Podcast
Questions and Answers
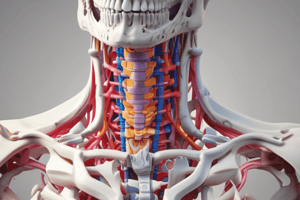
Which of the following anatomical structures provides stability to the vertebral column?
Which of the following anatomical structures provides stability to the vertebral column?
- Spinal ligaments (correct)
- Vertebral body
- Zygoapophyseal joints
- Transverse foramina
A 12-year-old boy sustains a forward flexion injury resulting in a fracture of T12 vertebral body. He was using a lap seat belt. Which of the following spinal fractures is most likely?
A 12-year-old boy sustains a forward flexion injury resulting in a fracture of T12 vertebral body. He was using a lap seat belt. Which of the following spinal fractures is most likely?
- Tear drop
- Clay-Shoveler's
- Burst fracture
- Chance fracture (correct)
A 31-year-old man comes to the clinic for pain in the right heel and lower back after a fall. Radiographs show a fracture of the calcaneus and the spine. Which of the spinal vertebral bodies is most likely fractured?
A 31-year-old man comes to the clinic for pain in the right heel and lower back after a fall. Radiographs show a fracture of the calcaneus and the spine. Which of the spinal vertebral bodies is most likely fractured?
- T11
- L2
- T12 (correct)
- L1
A 62-year-old woman is diagnosed with severe degenerative disease in the facet joints. Which of the following nerves is the likely cause of her pain?
A 62-year-old woman is diagnosed with severe degenerative disease in the facet joints. Which of the following nerves is the likely cause of her pain?
Which of the following anatomical structures is a continuation of the pia mater inferiorly and descends to the coccyx, anchoring the spinal cord?
Which of the following anatomical structures is a continuation of the pia mater inferiorly and descends to the coccyx, anchoring the spinal cord?
Which part of the spine is formed by the fusion of sacral vertebrae?
Which part of the spine is formed by the fusion of sacral vertebrae?
What is the primary function of the vertebral column?
What is the primary function of the vertebral column?
What contributes approximately 75% to the height of the vertebral column?
What contributes approximately 75% to the height of the vertebral column?
What is the most common abnormal curvature of the spine?
What is the most common abnormal curvature of the spine?
What is used to measure the Cobb angle in scoliosis?
What is used to measure the Cobb angle in scoliosis?
Which part of the spine forms an angle at the junction of L5 and the sacrum?
Which part of the spine forms an angle at the junction of L5 and the sacrum?
What structure separates the vertebrae and contributes approximately 25% to the height of the vertebral column?
What structure separates the vertebrae and contributes approximately 25% to the height of the vertebral column?
What is the primary role of the deep fascia in the back?
What is the primary role of the deep fascia in the back?
Which type of fracture is caused by violent forward flexion, resulting in a pure bony injury extending from posterior to anterior through the spinous processes, pedicles, and vertebral body?
Which type of fracture is caused by violent forward flexion, resulting in a pure bony injury extending from posterior to anterior through the spinous processes, pedicles, and vertebral body?
Which type of fracture is a stable fracture through the spinous process of a lower cervical or upper thoracic vertebra?
Which type of fracture is a stable fracture through the spinous process of a lower cervical or upper thoracic vertebra?
Which vertebrae have limited range of motion, with T12 being the most commonly fractured vertebra?
Which vertebrae have limited range of motion, with T12 being the most commonly fractured vertebra?
Which vertebrae have large bodies for support, and L5-S1 is a common site for disc degeneration and other spinal issues?
Which vertebrae have large bodies for support, and L5-S1 is a common site for disc degeneration and other spinal issues?
What can metastasize to the lumbar vertebrae via Batson's venous plexus?
What can metastasize to the lumbar vertebrae via Batson's venous plexus?
What causes loss of fluid contents, disruption of collagen and protein, resulting in abnormal motion and bony changes?
What causes loss of fluid contents, disruption of collagen and protein, resulting in abnormal motion and bony changes?
What is the inflammation of the vertebral disk space, often related to infection and diagnosed through MRI with contrast?
What is the inflammation of the vertebral disk space, often related to infection and diagnosed through MRI with contrast?
What is a surgical procedure to relieve pressure on the spinal cord or nerve roots, often due to herniated discs, bony hypertrophy, or tumors?
What is a surgical procedure to relieve pressure on the spinal cord or nerve roots, often due to herniated discs, bony hypertrophy, or tumors?
What in the lumbar region can cause pain with standing and walking and may require surgical decompression?
What in the lumbar region can cause pain with standing and walking and may require surgical decompression?
What separates adjacent vertebrae and acts as shock absorbers, with the nucleus pulposus providing elasticity and compressibility?
What separates adjacent vertebrae and acts as shock absorbers, with the nucleus pulposus providing elasticity and compressibility?
What is an unstable fracture/dislocation at the thoracolumbar junction, caused by a flexion/rotation injury?
What is an unstable fracture/dislocation at the thoracolumbar junction, caused by a flexion/rotation injury?
What is a common disc problem affecting the spine characterized by abnormal growth of bone in and around the discs?
What is a common disc problem affecting the spine characterized by abnormal growth of bone in and around the discs?
Which region of the vertebral column lacks transverse foramina and costal facets?
