Podcast
Questions and Answers
In a patient with fecal incontinence secondary to diabetic neuropathy and confirmed chronic diarrhea, which intervention necessitates the most judicious and nuanced consideration before implementation?
In a patient with fecal incontinence secondary to diabetic neuropathy and confirmed chronic diarrhea, which intervention necessitates the most judicious and nuanced consideration before implementation?
- Dietary modification focusing on stool-thickening agents like applesauce, being mindful of potential glycemic control issues in diabetic patients.
- Implementation of biofeedback therapy for pelvic floor muscle training, recognizing the possible limitations imposed by peripheral neuropathy. (correct)
- Meticulous perineal skin hygiene with barrier creams, carefully selecting products to avoid exacerbating potential fungal infections in immunocompromised individuals.
- Initiation of a bowel-training program with scheduled toileting, considering the potential for autonomic neuropathy affecting bowel motility.
A geriatric patient with a long history of laxative abuse presents with fecal incontinence. Anorectal manometry reveals severely diminished sphincter tone and rectal sensitivity. Beyond immediate cessation of laxatives, what is the most critical next step in this patient's comprehensive management?
A geriatric patient with a long history of laxative abuse presents with fecal incontinence. Anorectal manometry reveals severely diminished sphincter tone and rectal sensitivity. Beyond immediate cessation of laxatives, what is the most critical next step in this patient's comprehensive management?
- Prescribing a course of stimulant laxatives to 'retrain' the bowel and improve motor function over a short period.
- Performing flexible sigmoidoscopy to rule out structural abnormalities or inflammation contributing to incontinence.
- Instituting a structured bowel training program combined with biofeedback, tailored to address both sensory and motor deficits. (correct)
- Initiating a high-fiber diet and psyllium supplementation to increase stool bulk and improve bowel regularity immediately.
In the management of Irritable Bowel Syndrome (IBS) with diarrhea, which of the following pharmacological interventions aims to directly impede intestinal transit and augment water absorption?
In the management of Irritable Bowel Syndrome (IBS) with diarrhea, which of the following pharmacological interventions aims to directly impede intestinal transit and augment water absorption?
- Loperamide (Imodium) (correct)
- Propantheline (Pro-Banthine)
- Dicyclomine (Bentyl)
- Alosetron (Lotronex)
Following an extensive anterior resection with low colorectal anastomosis for rectal cancer, a patient experiences persistent fecal incontinence. What is the most appropriate initial surgical intervention to consider, assuming conservative management has failed and the anastomosis is confirmed to be intact?
Following an extensive anterior resection with low colorectal anastomosis for rectal cancer, a patient experiences persistent fecal incontinence. What is the most appropriate initial surgical intervention to consider, assuming conservative management has failed and the anastomosis is confirmed to be intact?
A patient diagnosed with Irritable Bowel Syndrome (IBS) presents with predominant constipation. Considering the recommended dietary and pharmacological interventions, which of the following strategies is most appropriate for initial management?
A patient diagnosed with Irritable Bowel Syndrome (IBS) presents with predominant constipation. Considering the recommended dietary and pharmacological interventions, which of the following strategies is most appropriate for initial management?
In a patient with chronic fecal incontinence, secondary to radiation proctitis following prostate cancer treatment, which management strategy demonstrates the highest degree of evidence-based rationale, considering the pathophysiology of radiation-induced tissue damage?
In a patient with chronic fecal incontinence, secondary to radiation proctitis following prostate cancer treatment, which management strategy demonstrates the highest degree of evidence-based rationale, considering the pathophysiology of radiation-induced tissue damage?
What is the rationale behind advising patients with Irritable Bowel Syndrome (IBS) to avoid gas-forming foods such as broccoli and cabbage?
What is the rationale behind advising patients with Irritable Bowel Syndrome (IBS) to avoid gas-forming foods such as broccoli and cabbage?
A researcher is designing a study to evaluate the efficacy of a novel biofeedback protocol for fecal incontinence. Which of the following outcome measures would provide the most clinically meaningful and comprehensive assessment of treatment success, considering the multifaceted impact of this condition?
A researcher is designing a study to evaluate the efficacy of a novel biofeedback protocol for fecal incontinence. Which of the following outcome measures would provide the most clinically meaningful and comprehensive assessment of treatment success, considering the multifaceted impact of this condition?
Considering the Rome IV criteria for diagnosing Irritable Bowel Syndrome (IBS), which of the following symptom clusters is essential, occurring on average at least once a week in the preceding three months?
Considering the Rome IV criteria for diagnosing Irritable Bowel Syndrome (IBS), which of the following symptom clusters is essential, occurring on average at least once a week in the preceding three months?
