Podcast
Questions and Answers
What characterizes the second stage in volume-loading hypertension?
What characterizes the second stage in volume-loading hypertension?
- High blood pressure and high total peripheral resistance (correct)
- Low blood pressure and high cardiac output
- High blood pressure and elevated cardiac output
- Normal blood pressure and low total peripheral resistance
In volume-loading hypertension, what happens to total peripheral resistance after hypertension develops?
In volume-loading hypertension, what happens to total peripheral resistance after hypertension develops?
- It increases as a secondary response to hypertension (correct)
- It fluctuates randomly without a clear trend
- It remains normal and unaffected
- It decreases as a direct cause of hypertension
What measurement may often fail to detect in the second stage of volume-loading hypertension?
What measurement may often fail to detect in the second stage of volume-loading hypertension?
- Abnormally elevated cardiac output (correct)
- Total blood volume
- Decreased peripheral resistance
- Normal blood pressure ranges
Which factor is primarily secondary to hypertension in volume-loading hypertension?
Which factor is primarily secondary to hypertension in volume-loading hypertension?
What mechanism is indicated to be ineffective in managing blood pressure in patients maintained with an artificial kidney?
What mechanism is indicated to be ineffective in managing blood pressure in patients maintained with an artificial kidney?
How does renal function relate to hypertension in the context of volume-loading?
How does renal function relate to hypertension in the context of volume-loading?
What is a significant effect of elevated salt intake on arterial pressure?
What is a significant effect of elevated salt intake on arterial pressure?
What occurs in the initial weeks of volume-loading hypertension as indicated by the provided data?
What occurs in the initial weeks of volume-loading hypertension as indicated by the provided data?
What is the initial cause of hypertension in volume-loading hypertension?
What is the initial cause of hypertension in volume-loading hypertension?
Which of the following is a consequence of elevated arterial pressure on kidney function?
Which of the following is a consequence of elevated arterial pressure on kidney function?
After several weeks of volume loading, what change occurs to the extracellular fluid volume?
After several weeks of volume loading, what change occurs to the extracellular fluid volume?
What effect does volume loading have on total peripheral resistance after several weeks?
What effect does volume loading have on total peripheral resistance after several weeks?
What primarily mediates hypertension in the first stage of volume-loading hypertension?
What primarily mediates hypertension in the first stage of volume-loading hypertension?
Which of the following mechanisms is involved in renal autoregulation?
Which of the following mechanisms is involved in renal autoregulation?
How does increased salt intake affect arterial pressure in the context of volume loading?
How does increased salt intake affect arterial pressure in the context of volume loading?
During the progression of volume-loading hypertension, what happens to cardiac output?
During the progression of volume-loading hypertension, what happens to cardiac output?
Which statement accurately reflects a physiological adaptation in volume-loading hypertension?
Which statement accurately reflects a physiological adaptation in volume-loading hypertension?
What role does increased cardiac output play in the context of hypertension?
What role does increased cardiac output play in the context of hypertension?
What is the primary mechanism through which renal autoregulation influences blood flow?
What is the primary mechanism through which renal autoregulation influences blood flow?
How does increased salt intake primarily affect arterial pressure in the absence of impaired kidney function?
How does increased salt intake primarily affect arterial pressure in the absence of impaired kidney function?
What condition is characterized by chronic hypertension due to excess extracellular fluid accumulation?
What condition is characterized by chronic hypertension due to excess extracellular fluid accumulation?
What happens to total peripheral resistance when autoregulation mechanisms constrict blood vessels?
What happens to total peripheral resistance when autoregulation mechanisms constrict blood vessels?
Which physiological process is disrupted when renal function is impaired, leading to chronic hypertension?
Which physiological process is disrupted when renal function is impaired, leading to chronic hypertension?
What is the primary initial cause of hypertension related to body fluid volume?
What is the primary initial cause of hypertension related to body fluid volume?
How does the autoregulation mechanism affect cardiac output in hypertension?
How does the autoregulation mechanism affect cardiac output in hypertension?
What is secondary to the initial increase in cardiac output during the development of hypertension?
What is secondary to the initial increase in cardiac output during the development of hypertension?
What triggers the release of renin from the JG cells during low arterial pressure?
What triggers the release of renin from the JG cells during low arterial pressure?
What is a consequence of allowing extracellular fluid volume to increase without intervention?
What is a consequence of allowing extracellular fluid volume to increase without intervention?
What type of hypertension is characterized by excess aldosterone?
