Podcast
Questions and Answers
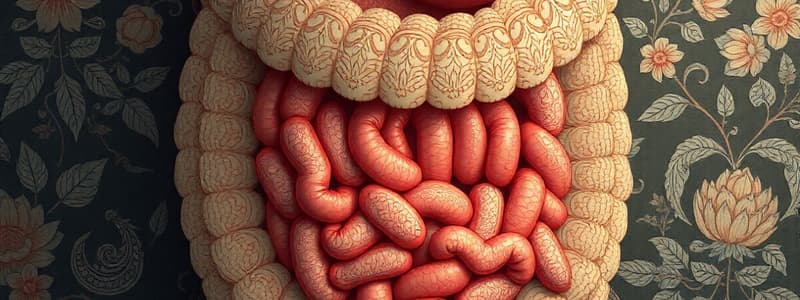
What is the primary function of the digestive system?
What is the primary function of the digestive system?
- To filter waste from the blood
- To produce hormones for growth
- To transport oxygen throughout the body
- To break down food into molecules (correct)
Which process initiates mechanical digestion?
Which process initiates mechanical digestion?
- Swallowing food into the esophagus
- Contraction of the stomach
- Chewing food with teeth (correct)
- Chemical breakdown by enzymes
What role does bile play in digestion?
What role does bile play in digestion?
- It is primarily responsible for protein breakdown
- It acts as a coagulant for food particles
- It breaks down carbohydrates into sugars
- It helps in the digestion of lipids (correct)
Which of the following describes peristalsis?
Which of the following describes peristalsis?
What is the initial site of chemical digestion?
What is the initial site of chemical digestion?
What are the simplest forms of food absorbed after digestion?
What are the simplest forms of food absorbed after digestion?
Which enzyme is responsible for carbohydrate digestion in the mouth?
Which enzyme is responsible for carbohydrate digestion in the mouth?
What is the primary role of catabolic processes in metabolism?
What is the primary role of catabolic processes in metabolism?
What process involves the reabsorption of amino acids and glucose into the blood?
What process involves the reabsorption of amino acids and glucose into the blood?
Which waste products are disposed of by the kidneys?
Which waste products are disposed of by the kidneys?
Which enzyme is secreted by the pancreas for lipid digestion?
Which enzyme is secreted by the pancreas for lipid digestion?
What is the main function of the urinary system?
What is the main function of the urinary system?
Which of the following is NOT a function of anabolic processes?
Which of the following is NOT a function of anabolic processes?
What is the approximate volume of filtrate produced by the kidneys per day?
What is the approximate volume of filtrate produced by the kidneys per day?
What is the net filtration pressure in the glomerulus?
What is the net filtration pressure in the glomerulus?
Which of the following best describes the process of reabsorption in the Proximal Convoluted Tubule (PCT)?
Which of the following best describes the process of reabsorption in the Proximal Convoluted Tubule (PCT)?
Which pressure opposes glomerular filtration?
Which pressure opposes glomerular filtration?
At what blood glucose level does glucosuria begin to occur?
At what blood glucose level does glucosuria begin to occur?
Which of the following correctly states the amount of sodium and water reabsorbed in the PCT?
Which of the following correctly states the amount of sodium and water reabsorbed in the PCT?
What is the permeability feature of the descending loop of the Loop of Henle?
What is the permeability feature of the descending loop of the Loop of Henle?
What percentage of the filtrate is typically reabsorbed by the nephron?
What percentage of the filtrate is typically reabsorbed by the nephron?
Which of the following substances is a common waste product excreted in urine?
Which of the following substances is a common waste product excreted in urine?
What is the primary component of urine by volume?
What is the primary component of urine by volume?
How does alcohol affect urine production?
How does alcohol affect urine production?
Which factor prevents excess loss of sodium and promotes water retention in the body?
Which factor prevents excess loss of sodium and promotes water retention in the body?
What does dialysis do for patients with kidney failure?