What is the most crucial differentiating factor in the pathophysiology of fecal incontinence caused by internal anal sphincter dysfunction versus that caused by external anal sphincter dysfunction?
What is the most crucial differentiating factor in the pathophysiology of fecal incontinence caused by internal anal sphincter dysfunction versus that caused by external anal sphincter dysfunction?
Given the multifactorial etiology of Irritable Bowel Syndrome (IBS), which of the following considerations is MOST critical when formulating a comprehensive management plan?
Given the multifactorial etiology of Irritable Bowel Syndrome (IBS), which of the following considerations is MOST critical when formulating a comprehensive management plan?
In the context of managing fecal incontinence related to repeated stool contact, which of the following interventions is MOST directly aimed at preventing the formation of anal sores (ulcers)?
In the context of managing fecal incontinence related to repeated stool contact, which of the following interventions is MOST directly aimed at preventing the formation of anal sores (ulcers)?
In a patient with fecal incontinence secondary to pelvic floor relaxation, what are the most crucial components to assess when determining candidacy for pelvic floor reconstructive surgery, beyond standard clinical and manometric evaluations?
In a patient with fecal incontinence secondary to pelvic floor relaxation, what are the most crucial components to assess when determining candidacy for pelvic floor reconstructive surgery, beyond standard clinical and manometric evaluations?
Considering the potential impact of straining during bowel movements, which of the following long-term consequences is MOST directly associated with this behavior?
Considering the potential impact of straining during bowel movements, which of the following long-term consequences is MOST directly associated with this behavior?
What is the MOST plausible underlying mechanism by which psychological factors and stress contribute to the pathogenesis and exacerbation of Irritable Bowel Syndrome (IBS)?
What is the MOST plausible underlying mechanism by which psychological factors and stress contribute to the pathogenesis and exacerbation of Irritable Bowel Syndrome (IBS)?
In the context of acute inflammatory disorders, appendicitis is characterized by inflammation of which specific anatomical structure?
In the context of acute inflammatory disorders, appendicitis is characterized by inflammation of which specific anatomical structure?
In the context of managing lactase deficiency, which intervention demonstrates an advanced understanding of calcium homeostasis and alternative metabolic pathways, going beyond simple supplementation?
In the context of managing lactase deficiency, which intervention demonstrates an advanced understanding of calcium homeostasis and alternative metabolic pathways, going beyond simple supplementation?
Which clinical scenario involving intestinal obstruction necessitates the most immediate and sophisticated integration of diagnostic modalities and therapeutic interventions, reflecting an in-depth understanding of pathophysiology?
Which clinical scenario involving intestinal obstruction necessitates the most immediate and sophisticated integration of diagnostic modalities and therapeutic interventions, reflecting an in-depth understanding of pathophysiology?
Considering the multifaceted etiology of paralytic ileus, which therapeutic strategy demonstrates the most nuanced understanding of gastrointestinal motility and neuromuscular physiology?
Considering the multifaceted etiology of paralytic ileus, which therapeutic strategy demonstrates the most nuanced understanding of gastrointestinal motility and neuromuscular physiology?
In managing a patient with a large bowel obstruction secondary to a malignant tumor, which perioperative intervention reflects the most sophisticated integration of surgical oncology principles and enhanced recovery after surgery (ERAS) protocols?
In managing a patient with a large bowel obstruction secondary to a malignant tumor, which perioperative intervention reflects the most sophisticated integration of surgical oncology principles and enhanced recovery after surgery (ERAS) protocols?
In the context of differentiating between small and large bowel obstruction, which constellation of clinical and paraclinical findings would most strongly suggest a distal ileal obstruction with impending strangulation, necessitating immediate surgical intervention?
In the context of differentiating between small and large bowel obstruction, which constellation of clinical and paraclinical findings would most strongly suggest a distal ileal obstruction with impending strangulation, necessitating immediate surgical intervention?
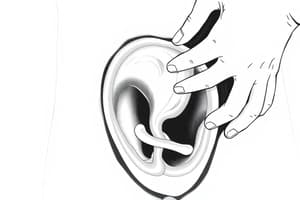
In the surgical construction of a Kock pouch, what precise physiological principle is leveraged to prevent retrograde flow and ensure continence, and what is the most critical technical challenge in maintaining its long-term efficacy?
In the surgical construction of a Kock pouch, what precise physiological principle is leveraged to prevent retrograde flow and ensure continence, and what is the most critical technical challenge in maintaining its long-term efficacy?