What type of hypertension is characterized by excess aldosterone?
Which of the following factors contributes to the regulation of renin release during low sodium chloride levels?
Which of the following factors contributes to the regulation of renin release during low sodium chloride levels?
In the context of hypertension, what role does the sympathetic nervous system play?
In the context of hypertension, what role does the sympathetic nervous system play?
Which of the following is NOT a mechanism that leads to increased renin release?
Which of the following is NOT a mechanism that leads to increased renin release?
What is the effect of sustained high peripheral resistance in hypertension?
What is the effect of sustained high peripheral resistance in hypertension?
What is a key characteristic of volume-loading hypertension?
What is a key characteristic of volume-loading hypertension?
What effect does consuming 0.9% saline solution have on dogs with significant renal tissue removed?
What effect does consuming 0.9% saline solution have on dogs with significant renal tissue removed?
What primary change occurs in circulatory function during the development of volume-loading hypertension?
What primary change occurs in circulatory function during the development of volume-loading hypertension?
How does excess salt intake influence arterial pressure?
How does excess salt intake influence arterial pressure?
Which mechanism is primarily responsible for renal autoregulation in maintaining stable blood flow to the kidneys?
Which mechanism is primarily responsible for renal autoregulation in maintaining stable blood flow to the kidneys?
What initial change occurs in cardiovascular parameters when salt is accumulated in the body?
What initial change occurs in cardiovascular parameters when salt is accumulated in the body?
Which of the following best describes the changes that occur during the initial phase of volume-loading hypertension?
Which of the following best describes the changes that occur during the initial phase of volume-loading hypertension?
What influence does removing 35-45% of left kidney tissue have on arterial pressure?
What influence does removing 35-45% of left kidney tissue have on arterial pressure?
How does prolonged sodium intake affect peripheral resistance over time?
How does prolonged sodium intake affect peripheral resistance over time?
In the development of volume-loading hypertension, which of the following occurs after acute changes?
In the development of volume-loading hypertension, which of the following occurs after acute changes?
What is the response of the kidneys when excess fluid volume is present in the body?
What is the response of the kidneys when excess fluid volume is present in the body?
What is the equilibrium point in relation to long-term arterial pressure control?
What is the equilibrium point in relation to long-term arterial pressure control?
What happens to the mean arterial pressure when the renal output of salt and water equals the intake?
What happens to the mean arterial pressure when the renal output of salt and water equals the intake?
What occurs when arterial pressure rises above the equilibrium point?
What occurs when arterial pressure rises above the equilibrium point?
What principle explains the kidneys' capacity to manage long-term arterial pressure?
What principle explains the kidneys' capacity to manage long-term arterial pressure?
What physiological phenomenon describes the kidneys excreting excess fluid when arterial pressure rises?
What physiological phenomenon describes the kidneys excreting excess fluid when arterial pressure rises?
How does the kidney respond to a significant increase in arterial pressure above normal levels?
How does the kidney respond to a significant increase in arterial pressure above normal levels?
At what arterial pressure does the urine output of a hagfish become essentially zero?
At what arterial pressure does the urine output of a hagfish become essentially zero?
What is the relationship between blood volume and arterial pressure in hagfish?
What is the relationship between blood volume and arterial pressure in hagfish?
What is the primary purpose of the renal urinary output curve?
What is the primary purpose of the renal urinary output curve?
What happens to arterial pressure when total peripheral resistance increases acutely?
What happens to arterial pressure when total peripheral resistance increases acutely?
Why does arterial pressure return to normal within a couple of days after an acute rise?
Why does arterial pressure return to normal within a couple of days after an acute rise?
What role do the kidneys play when there is an increase in arterial pressure?
What role do the kidneys play when there is an increase in arterial pressure?
What primarily causes hypertension when total peripheral resistance increases?
What primarily causes hypertension when total peripheral resistance increases?
What happens to the equilibrium point for blood pressure control when vascular resistance is increased elsewhere in the body?
What happens to the equilibrium point for blood pressure control when vascular resistance is increased elsewhere in the body?
Which mechanism is primarily responsible for the kidneys' response to increased arterial pressure?
Which mechanism is primarily responsible for the kidneys' response to increased arterial pressure?
What occurs immediately after an acute increase in total peripheral resistance?
What occurs immediately after an acute increase in total peripheral resistance?
If vascular capacity does not increase, how can increased extracellular fluid volume affect arterial pressure?
If vascular capacity does not increase, how can increased extracellular fluid volume affect arterial pressure?