What does dialysis do for patients with kidney failure?
During dialysis, how does passive diffusion occur?
During dialysis, how does passive diffusion occur?
What daily urine output is considered oliguria?
What daily urine output is considered oliguria?
What is a potential consequence of untreated kidney failure?
What is a potential consequence of untreated kidney failure?
What is the primary function of the loop of Henle in the nephron?
What is the primary function of the loop of Henle in the nephron?
What determines the reabsorption in the distal convoluted tubule (DCT) and collecting tubule (CT)?
What determines the reabsorption in the distal convoluted tubule (DCT) and collecting tubule (CT)?
How does ADH affect water reabsorption in the kidneys?
How does ADH affect water reabsorption in the kidneys?
What is a significant effect of low levels of ADH in the body?
What is a significant effect of low levels of ADH in the body?
What is the primary role of sodium pumps in the ascending loop of Henle?
What is the primary role of sodium pumps in the ascending loop of Henle?
What is the relationship between the length of the loop of Henle and the ability to reabsorb water?
What is the relationship between the length of the loop of Henle and the ability to reabsorb water?
Which type of cells in the DCT and CT respond to ADH and aldosterone?
Which type of cells in the DCT and CT respond to ADH and aldosterone?
What is the process of selective transport from blood to the renal tubules called?
What is the process of selective transport from blood to the renal tubules called?
What is the typical blood pH level that must be maintained in the body?
What is the typical blood pH level that must be maintained in the body?
Where are the kidneys located in the human body?
Where are the kidneys located in the human body?
What is the maximum capacity of an adult urinary bladder?
What is the maximum capacity of an adult urinary bladder?
What is the primary function of the nephron in the kidneys?
What is the primary function of the nephron in the kidneys?
What happens during the filtration step of urine formation?
What happens during the filtration step of urine formation?
What defines the Glomerular Filtration Rate (GFR)?
What defines the Glomerular Filtration Rate (GFR)?
How long can a typical healthy adult hold urine in their bladder?
How long can a typical healthy adult hold urine in their bladder?
Which kidney is located higher in the abdomen?
Which kidney is located higher in the abdomen?
Flashcards
Digestive Enzymes
Digestive Enzymes
Substances that speed up chemical reactions in the digestive system, breaking down food into simpler molecules.
Chemical Digestion
Chemical Digestion
The process of breaking down complex food molecules into simpler molecules using enzymes.
Food Assimilation
Food Assimilation
The process of absorbing nutrients from digested food into the bloodstream.
Absorption (in Digestion)
Absorption (in Digestion)
Signup and view all the flashcards
Metabolism (Catabolism)
Metabolism (Catabolism)
Signup and view all the flashcards
Metabolism (Anabolism)
Metabolism (Anabolism)
Signup and view all the flashcards
Kidney Function
Kidney Function
Signup and view all the flashcards
Urinary System Function
Urinary System Function
Signup and view all the flashcards
Mechanical Digestion
Mechanical Digestion
Signup and view all the flashcards
Chemical Digestion
Chemical Digestion
Signup and view all the flashcards
Digestive System Function
Digestive System Function
Signup and view all the flashcards
Mastication
Mastication
Signup and view all the flashcards
Peristalsis
Peristalsis
Signup and view all the flashcards
Blood pH
Blood pH
Signup and view all the flashcards
Kidney location
Kidney location
Signup and view all the flashcards
Ureter function
Ureter function
Signup and view all the flashcards
Bladder function
Bladder function
Signup and view all the flashcards
Urethra function
Urethra function
Signup and view all the flashcards
Nephron
Nephron
Signup and view all the flashcards
Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR)
Signup and view all the flashcards
Urine Formation Steps