A patient post-total proctocolectomy with continent ileostomy (Kock pouch) presents with symptoms including increased pouchitis episodes, difficulty in catheterizing the pouch, and signs suggestive of vitamin B12 deficiency. Beyond routine management, which advanced diagnostic modality would be most appropriate to assess the underlying etiology?
A patient post-total proctocolectomy with continent ileostomy (Kock pouch) presents with symptoms including increased pouchitis episodes, difficulty in catheterizing the pouch, and signs suggestive of vitamin B12 deficiency. Beyond routine management, which advanced diagnostic modality would be most appropriate to assess the underlying etiology?
In the nutritional management of a patient with a newly formed ileostomy, what is the most critical consideration regarding electrolyte balance, and how does this impact the formulation of an optimal rehydration strategy?
In the nutritional management of a patient with a newly formed ileostomy, what is the most critical consideration regarding electrolyte balance, and how does this impact the formulation of an optimal rehydration strategy?
An adolescent patient newly diagnosed with celiac disease expresses reluctance to adhere to a strict gluten-free diet due to social constraints and perceived limitations on food choices. What is the most evidence-based psychological intervention to improve long-term adherence?
An adolescent patient newly diagnosed with celiac disease expresses reluctance to adhere to a strict gluten-free diet due to social constraints and perceived limitations on food choices. What is the most evidence-based psychological intervention to improve long-term adherence?
Which of the following is a pathophysiological mechanism that can potentially explain the increased risk of autoimmune diseases such as rheumatoid arthritis and type 1 diabetes mellitus in individuals with celiac disease?
Which of the following is a pathophysiological mechanism that can potentially explain the increased risk of autoimmune diseases such as rheumatoid arthritis and type 1 diabetes mellitus in individuals with celiac disease?
A patient with long-standing celiac disease, despite strict adherence to a gluten-free diet, continues to experience symptoms of malabsorption and weight loss. Which of the following advanced diagnostic strategies is most appropriate to evaluate the possibility of refractory celiac disease?
A patient with long-standing celiac disease, despite strict adherence to a gluten-free diet, continues to experience symptoms of malabsorption and weight loss. Which of the following advanced diagnostic strategies is most appropriate to evaluate the possibility of refractory celiac disease?
A researcher is investigating novel therapeutic targets for celiac disease. Which of the following molecular pathways, if successfully inhibited, would most likely prevent the intestinal damage associated with gluten ingestion?
A researcher is investigating novel therapeutic targets for celiac disease. Which of the following molecular pathways, if successfully inhibited, would most likely prevent the intestinal damage associated with gluten ingestion?
In a patient with suspected lactase deficiency, which of the following confirmatory diagnostic tests would provide the most accurate assessment of lactase enzyme activity in the small intestine?
In a patient with suspected lactase deficiency, which of the following confirmatory diagnostic tests would provide the most accurate assessment of lactase enzyme activity in the small intestine?
A patient with confirmed lactase deficiency presents with persistent gastrointestinal symptoms despite adherence to a lactose-restricted diet. Which of the following pathophysiological mechanisms could explain the continued symptoms?
A patient with confirmed lactase deficiency presents with persistent gastrointestinal symptoms despite adherence to a lactose-restricted diet. Which of the following pathophysiological mechanisms could explain the continued symptoms?
What is the most accurate rationale for why individuals with lactase deficiency might exhibit variable degrees of lactose intolerance?
What is the most accurate rationale for why individuals with lactase deficiency might exhibit variable degrees of lactose intolerance?
In the context of acute appendicitis, which pathophysiological mechanism most accurately describes the sequence of events leading to perforation, considering the interplay between intraluminal pressure, bacterial proliferation, and compromise of the appendiceal vascular supply?
In the context of acute appendicitis, which pathophysiological mechanism most accurately describes the sequence of events leading to perforation, considering the interplay between intraluminal pressure, bacterial proliferation, and compromise of the appendiceal vascular supply?
A patient presents with suspected acute appendicitis. Considering the limitations of individual clinical signs, which combination of findings would yield the highest positive predictive value for diagnosing acute appendicitis, accounting for potential confounders and variations in anatomical location?
A patient presents with suspected acute appendicitis. Considering the limitations of individual clinical signs, which combination of findings would yield the highest positive predictive value for diagnosing acute appendicitis, accounting for potential confounders and variations in anatomical location?
In a patient presenting with atypical symptoms suggestive of appendicitis, which advanced imaging modality, beyond standard radiography, would offer the most definitive diagnostic information while minimizing radiation exposure, particularly in younger patients and pregnant individuals?
In a patient presenting with atypical symptoms suggestive of appendicitis, which advanced imaging modality, beyond standard radiography, would offer the most definitive diagnostic information while minimizing radiation exposure, particularly in younger patients and pregnant individuals?
