
- Flat and upright abdominal x-rays
- CBC
- Interventions:
- NGT to LIS
- Intravenous fluids (LR or NS)
- Antibiotics
- Analgesics
- Antiemetics
- Possible surgery (cholecystectomy)
- Low-fat diet
Gastroenteritis
- Inflammation of the stomach and intestines
- Causes:
- Viral
- Bacterial
- Parasitic
- Protozoan
- Signs and symptoms:
- Crampy, colicky, abdominal pain
- Nausea and vomiting
- Diarrhea
- Hyperactive bowel sounds
- Diagnostic studies:
- Electrolytes
- Stool exam for blood
- Culture
- O&P (ova and parasite)
- Interventions:
- Hydration
Appendicitis
- Inflammation of the appendix
- Signs and symptoms:
- Pain that originates in the periumbilical area and then localizes in the RLQ
- Preferred position: supine with legs flexed
- Rovsing's sign: RLQ pain on palpation of LLQ
- Obturator sign: pain with flexion and internal rotation of the right thigh
- Psoas sign: pain with hyperextension of the right hip
- Loss of appetite (anorexia)
- Nausea and vomiting
- Fever and tachycardia
- RLQ guarding and pain with movement
- Rebound tenderness and abdominal rigidity (peritoneal sign) if ruptured
- Diagnostic aids:
- Serial CBCs (with left shift)
- Renal panel, hepatic panel, bone panel (50%)
Hepatic Injury
- Mechanism:
- Blunt or penetrating abdominal trauma
- Liver is injured in about 19% of blunt or penetrating abdominal trauma cases
- Signs and symptoms:
- Abdominal wall muscle spasm and rigidity
- Hypoactive or absent bowel sounds
- Involuntary guarding
- Rebound tenderness
- RUQ pain
- Signs of hypovolemic shock
- Diagnostic aids:
- CT
- Liver enzymes
- Angiography
- Therapeutic interventions:
- Hydration
- Urinary catheter
- NGT
- Antibiotics
- If there is evisceration, cover with saline gauze
Bowel Obstruction
- Blockage of the inside of the intestine
- Causes:
- Adhesions
- Hernias
- Fecal impactions
- Tumors
- Signs and symptoms:
- Crampy abdominal pain
- Nausea and vomiting (often of fecal matter)
- Abdominal distention
- Constipation
- Rectal blood and mucous without fecal matter or flatus
- Dehydration
- Diffuse abdominal tenderness and rigidity
- Diagnostic studies:
- CBC, renal panel, hepatic panel, BUN and creatinine, amylase
- Abdominal x-rays
- Colonoscopy
- Therapeutic interventions:
- Rehydration with crystalloids
- NGT to LIS
- NPO (nothing by mouth)
- Antibiotics
- Urinary catheter
- Treat or eliminate the cause
Abdominal Trauma
- Closed injury (blunt): Includes injuries caused by blunt force trauma, such as a car accident, a fall, or a blow to the abdomen.
- Open injury (penetrating): Includes injuries caused by piercing objects, such as knives, bullets, or shrapnel.
- Signs and symptoms:
- Mechanism of injury
- Pain
- Tachycardia
- Shock
- Bruising
- Distended or rigid abdomen
- Nausea and vomiting
Care for Penetrating Injuries
- For penetrating wounds:
- Check for exit wounds.
- Apply a dry, sterile dressing to the wound.
- If an object is impaled, stabilize it with bulky dressings.
- For abdominal eviscerations:
- Never attempt to replace organs.
- Cover organs with moist gauze, then a sterile dressing.
- Keep organs warm and moist.
- Transport promptly.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the anatomy of hollow and solid organs in the abdomen. This quiz also covers the essential components of gastrointestinal and genitourinary assessments, including history taking and physical examination techniques. Be prepared to identify key aspects of inspection, auscultation, and percussion.