What is the eventual effect of the kidneys' response to a sustained increase in arterial pressure?
What is the eventual effect of the kidneys' response to a sustained increase in arterial pressure?
An increase in arterial pressure can cause the renal output of water to decrease.
An increase in arterial pressure can cause the renal output of water to decrease.
Pressure natriuresis refers to the increase in salt output in response to increased arterial pressure.
Pressure natriuresis refers to the increase in salt output in response to increased arterial pressure.
The renal-body fluid system for arterial pressure control acts quickly but is less powerful than other mechanisms.
The renal-body fluid system for arterial pressure control acts quickly but is less powerful than other mechanisms.
Fluid intake and output must be precisely unbalanced for long-term survival.
Fluid intake and output must be precisely unbalanced for long-term survival.
The renin-angiotensin mechanism is a significant refinement added to the renal-body fluid system over evolutionary stages.
The renin-angiotensin mechanism is a significant refinement added to the renal-body fluid system over evolutionary stages.
Drinking 0.9% saline solution instead of water significantly increases mean arterial pressure in dogs with removed renal tissue.
Drinking 0.9% saline solution instead of water significantly increases mean arterial pressure in dogs with removed renal tissue.
In volume-loading hypertension, total peripheral resistance decreases over time.
In volume-loading hypertension, total peripheral resistance decreases over time.
The kidneys play a role in controlling long-term arterial pressure by excreting excess fluid when arterial pressure is high.
The kidneys play a role in controlling long-term arterial pressure by excreting excess fluid when arterial pressure is high.
The removal of 35-45% of left kidney tissue has no impact on arterial pressure.
The removal of 35-45% of left kidney tissue has no impact on arterial pressure.
Secondary changes in circulatory function occur immediately after the development of volume-loading hypertension.
Secondary changes in circulatory function occur immediately after the development of volume-loading hypertension.
In the second stage of volume-loading hypertension, cardiac output is significantly lower than normal.
In the second stage of volume-loading hypertension, cardiac output is significantly lower than normal.
Total peripheral resistance is a primary cause of hypertension in volume-loading hypertension.
Total peripheral resistance is a primary cause of hypertension in volume-loading hypertension.
Volume-loading hypertension can occur in patients without any kidney function.
Volume-loading hypertension can occur in patients without any kidney function.
In volume-loading hypertension, hypertension is a result of increased cardiac output.
In volume-loading hypertension, hypertension is a result of increased cardiac output.
The second stage of volume-loading hypertension is characterized by low total peripheral resistance.
The second stage of volume-loading hypertension is characterized by low total peripheral resistance.
Hypertension in volume-loading hypertension develops before any peripheral resistance changes occur.
Hypertension in volume-loading hypertension develops before any peripheral resistance changes occur.
The typical techniques used to measure cardiac output are often unable to detect changes during the second stage of volume-loading hypertension.
The typical techniques used to measure cardiac output are often unable to detect changes during the second stage of volume-loading hypertension.
In individuals with volume-loading hypertension, elevated blood pressure and increased peripheral resistance typically occur together.
In individuals with volume-loading hypertension, elevated blood pressure and increased peripheral resistance typically occur together.
Cardiac output remains chronically elevated in patients experiencing volume-loading hypertension.
Cardiac output remains chronically elevated in patients experiencing volume-loading hypertension.
Progressive changes in circulatory variables during volume-loading hypertension are uncomplicated and linear.
Progressive changes in circulatory variables during volume-loading hypertension are uncomplicated and linear.
Match the following terms related to arterial pressure and kidney function:
Match the following terms related to arterial pressure and kidney function:
Match the following effects with the corresponding conditions:
Match the following effects with the corresponding conditions:
Match the following concepts in volume-loading hypertension:
Match the following concepts in volume-loading hypertension:
Match the following terms about renal response to arterial pressure changes:
Match the following terms about renal response to arterial pressure changes:
Match the following points on the arterial pressure–renal urinary output curve:
Match the following points on the arterial pressure–renal urinary output curve:
Match the following terms with their definitions in the context of arterial pressure control:
Match the following terms with their definitions in the context of arterial pressure control:
Match the following physiological processes with their functions:
Match the following physiological processes with their functions:
Match the following consequences with their respective triggers in blood pressure regulation:
Match the following consequences with their respective triggers in blood pressure regulation:
Match the following concepts with their significance in the renal–body fluid system:
Match the following concepts with their significance in the renal–body fluid system:
Match the following mechanisms with their descriptions:
Match the following mechanisms with their descriptions:
Flashcards
Stage 1 Volume-Loading Hypertension
Stage 1 Volume-Loading Hypertension
Increased blood volume leads to elevated cardiac output, resulting in high blood pressure.