Considering the potential for rapid progression of appendicitis to perforation and peritonitis, which intervention should be prioritized in the initial management of a patient with suspected appendicitis prior to definitive surgical intervention, accounting for individual patient factors and potential comorbidities?
Considering the potential for rapid progression of appendicitis to perforation and peritonitis, which intervention should be prioritized in the initial management of a patient with suspected appendicitis prior to definitive surgical intervention, accounting for individual patient factors and potential comorbidities?
Following an open appendectomy for perforated appendicitis, which specific post-operative nursing intervention is most critical in preventing intra-abdominal abscess formation, considering the principles of surgical site infection prevention and the pathophysiology of peritoneal contamination?
Following an open appendectomy for perforated appendicitis, which specific post-operative nursing intervention is most critical in preventing intra-abdominal abscess formation, considering the principles of surgical site infection prevention and the pathophysiology of peritoneal contamination?
What is the most likely long-term complication following a ruptured appendix that was treated with an appendectomy?
What is the most likely long-term complication following a ruptured appendix that was treated with an appendectomy?
Which of the following is a contraindication for laparoscopic appendectomy?
Which of the following is a contraindication for laparoscopic appendectomy?
What is the primary reason for avoiding the use of laxatives or enemas in a patient suspected of having acute appendicitis?
What is the primary reason for avoiding the use of laxatives or enemas in a patient suspected of having acute appendicitis?
Why is it important to position a patient in high-Fowler's position post-appendectomy?
Why is it important to position a patient in high-Fowler's position post-appendectomy?
Which diagnostic finding is most indicative of appendiceal perforation rather than simple appendicitis?
Which diagnostic finding is most indicative of appendiceal perforation rather than simple appendicitis?
Flashcards
Fecal Incontinence
Fecal Incontinence
Involuntary passage of stool from the rectum.
Causes of Fecal Incontinence
Causes of Fecal Incontinence
Trauma, neurologic disorders, infection, diarrhea, fecal impaction, medications, or age-related muscle weakness.
Risk Factors: Fecal Incontinence
Risk Factors: Fecal Incontinence
Age, female gender, nerve damage, dementia, or physical disability.
Symptoms: Fecal Incontinence
Symptoms: Fecal Incontinence
Signup and view all the flashcards
Fecal Incontinence: Dx Tests
Fecal Incontinence: Dx Tests
Signup and view all the flashcards
Medical Management: Fecal Incontinence
Medical Management: Fecal Incontinence
Signup and view all the flashcards
Nursing Management: Fecal Incontinence
Nursing Management: Fecal Incontinence
Signup and view all the flashcards
Complications of Stool Exposure
Complications of Stool Exposure
Signup and view all the flashcards
Preventing Constipation
Preventing Constipation
Signup and view all the flashcards
Controlling Diarrhea
Controlling Diarrhea
Signup and view all the flashcards
Preventing Straining
Preventing Straining
Signup and view all the flashcards
Rome IV Criteria for IBS
Rome IV Criteria for IBS
Signup and view all the flashcards
Cause of IBS
Cause of IBS
Signup and view all the flashcards
Managing IBS with Constipation
Managing IBS with Constipation
Signup and view all the flashcards
Managing IBS with Diarrhea
Managing IBS with Diarrhea
Signup and view all the flashcards
Appendicitis Defined
Appendicitis Defined
Signup and view all the flashcards
Intestinal Obstruction
Intestinal Obstruction
Signup and view all the flashcards
Mechanical Obstruction
Mechanical Obstruction
Signup and view all the flashcards
Intussusception
Intussusception
Signup and view all the flashcards
Volvulus
Volvulus
Signup and view all the flashcards
Paralytic Ileus
Paralytic Ileus
Signup and view all the flashcards
Ileostomy
Ileostomy
Signup and view all the flashcards
Kock Pouch
Kock Pouch
Signup and view all the flashcards
Post-surgery Ostomy Diet
Post-surgery Ostomy Diet
Signup and view all the flashcards
Celiac Disease
Celiac Disease
Signup and view all the flashcards
Gluten
Gluten
Signup and view all the flashcards
Celiac stool characteristics
Celiac stool characteristics
Signup and view all the flashcards
Celiac Biopsy
Celiac Biopsy
Signup and view all the flashcards
Gluten-free Diet
Gluten-free Diet
Signup and view all the flashcards
Lactase Deficiency
Lactase Deficiency
Signup and view all the flashcards
Symptoms of Lactose Intolerance
Symptoms of Lactose Intolerance
Signup and view all the flashcards
Appendicitis Cause
Appendicitis Cause
Signup and view all the flashcards
Simple Appendicitis
Simple Appendicitis
Signup and view all the flashcards
Gangrenous Appendicitis
Gangrenous Appendicitis
Signup and view all the flashcards
Perforated Appendicitis
Perforated Appendicitis
Signup and view all the flashcards
Appendicitis Manifestations
Appendicitis Manifestations
Signup and view all the flashcards
Blumberg's Sign
Blumberg's Sign
Signup and view all the flashcards
Rovsing's Sign
Rovsing's Sign
Signup and view all the flashcards
Iliopsoas Muscle Test
Iliopsoas Muscle Test
Signup and view all the flashcards
Appendicitis CBC Result
Appendicitis CBC Result
Signup and view all the flashcards
Appendectomy
Appendectomy
Signup and view all the flashcards
Study Notes
Fecal Incontinence
- This is the involuntary passage of stool from the rectum.