Urine Formation Steps
Signup and view all the flashcards
Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR)
Signup and view all the flashcards
Filtrate Composition
Filtrate Composition
Signup and view all the flashcards
Reabsorption in PCT
Reabsorption in PCT
Signup and view all the flashcards
Glucosuria
Glucosuria
Signup and view all the flashcards
Loop of Henle
Loop of Henle
Signup and view all the flashcards
Net Filtration Pressure
Net Filtration Pressure
Signup and view all the flashcards
Obligatory Reabsorption
Obligatory Reabsorption
Signup and view all the flashcards
Glomerular Capillary Hydrostatic Pressure
Glomerular Capillary Hydrostatic Pressure
Signup and view all the flashcards
Excreted Waste Products
Excreted Waste Products
Signup and view all the flashcards
Urine Composition
Urine Composition
Signup and view all the flashcards
Urine Volume (Normal)
Urine Volume (Normal)
Signup and view all the flashcards
ADH and Urine
ADH and Urine
Signup and view all the flashcards
Alcohol and Urine
Alcohol and Urine
Signup and view all the flashcards
Kidney Failure Treatment
Kidney Failure Treatment
Signup and view all the flashcards
Dialysis Function
Dialysis Function
Signup and view all the flashcards
Dialysis Method
Dialysis Method
Signup and view all the flashcards
Loop of Henle
Loop of Henle
Signup and view all the flashcards
Ascending Loop
Ascending Loop
Signup and view all the flashcards
Descending Loop
Descending Loop
Signup and view all the flashcards
DCT and CT Reabsorption
DCT and CT Reabsorption
Signup and view all the flashcards
ADH (Antidiuretic Hormone)
ADH (Antidiuretic Hormone)
Signup and view all the flashcards
Diabetes Insipidus
Diabetes Insipidus
Signup and view all the flashcards
Urine Concentration
Urine Concentration
Signup and view all the flashcards
Nephron Length
Nephron Length
Signup and view all the flashcards
Study Notes
Functioning Systems
- The presentation is by Prof. Dr. Eman Salah Abdel-Reheim
- The topic is Zoology.
- The location of the presentation is Beni-Suef University.
Food Assimilation
- Learning objectives include:
- General function of digestive system
- Mechanical & chemical digestion
- Simplest forms of nutrients & their absorption
- Simple outlines about metabolism
Functions of Digestive System
- Breaks down food into molecules.
- Absorbs molecules into blood for bodily distribution.
- Eliminates wastes from the body.
Digestion
- Digestion is the process by which the body breaks down food into small nutrient molecules.
- It begins in the mouth.
Types of Digestion
- Mechanical digestion: physically breaks down food into smaller pieces, beginning with chewing. The process includes mastication (chewing) and teeth cutting.
- Chemical digestion: breaks down food into smaller chemical building blocks using chemicals produced by the body. This begins in the mouth.
Mechanical Digestion Expressions
- Mastication: chewing and enzymatic breakdown by saliva.
- Deglutition: swallowing; voluntary in the mouth, involuntary in the esophagus.
Mechanical Digestion
- Churning in the stomach forms chyme.
- Peristalsis: contraction of circular muscle.
- Segmentation: contraction of longitudinal muscle (back and forth movement) till the colon.
Chemical Digestion: Digestive Juices
- Saliva: from parotid, sublingual, & submandibular glands.
- Gastric: chief cells for pepsinogen, parietal cells for HCl.
- Pancreatic: from exocrine cells in the pancreas.
- Bile: produced by the liver, stored in the gall bladder, secreted into the small intestine for lipid digestion.
- Intestinal Juice: secreted by the mucosa of the small & large intestines.
Chemical Digestion
- accomplished by enzymes :
- Mouth (carbohydrates): salivary amylase
- Stomach (proteins): pepsin
- Small intestine (lipids): trypsin, chymotrypsin, amylase, and lipase
- Small intestine (carbohydrates, proteins, and lactose) : maltase, sucrase, lactase, and peptidases from intestinal villi.
Absorption
- After digestion, the simplest forms of food (glucose, amino acids, and fatty acids) are absorbed.
- Absorption is the passage of these nutrients through the intestinal mucosa into the blood.