Stage 2 Volume-Loading Hypertension
Stage 2 Volume-Loading Hypertension
Total peripheral resistance increases after hypertension develops and cardiac output returns to normal, sustaining high blood pressure.
Volume-Loading Hypertension: Mechanism
Volume-Loading Hypertension: Mechanism
Excess fluid accumulation raises blood pressure, initially increasing cardiac output, followed by autoregulation and increased total peripheral resistance.
Salt & Impaired Renal Function
Salt & Impaired Renal Function
Signup and view all the flashcards
Renin
Renin
Signup and view all the flashcards
Stimuli for Renin Release
Stimuli for Renin Release
Signup and view all the flashcards
RAAS
RAAS
Signup and view all the flashcards
Aldosterone
Aldosterone
Signup and view all the flashcards
Autoregulation Role
Autoregulation Role
Signup and view all the flashcards
Pressure diuresis
Pressure diuresis
Signup and view all the flashcards
Pressure natriuresis
Pressure natriuresis
Signup and view all the flashcards
Renal output curve
Renal output curve
Signup and view all the flashcards
Equilibrium point
Equilibrium point
Signup and view all the flashcards
Decreased arterial pressure
Decreased arterial pressure
Signup and view all the flashcards
Renin-Angiotensin system function
Renin-Angiotensin system function
Signup and view all the flashcards
Renal-body fluid systems long-term function
Renal-body fluid systems long-term function
Signup and view all the flashcards
Increase in extracellular fluid volume
Increase in extracellular fluid volume
Signup and view all the flashcards
Preeclampsia
Preeclampsia
Signup and view all the flashcards
JG cells
JG cells
Signup and view all the flashcards
Study Notes
Stages of Volume-Loading Hypertension
- Stage 1: Increased blood volume leads to elevated cardiac output, resulting in high blood pressure.
- Stage 2: Total peripheral resistance increases after hypertension develops. While cardiac output returns to normal, the increased resistance sustains the high blood pressure.
Volume-Loading Hypertension in Patients with No Kidneys
- Artificial Kidney Maintenance: When patients have no kidneys but are maintained with an artificial kidney, the increased blood pressure causes the kidneys to excrete excess fluid.
- Consequences: Over time, this leads to:
- Hypertension
- Increased total peripheral resistance
- Return of normal extracellular fluid volume, blood volume, and cardiac output
Volume-Loading Hypertension: Causes and Mechanisms
- Increased Fluid Volume: Excess fluid accumulation, potentially from drinking excessive fluids or consuming a salty diet, raises the blood pressure.
- Cardiac Output: The increased volume initially causes a rise in cardiac output, which directly contributes to the increased pressure.
- Autoregulation: Once the hypertension has developed, the body’s autoregulation mechanisms return the cardiac output to normal.
- Total Peripheral Resistance: This shift in cardiac output causes a secondary increase in total peripheral resistance, perpetuating the hypertension.
Consequences of Salt Intake and Renal function
- Salt Intake: Excess salt intake in individuals with healthy kidneys typically doesn’t lead to significant blood pressure elevation. This is due to the ability of the kidneys to quickly eliminate the extra salt.
- Impaired Renal Function: However, when kidney function is impaired, the excess salt accumulates in the body.
- Hormonal Effects: Excessive levels of antinatriuretic hormones, such as aldosterone, can also cause sodium retention and contribute to hypertension.
Renin Release and Pressure Regulation
- Renin Release: Renin is an enzyme released by the juxtaglomerular (JG) cells in the kidneys, which plays a key role in regulating blood volume and pressure.
- Stimuli for Renin Release:
- Decreased pressure in the kidney
- Decreased sodium chloride delivery to the macula densa cells in the distal tubule
- Increased sympathetic nervous system activity
Role of the Renin-Angiotensin-Aldosterone System (RAAS)
- RAAS: This system contributes to blood pressure regulation by influencing salt and water retention.
- Aldosterone: The mineralocorticoid hormone aldosterone, produced by the adrenal glands, stimulates sodium retention in the kidneys and plays a critical role in fluid balance.
- Hypertension: Excess aldosterone can lead to volume-loading hypertension by increasing blood volume.