- Factors influencing it include:
- The rectum's sensitivity
- Stool consistency/amount
- Anal sphincter integrity
- Rectal motility
Causes of Fecal Incontinence
- Trauma, especially after rectal surgeries
- Neurologic disorders like stroke, multiple sclerosis, diabetic neuropathy, and dementia
- Inflammation and infection
- Diarrhea
- Chemotherapy and radiation treatment
- Fecal impaction and Pelvic floor relaxation
- Laxative abuse, medications, and advancing age which causes loss of anal or rectal muscle tone
Risk Factors
- Age
- Being female, nerve damage, dementia, and physical disability
Clinical Manifestations
- Minor soiling and occasional urgency
- Loss of bowel control (partial or complete)
- Poor control of flatus
- Diarrhea or constipation
Assessment & Diagnostic Tests
- Rectal examination and flexible sigmoidoscopy are used
- Barium enema, CT scan, and anorectal manometry
Medical Management
- If the cause is fecal impaction, the impaction is manually removed then the rectum is cleaned.
- Biofeedback therapy with pelvic floor muscle training can assist with decreased sensory awareness or sphincter control
- Bowel training programs can also be implemented.
Surgical Management
- Surgical reconstruction, artificial sphincter implantation, sphincter repair, and fecal diversion.
Nursing Management
- Gather a thorough health history, noting surgical history, dietary habits, bowel habits, any problems, and current medications.
- Initiate a bowel-training program, set a schedule for bowel regularity.
- Offer foods that thicken stool such as applesauce and psyllium fiber products.
- Maintain perineal skin integrity, minimize brief/diaper use, teach meticulous hygiene, and use skin protection products.
- Consider fecal incontinence devices.
Complications
- Emotional distress, from the loss of control of bodily functions
- Skin irritation because the constant contact with stool can cause sores or ulcers.
Prevention
- Reduce constipation by drinking plenty of fluids, eating more high-fiber foods, and increasing exercise.
- Aim to control diarrhea: treating or eliminating the cause of diarrhea can help prevent incontinence.
- Avoid straining during bowel movements as it could weaken sphincter muscles.
Irritable Bowel Syndrome (IBS)
- Complex syndrome marked by intermittent abdominal pain and stool pattern irregularities
- Peristaltic waves are affected in the intestine in both intensity and how well they propel fecal matter.
- Bowel pattern changes include constipation, diarrhea, or both.
Signs & Symptoms
- Abdominal distension, excessive flatulence and a continual urge to defecate
- Urgency and a sensation of incomplete evacuation
Rome IV Criteria for Diagnosis
- Recurrent abdominal pain (at least one day per week) during the last three months, associated with at least two of the following:
- Related to defecation
- Associated with changes in stool frequency or appearance
Cause and Incidence
- The cause of IBS is unknown, it is a functional disorder of intestinal motility linked to neuroendocrine dysregulation or vascular metabolic disturbance.
- IBS is more common in women.
Predisposing Factors
- Stress and psychological factors
- Prior gastroenteritis and specific food intolerance
Nursing Management for IBS
- For IBS with constipation:
- Consume 20 g per day of dietary fiber and a bulking agent (Metamucil).
- Tegaserod (Zelnorm) aids motility.
- For IBS with diarrhea:
- Antispasmodic agents such as Dicyclomine [Bentyl] or Propantheline [Pro-Banthine] taken before meals
- Loperamide (Imodium) is a synthetic opioid that minimizes intestinal water absorption and transit
- Alosetron (Lotronex) can have side effects like severe constipation/ischemic colitis
- To generally treat IBS, avoid gas-forming foods (broccoli, cabbage)
- Avoid alcohol use and cigarette smoking
- Cognitive-behavioral therapy, acupuncture, hypnosis, Chinese herbs, and relaxation/stress management techniques.