- Amino acids & glucose are absorbed into the blood by secondary active transport.
- Fatty acids enter the lymph via simple diffusion.
Metabolism
-
Catabolism:
- Hydrolysis: breaks down monomers.
- Cellular respiration: oxidizes monomers to yield energy
-
Anabolism:
- Cell maintenance & repair
- Growth
- Formation of secretions
- Nutrient reserves
Metabolic Processes of Substances
- Glucose: glycolysis, Kreb's cycle, electron transport chain, Glycogenesis, gluconeogenesis
- Fatty acids: beta-oxidation, Kreb's cycle, electron transport chain, lipogenesis
- Amino acids: deamination, Kreb's cycle, electron transport chain, synthesis of non-essential amino acids
Urinary System
- Learning objectives include:
- Functions of the urinary system
- Anatomy of the urinary system
- Nephron structure
- Urine formation: Filtration, Reabsorption, Secretion
- Urine composition
- Factors affecting kidney function
- Hemodialysis
Function of the Urinary System
- Regulates blood composition and volume to maintain homeostasis.
- Disposes of metabolic waste (urea, creatinine, ammonium, uric acid).
- Maintains water-salt and electrolyte balance (sodium, potassium, bicarbonate, etc.).
- Maintains acid-base balance (blood pH ~7.4).
Structure & Anatomy of the Urinary System
- Kidneys: located in the back of the abdomen, one on each side just below the diaphragm
- The left kidney is located in the T12 to L3 vertebrae and the right kidney is lower due to liver displacement.
- Each kidney weighs about 125-175 g in males and 115-155 g in females.
- Approximately 11-14 cm in length, 6 cm wide, and 4 cm thick.
- Uses 20-25% of the body’s oxygen
- Ureters: 25 cm long muscular tubes that carry urine from the kidneys to the bladder.
- Bladder: a triangle-shaped hollow organ in the lower abdomen, storing urine. Urine empties through the urethra.
- Urethra: a tube that carries urine out of the body.
Kidney Anatomy
- The kidney is protected by fibrous tissue, fat, muscle, and ribs.
- Consists of the outer renal cortex and inner medulla then pelvis. Renal cortex, Renal medulla, Renal papilla, Renal pyramid, Renal artery, Renal pelvis, Minor calyx, Major calyx, Renal vein, Bowman's capsule, Collecting duct, Nephron
Nephron
- The structural and functional unit of the kidney, composed of the renal corpuscle and renal tubules.
- Renal corpuscle: glomerular capsule (cup-shaped) and capillary network (glomerulus)
- Proximal convoluted tubule (PCT), Nephron loop (Loop of Henle), Distal convoluted tubule (DCT)
- Renal corpuscle: glomerular capsule (cup-shaped) and capillary network (glomerulus)
Steps in Urine Formation
- Filtration: water and small molecules are removed from the blood into the renal capsule (pressure filtration, depends on size).
- Reabsorption: water and essential molecules are returned to the blood in the renal tubules.
- Secretion: wastes and excess salts are added from body fluids to tubular fluid (urine) in the renal tubules.
Glomerular Filtration Rate (GFR)
- The amount of filtrate produced by the kidneys each minute.
- 20% of total blood enters each kidney every minute (~1000 -1200 ml/min).
- ≈625 ml of plasma only pass as filtrate.
- Only approx. 20% of the filtrate passes into the tubules.
- 125-130 ml of the filtrate passes through the renal tubules (~180 liters/day).
- The kidneys can filter ~150-200 liters of plasma per day.
Forces Affecting Filtration
- Glomerular capillary hydrostatic pressure (GHP) = +55 mmHg
- Blood osmotic (colloidal) pressure (BOP) = -30 mmHg
- Capsular hydrostatic pressure (CHP) = -15 mmHg
- Net filtration rate = +10 mmHg
Reabsorption
- Reabsorption of nutrients, electrolytes, and water occurs through mechanisms in the renal tubules.