Autoregulation and Tissue Blood Flow
- Autoregulation: Local tissues regulate their blood flow independently of the body’s overall circulatory needs. When blood flow increases, the tissue constricts blood vessels to maintain a stable flow.
- Systemic Effects: Increased blood volume causes increased flow to all tissues. If this flow exceeds the tissues’ metabolic needs, the autoregulation mechanism constricts blood vessels across the entire body. This systemic constriction contributes to increased total peripheral resistance.
Importance of Maintaining Normal Fluid Volume
- Dialysis Patients: In individuals with no kidneys, regular dialysis is crucial to maintain normal fluid volume and prevent hypertension.
- Volume Control: Without proper fluid volume control, these patients experience the same sequence of events as in volume-loading hypertension, starting with increased cardiac output followed by a secondary increase in peripheral resistance.
Blood Pressure and Fluid Volume
- Increased blood volume raises arterial pressure unless vascular capacitance also increases.
- Kidneys excrete excess volume to maintain normal pressure.
- Pressure diuresis: Increased urine output due to rising arterial pressure.
- Pressure natriuresis: Increased sodium output as arterial pressure rises.
Renal-Body Fluid System for Pressure Control
- Primitive pressure control in hagfish.
- Hagfish drink seawater, increasing blood volume and pressure.
- Kidneys excrete excess fluid to regulate pressure.
- System has evolved to include nervous system, hormones, and local control mechanisms.
Kidney Function and Arterial Pressure Control
- Renal output curve: Relates kidney's output of water and salt to arterial pressure.
- Equilibrium point: Intersection of renal output curve and intake curve; where output equals intake.
- Arterial pressure adjusts to reach the equilibrium point over time.
- Increasing total peripheral resistance can temporarily raise pressure, but kidneys will compensate.
Hypertension: Increased Fluid Volume
- Hypertension can occur when extracellular fluid volume rises.
- Initial cause: Increased cardiac output
- Secondary effect: Increased total peripheral resistance.
- High peripheral resistance hypertension is often the final result of increased fluid volume.
Hypertension: Excess Aldosterone
- Aldosterone excess can lead to hypertension due to sodium and water retention.
- Sodium and water retention further increases blood volume and pressure.
Renin-Angiotensin System and Blood Pressure
- Renin-Angiotensin System helps regulate blood pressure.
- Renin released by the kidneys due to:
- Decreased arterial pressure
- Decreased sodium chloride delivery
- Increased sympathetic nervous system activity
- Angiotensin II constricts renal arterioles, leading to:
- Reduced blood flow in kidneys
- Increased fluid reabsorption
- Angiotensin II stimulates aldosterone secretion, further increasing sodium and water retention.
- Renin-Angiotensin system plays a key role in short-term blood pressure regulation.
Renal-Body Fluid System for Arterial Pressure Control
- The renal-body fluid system is a powerful mechanism for long-term arterial pressure control.
- It acts slowly but effectively by regulating the balance between fluid intake and output.
- This system is crucial for maintaining homeostasis of body fluid volume.
- The kidneys, through local control systems, regulate the excretion of salt and water for long-term pressure regulation.
- An example of this system in action is the "pressure diuresis" phenomenon.
- A small increase in arterial pressure can double the renal output of water and salt.
- Humans, similar to hagfish, possess this essential renal-body fluid system for long-term arterial pressure control.
- Over time, the system has evolved with refinements, including the renin-angiotensin mechanism, making it more precise.
Quantitation of Pressure Diuresis and Arterial Pressure Control
- Studies involving volume-loading hypertension have provided valuable insights into long-term arterial pressure regulation.
- In these studies, excess salt and water intake lead to an increase in extracellular fluid volume.
- This excess fluid is gradually excreted, raising arterial pressure until the excess salt and water are eliminated.
- Experiments using dogs with partial nephrectomy (kidney removal) demonstrate the impact of renal function on arterial pressure.
- Removing 35-45% of the left kidney or the entire right kidney results in a significant increase in arterial pressure.
- This increase is sustained over several days, indicating the role of the kidneys in regulating long-term arterial pressure.
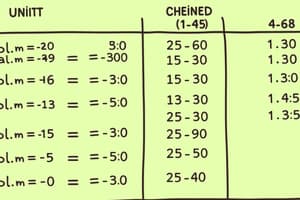
Sequential Changes in Circulatory Function During Volume-Loading Hypertension
- During the development of volume-loading hypertension, specific circulatory changes occur over time.
- Initially, there is an increase in extracellular fluid volume, leading to a rise in cardiac output and a slight decrease in total peripheral resistance.