Acute Inflammatory Disorders: Appendicitis
- Appendicitis is an inflammation of the appendix — a narrow, blind tube extending from the inferior cecum.
- Obstruction of the lumen by a fecalith (accumulated feces) is the most common cause.
Classifications
- Simple: appendix is inflamed but still intact
- Gangrenous: Tissue necrosis with microscopic perforation areas
- Perforation: Large perforation with contents flowing into the peritoneal cavity
Manifestations
- Begins with periumbilical pain; followed by anorexia, nausea, and vomiting
- Low-grade fever
- Pain becomes persistent and shifts to the RLQ at McBurney's point
Signs of Appendicitis
- Blumberg's sign (rebound tenderness) the abdomen is sensitive after the tips of the fingers are pressed gently into the abdominal wall and then withdrawn suddenly
- Rovsing's sign is felt at the RLQ when LLQ is palpated while the Psoas' sign show when the person lies still with right leg drawn up
- An Iliopsoas muscle test will result in pelvic pain if flexing the right thigh against resistance
- An Obturator muscle test will cause pain when the right thigh is flexed 90° and the leg rotated internally/externally.
Diagnostic Studies
- X-ray acts as a confirmatory test
- Complete bloodcount reveals an elevated WBC (10,000/mm3 – 20,000/mm3)
- Urinalysis is used to rule out urinary tract infection.
Complications & Management
- Perforation & peritonitis
- Surgical management: appendectomy (open abdominal or laparoscopic)
Nursing Management
- Implement with NPO.
- Avoid laxatives and enemas to prevent increased peristalsis, which could lead to perforation.
- Apply an ice bag to the RLQ.
- Place the patient in high-Fowler's position before and after surgery.
- Administer Morphine Sulfate for postoperative pain relief.
- Monitor the patient for signs of peritonitis.
Peritonitis
- Peritonitis is the inflammation of the peritoneum.
- Primary causes include bacterial infection such as E.coli, Klebsiella, Proteus, and Pseudomonas.
- Secondary causes include ruptured appendicitis, ruptured diverticulitis, perforated PUD, and postoperative complications.
Manifestations
- Abdominal pain (most common symptom)
- Tenderness, muscular rigidity and spasm, absent bowel sounds (paralytic ileus)
- High fever, tachycardia, diaphoresis
- Drawing the knees up to the chest
Complications
- Hypovolemic shock
- Septic shock
- Acute respiratory distress syndrome
Diagnostic Studies
- Elevated WBC count and hemoconcentration via CBC
- Peritoneal aspiration (paracentesis) tests for blood, bile, pus, amylase, fungus, or bacteria
- X-ray, CT scan, UTz, or perioneoscopy
Surgical & Nursing Management
- Surgical intervention involves laparoscopic repair to treat the underlying cause
- NPO, NGT insertion, IVF, semi-fowler's position with knees flexed, oxygen, analgesics, and antibiotics
- Monitor vitals frequently, and provide a quiet, restful environment post-op
Diverticular Disease
- Diverticulum: a saccular dilation/outpouching of the mucosa through the circular smooth muscle of the intestinal wall
- Diverticulosis: a condition where an individual has noninflamed diverticula
- Diverticulitis: an inflammation and obstruction of a colonic diverticulum
Causes
- Lack of dietary fiber intake
- Loss of muscle mass and collagen with aging
- Associated with obesity
Manifestations
- Diverticulum is primarily asymptomatic
- Diverticulitis:
- LLQ abdominal pain (most common symptom)
- Nausea, vomiting, changes in bowel habits, and bloating
- Palpable abdominal mass
Diagnostics
- UTz & CT scan with contrast
- Barium enema and colonoscopy are contraindicated
- CBC showing leukocytosis and elevated sedimentation rate
Nursing Management
- Emphasize a high-fiber diet rich in fruits and vegetables
- Minimizing fat and red meat intake
- High levels of physical activity
- Weight reduction for the obese
- Avoid increasing intra-abdominal pressure
- Observe for possible peritonitis
Pharmacological Management
- Bulk-forming laxatives such as Psyllium (Metamucil) and stool softeners like Docusate (Colace)
- Bisacodyl (Dulcolax), antispasmodics such as Propantheline (Pro-Banthine), and the pain reliever Meperidine (Demerol)
- Note: Morphine is contraindicated
Acute Gastroenteritis (AGE)
- An inflammation of the mucosa of the stomach and small intestine
- Manifestations: nausea, vomiting, diarrhea, abdominal cramping and distension, fever, and increased WBC with blood or mucous in the stool.