- Proximal Convoluted Tubule (PCT)
- Loop of Henle
- Distal Convoluted Tubule (DCT)
PCT- Reabsorption ("Obligatory Reabsorption")
- Glucose and amino acids are pumped out of the tubules by secondary active transport.
- The transporter for glucose has a limited capacity.
- If blood glucose is above 180 mg/dL, glucose remains in the urine (glucosuria).
PCT- Reabsorption
- 70% of sodium and water are reabsorbed.
- Water moves into the peritubular space by osmosis (passively).
- Chloride follows sodium by simple diffusion.
- Some compounds present in high concentration in filtrate but low in blood can move through diffusion.
Loop of Henle- Reabsorption
- Descending loop: permeable to water, moves water out of the tubules down the osmotic gradient. NO sodium pumps.
- Ascending loop: thick epithelium, impermeable to water but has many sodium pumps.
So, why is the loop of Henle useful?
- The longer the loop, the deeper it travels into the hyperosmotic medulla; more reabsorption and more concentrated tubular fluid is formed
- The collecting tubule runs through the hyperosmotic medulla for greater ability to reabsorb H2O.
DCT and CT Reabsorption ("Facultative Reabsorption")
- Reabsorption here depends on the body's need
- DCT & CT walls have tight junctions, impermeable to water.
- The cell membrane has receptors able to bind and respond to hormones (ADH and aldosterone)
- The binding of hormones modifies the membrane permeability of water and ions based on need.
Regulation of ADH secretion
- ADH increases water retention and reduces urine volume, prevents dehydration.
- ADH regulates decreased blood volume and/or decreased blood pressure (BP), through baroreceptors in the cardiovascular system
- ADH also regulates increased salt concentration via osmoreceptors in the hypothalamus to monitor extracellular osmolality changes. (Why?)
DCT and CT-Reabsorption (Urine Concentration)
- Late distal tubule (impermeable to H2O) : :ADH is low → no binding → H2O is not reabsorbed
- Late distal tubule (permeable to H2O) : ADH is released → binds to receptors → aquaporin channels open → H2O moves into the blood → low urine volume with high concentration
Secretion and Excretion
- Secretion: Selective transport of molecules from blood in the peritubular capillaries to the lumen of renal tubules
- Example of excreted waste products: urea, excess drug metabolites, K+, H+, Ca++
- Excretion: the body removes urine; molecules are dumped outside the tubules.
Urine Formation Summary
- Diagram illustrating the process of urine formation in the nephron
- Shows different stages of filtration, reabsorption, secretion, and excretion in the kidney
Urine Composition
- Urine composition varies with time and reflects the amount of water and solutes eliminated by the kidneys to maintain homeostasis.
- Urine is 95-96% water and contains urea, uric acid, traces of amino acids, and electrolytes.
- Normal daily production is 600-2500 ml/day.
Factors that Affect Kidney Function
- ADH: prevents excess water loss (less urine volume & concentrated urine)
- Alcohol: inhibits ADH secretion (more urine volume & diluted urine)
- Aldosterone: prevents excess sodium and water loss (less urine volume, no effect on urine concentration - why?)
- Caffeine: increases rate of salt and water loss; blocks adenosine receptors
- Increased blood pressure: increase rate of water loss
Notes
- Kidney diseases affect structure and function in 5 stages (from normal function to failure)
- Kidney failure is fatal if untreated.
- Kidney failure is treated by dialysis or transplantation.
- Kidney is the first successfully transplanted organ in humans (in 1954).
Hemodialysis
- Dialysis is a treatment for people with kidney failure.
- The kidneys do not filter blood normally, causing waste and toxins to build up
- Dialysis removes waste products from the blood.
- The dialyzer separates blood from the dialysis solution using a thin membrane; passive diffusion between the blood and dialysate.
- Waste products are removed into the dialysate, while essential minerals and amino acids move from the dialysate to the blood.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.