- As the hypertension progresses, the cardiac output returns to near-normal levels, while total peripheral resistance progressively increases.
- This increase in total peripheral resistance is a secondary response to hypertension, not its cause.
Role of the Renin-Angiotensin System in Arterial Pressure Control
- The renin-angiotensin system is another powerful mechanism for regulating arterial pressure, complementing the kidneys' role in fluid balance.
- Renin, an enzyme released by the kidneys, activates the renin-angiotensin system when arterial pressure falls.
- This system helps restore pressure by increasing blood volume and constricting blood vessels.
Components of the Renin-Angiotensin System
- Renin is produced and stored in the juxtaglomerular cells (JG cells) of the kidneys.
- JG cells are specialized smooth muscle cells located in the walls of the afferent arterioles leading to the glomeruli.
- The renin-angiotensin system works through a series of steps:
- Renin converts angiotensinogen (a precursor protein) into angiotensin I.
- Angiotensin I is further converted into angiotensin II by an enzyme in the lungs.
- Angiotensin II, the active hormone, causes vasoconstriction, increases renal salt and water retention, and ultimately raises arterial pressure.
Hypertension in Preeclampsia
- Preeclampsia, also known as toxemia of pregnancy, is a complex condition characterized by high blood pressure.
- It affects 5% to 10% of expectant mothers and typically subsides after delivery.
- While the exact causes of preeclampsia are not fully understood, ischemia (lack of blood flow) to the placenta is believed to play a role.
- This placental ischemia releases toxic factors that can contribute to endothelial dysfunction.
- Endothelial dysfunction, in turn, impairs nitric oxide production, leading to vasoconstriction, decreased renal filtration, and impaired pressure natriuresis, ultimately contributing to hypertension.
Renal-Body Fluid System for Arterial Pressure Control
- Increase in arterial pressure above 150mm Hg causes a dramatic increase in renal output
- This increase in pressure above the equilibrium point, causes pressure diuresis
- Renal-body fluid system controls arterial pressure over long periods
- Increase in extracellular fluid volume increases blood volume, mean circulatory filling, venous return, cardiac output, ultimately leading to increased arterial pressure.
- Increase in arterial pressure causes increased renal excretion of salt and water
- Autoregulation controls blood flow
- Increases in cardiac output increase arterial pressure; one is direct increase in pressure; the other is an indirect effect of increasing peripheral vascular resistance.
Quantitation of Pressure Diuresis as a Basis for Arterial Pressure Control
- Pressure diuresis is the increase in renal output of water in response to increased arterial pressure
- Pressure natriuresis is the increase in renal output of salt in response to increased arterial pressure
- When pressure rises above the equilibrium point, renal output increases
- This system of pressure diuresis and natriuresis is fundamental to long-term arterial pressure control
Volume-Loading Hypertension
- Increasing extracellular fluid volume and blood volume can lead to hypertension
- The body regulates salt and water to control extracellular fluid volume
- Increasing sodium causes thirst and increases antidiuretic hormone (ADH) secretion
- Increases in ADH cause increased water reabsorption in the renal tubules, leading to reduced urine output and increased extracellular fluid volume.
- Volume-loading hypertension results from increased blood volume and increased arterial pressure
- Increased blood volume directly increases cardiac output, thus increasing pressure
- Increased blood volume also causes a rise in total peripheral resistance, which indirectly increases pressure
Hypertension in Preeclampsia (Toxemia of Pregnancy)
- Preeclampsia is a condition characterized by hypertension that develops during pregnancy
- It occurs in about 5-10% of pregnancies and often subsides after delivery
- Placental ischemia may trigger preeclampsia
- Placental toxicity may cause dysfunction of the vascular endothelium
- Endothelial dysfunction causes vasoconstriction, decreased glomerular filtration rate, impaired renal pressure natriuresis, and hypertension
Sequential Changes in Circulatory Function During Development of Volume-Loading Hypertension
- Volume-loading hypertension causes increased blood volume and cardiac output, leading to increased arterial pressure
- The kidneys eventually excrete the excess salt and water, returning arterial pressure to normal
- Ischemic kidney tissue releases renin, which can initiate a cascade of events, including vasoconstriction and increased arterial pressure
- When kidneys are ischemic, arterial pressure increases due to reduced pressure natriuresis and renin release
- In later stages of volume-loading hypertension, increased peripheral resistance and structural changes in nephrons are observed
- These structural changes contribute to sustained hypertension in these individuals.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.