- Cause: Salmonella and trichinosis in street foods or from contaminated water
- Monitoring Intake and Output.
- If a patient shows vomiting or dehydration, IVF and NPO.
Nursing Management for AGE
- Institute medical asepsis and infection control
- Educate about proper handwashing and instruct on how to prep/handle foods.
Inflammatory Bowel Disease (IBD)
- Regional Enteritis (Crohn's Disease), the most frequent site of inflammation and ulceration is the terminal ileum. With Inflammation involving all layers of the bowel wall (transmural lesions) With very deep ulcerations.
Ulcerative Colitis
- Usually starts in the rectum and spreads in a continuous pattern up the colon
- Inflammation involves mucosa and submucosa
Clinical Manifestations of Crohn's Disease
- Skip lesions where healthy tissue is interspersed with areas of classic cobblestone.
- Palpable mass felt in right iliac fossa, RLQ pain, crampy abdominal pain after meals, abdominal tenderness and spasm (pain relieved by defecation)
- There is weight loss, anemia (due to malabsorption), and steatorrhea (excessive fat in the stool)
- Diarrhea and Fever
Clinical Manifestations of Ulcerative Colitis
- Continous areas of ulcerations (rectum and colon) and inflammation of the mucosa and submucosa
- LLQ pain, intermittent tenesmus, and rectal bleeding
- Bloody diarrhea (10-20x a day)
- Minimal nutritional deficiencies and fever
Complications of IBD
- Regional Enteritis (Crohn's Disease): Fistula and Malnutrition as well as an increased chance of of recurrence after surgery
- Ulcerative Colitis: Can include Toxic megacolon, Perforation, Colon cancer, Hemorrhage, Skin lesions (erythema nodosum), Eye lesions (Uveitis), and Arthritis
Diagnostics for Crohn's Disease & Ulcerative Colitis
-
Crohn's Disease would require:
- Barium study (Upper GI) with the classic "string sign"
- CT scan showing bowel wall thickening and fistula formation
- CBC revealing decreased Hemoglobin and Hematocrit
- ESR and C-reactive proteins revel reveal an elevation
- Serum Albumin reveals diminished level
- WBC reveals an infectious process
- Capsule endoscopy and prevalence in Ashkenzai Jews Whites
-
Ulcerative Colitis would require:
- Barium enema shows mucosal irregularities, shortening of the colon, and dilation of bowel loops.
- Colonoscopy to show Friable and Infected mucosa -> Whites often get and are Diagnosed from adolescence through 30 year old
Causes of Inflammatory Bowel Disease
- Unknown but can by caused from:
- Autoimmune= CARD 1
- Hereditary
- Environment factors= food additives, pesticides, tobacco, radiation
Pharmacological Management of IBD
- Aminosalicylates: decreases GI inflammation.
- Sulfasalazine may cause orange discoloration of skin and urine, avoid sunlight.
- Mesalamine and Olsalazine
- Antimicrobials: prevent or treat secondary infections
- Metronidazole (Flagyl), Ciprofloxacin (Cipro), Clarithromycin (Biaxcin)
- Cortiocosteriods: Decrease inflimmation
- Prednisone, Hydrocortisone, Methylprednisolone
- Immunosuppressants suppress immune response
- Azathioprine (Imuran), Cyclosporine, 6-Mercaptopurine, Biologic therapy inhibits the cytokine tumor necrosis factor (TNF), Infliximab (Remicade).
Ileostomy
- Surgical procedure that involves Total Proctocolectomy with Permanent Ileostomy: involves the removal of colon and rectum with closure of the anus. Then and the end of ileum is brought out through the abdominal wall to create a ostomy. and The stoma is usually placed in the RLQ below the belt line.
- Surgical procedure that involves Total Proctocolectomy with Permanent Ileostomy uses what is called “Kock Pouch”, a surgical procedure where the the distal segment of the Ileum to create a one way Nipple Valve.
Ileostomy Nursing Management
- Enhance nutritional status/ nutritional therapy
- Diet high in CHON, calories, low residue, low in fat and suppplement with Vitamin therapy,iron, electrolytes, and blood replacement. Avoid all forms of Smoking / Alcohol, and and Diarrheal foods with rest periods.
- Provide with emotional support with psychotherapy and group sessions.
Malabsorption
- Nutrients no longer effectively absorbed in the small intestines
- Causes:
- Celiac Disease marked atrophy of the villi characterized in the proximal small intestine induced by ingestion of gluten-containing foods
- Nontropical Sprue
- Gluten = Made of high-Molecular weight protein in Barley, Rye, Oats and, Wheath
- Associated with autoimmune diseases, such as rheumatoid arthritis, type 1 diabetes mellitus, and thyroid disease
###Manifestations / Management of Malabsorption
- Foul-smelling diarrhea, Abdominal distension, Anorexia, Wasting,Failure to thrive.
- Confirmatory Histologic / diagnostic examination with biopsy shows flattened mucosa and noticeable losses of villi -Management involves: - Gluten-free diet for life , - Corticosteroids
###Example Of Foods Free of Gluten
- Eggs, Potatoes, Butter, Cheese or Cottage cheese, Meat/Fish/Poultry, Soy/Unflavored Milk Product, Bread product, Peanut Butter, Fresh Fruits,
- Flax/Corn /Rice/Tapioca ,Coffee ,Tea, Corn Tortillas ,Cocoa.
Lactase Deficiency
- a condition in which the lactase enzyme is deficient or absent
- Lactose is the enzyme that breaks down lactose into glucose and galactose
- Can be genetic
- Related to Inflimmatory Bowel Disease, Gastroenteritis, AND Celiac Disease
- Causes :Bloating, flatulence, cramping abdominal pain, and diarrhea, which are often confirmed by a lactose tolerance test or a lactose hydrogen breath test.
- Treats by Avoid milk, milk products,and Calcium supplements and live culture yogurt as a alternative with commercially available Lactaid enzyme .
Intestinal Obstruction
- Partial or complete impairment of forward flow of intestinal contents occurs due with Blockage of movement that causes an in movement through parts of small and large intestine:
Causes of Intestinal Obstruction.
- Mechanical Obstruction an obstruction caused by pressure on the intestinal wall occurs:
- Adhesions: which lead to intussusceptions or loops of intestine becoming one located below Intusseception
- volvulus/ tummor
Nonmechanical Obstruction
- neurological or vascular related disorders called paralytic ileus and may be due to postoperative abdominal surgeries and can result In mesentery infarction with presence of bowel sounds with CBC
Clinical Manifestations:
Small Intestinal Obstructions has Onset, that is Vomiting frequently with Copious colicky intermittent pain due to feces.
- Large Intestinal Obstructions has onset, then gradual low grade cramping the abdomen, constipation Abdominal distention is related to fluid levels with Gas in Intenstiones, and
- Diangostics through Abdominal imaging such as rays using Bariun Enemas to locate, CBC and Ultrasonds
Treatments of Intertional Obstuction
- Surgical= Partitial/ Total colectomy, or Ileostomy after colonoscopy because extensive obstruction ( NPOA, Insertation, Decomression, Analgesiz
- Medical management of F&E
- Nursing actions include: -F&E, Asecultating, Palate bowel sunds, passing stones through F&E with IO with dehydration and Comfort patient.
Management of Clients With Anorectal Disorders: Hemorrhoids
- Dilated hemorrhoidal veins, which has two types: =Located Above internals- below internal above external-
- Degree of internal Hemorrhoid Prolabses is 1st-No Prolapse with Just vein appearance -2nd Prolapse of straining but comes back slowly -3nd need someone to push the protrusion back but does not stay -Prolapsed out and never comes back Result from stretching during heavy deication,
- During defecation, venules become dilated
- Symptoms-Pruritus, rectal pain, prolapse, Asym
Hemmorhoids- Treatments and Solutions
- DRE-visual for exterrnal examination .
- Rubber band Ligation with Anoscopy and Ligation
- Sclertheraphy 5% Injection of Phenol in the the base causing Thrombusus
- StapledHemmohectomy removes prolapses Hemorrhiodactomy surgical removal that is painful with 5-20 minutes Sitz Bath
- Nursing Solutions includes hydro cortisol cream that prevent side effects such as Derm/Mucosal.
###Anal Fissure
- Skin ulcer that line the area that cause irritation and inflammation.
- Causes of skin issues
Treatment of Anal Fissures:
- Local injection of botulinum toxin (botox)
-Topical NTG, calcium channel blockers= are used to decrease rectal anal pressure and with stool.
- Surgical Management including,excision if the fissurtes of the issues for better resond to treatments.
- Surgical Managements can can be followed a 3 ways
- Fistulotmy/Fistulectomy
- Anal Fistula
- Complication of Crohhns that requires persistient cleaning or stull in vagina ,butt cheeks with surgicals action.
- Anorectal Abscess that cuases infection or aids in the site that need removal such as Local pain and swelling
- Foul-smelling drainage
- Tenderness
-Elevated temparute from this may need anal packing with surgical dranage and compresses.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.