Which region of the vertebral column lacks transverse foramina and costal facets?
What type of joints permit gliding movements and can cause dermatomal pain with degenerative changes?
What type of joints permit gliding movements and can cause dermatomal pain with degenerative changes?
Which ligament plays a role in preserving normal spinal curvature and preventing abrupt flexion?
Which ligament plays a role in preserving normal spinal curvature and preventing abrupt flexion?
Which movements are permitted by the vertebral column?
Which movements are permitted by the vertebral column?
What is the approximate length of the spinal cord in adults?
What is the approximate length of the spinal cord in adults?
Which veins form within the vertebral bodies for venous drainage?
Which veins form within the vertebral bodies for venous drainage?
What do the spinal nerve roots and spinal meninges contain?
What do the spinal nerve roots and spinal meninges contain?
What do the meninges surround and protect?
What do the meninges surround and protect?
Where do spinal nerves exit the vertebral column?
Where do spinal nerves exit the vertebral column?
What is the arterial blood supply of the vertebrae primarily involve?
What is the arterial blood supply of the vertebrae primarily involve?
What type of branches supply bones, periosteum, ligaments, and meninges?
What type of branches supply bones, periosteum, ligaments, and meninges?
Which region of the spinal cord is enlarged for limb innervation?
Which region of the spinal cord is enlarged for limb innervation?
Which imaging position is recommended for assessing the degree of curvature in scoliosis films?
Which imaging position is recommended for assessing the degree of curvature in scoliosis films?
What is the primary role of the transverse ligament of the atlas in the cervical spine?
What is the primary role of the transverse ligament of the atlas in the cervical spine?
What is the distinctive feature of cervical vertebrae related to foramina in transverse processes?
What is the distinctive feature of cervical vertebrae related to foramina in transverse processes?
Which condition can cause severe arthritis in the upper cervical spine, leading to restricted neck rotation?
Which condition can cause severe arthritis in the upper cervical spine, leading to restricted neck rotation?
What is the pivotal joint visible in the 'open mouth' or 'water's view' X-ray?
What is the pivotal joint visible in the 'open mouth' or 'water's view' X-ray?
What is the primary purpose of the Risser classification in scoliosis assessment?
What is the primary purpose of the Risser classification in scoliosis assessment?
What is the function of the vertebral foramen in typical vertebrae?
What is the function of the vertebral foramen in typical vertebrae?
What is the primary cause for obtaining MRI in specific scoliosis cases?
What is the primary cause for obtaining MRI in specific scoliosis cases?
What is the primary purpose of the scoliometer in scoliosis assessment?
What is the primary purpose of the scoliometer in scoliosis assessment?
What condition can cause lateral tilt, listhesis of vertebral body, and sciatica in the context of spinal anatomy?
What condition can cause lateral tilt, listhesis of vertebral body, and sciatica in the context of spinal anatomy?
What are the landmarks on physical exam for assessing spinal anatomy?
What are the landmarks on physical exam for assessing spinal anatomy?
What is the primary characteristic of cervical vertebrae related to dislocation and fractures?
What is the primary characteristic of cervical vertebrae related to dislocation and fractures?
Which of the following regions is heavily reliant on ligaments for stability?
Which of the following regions is heavily reliant on ligaments for stability?
What is the primary cause of overuse inflammation often implicated in the greater trochanter?
What is the primary cause of overuse inflammation often implicated in the greater trochanter?
Which soft space is usually indicative of meniscal pathology?
Which soft space is usually indicative of meniscal pathology?
During puberty, the 3 main sections of the hip bone solidify via the triradiate cartilage and become the hip. Which sections are these?
During puberty, the 3 main sections of the hip bone solidify via the triradiate cartilage and become the hip. Which sections are these?
Which bone in the lower limb is mainly for muscle attachment and not weight-bearing?
Which bone in the lower limb is mainly for muscle attachment and not weight-bearing?
Which bone in the lower limb is encapsulated in tendon and articulates at the intercondylar groove of the femur?
Which bone in the lower limb is encapsulated in tendon and articulates at the intercondylar groove of the femur?
Which bone in the lower limb widens and flattens out proximally to form the tibial plateau?
Which bone in the lower limb widens and flattens out proximally to form the tibial plateau?
Which bone in the lower limb consists of the head, neck, and greater and lesser trochanters?
Which bone in the lower limb consists of the head, neck, and greater and lesser trochanters?
Which bone in the lower limb is a common site for fractures and has specific angles of inclination and torsion?
Which bone in the lower limb is a common site for fractures and has specific angles of inclination and torsion?
Which part of the lower limb consists of the talus, calcaneus, cuboid, navicular, and 3 cuneiforms?
Which part of the lower limb consists of the talus, calcaneus, cuboid, navicular, and 3 cuneiforms?
Which part of the lower limb consists of 5 metatarsals, with the 3rd metatarsal often implicated in stress fractures?
Which part of the lower limb consists of 5 metatarsals, with the 3rd metatarsal often implicated in stress fractures?
How many phalanges are there per foot, with the 1st toe having 2 and toes 2-5 having 3 each?
How many phalanges are there per foot, with the 1st toe having 2 and toes 2-5 having 3 each?
Which artery supplies various muscles and tissues in the thigh and gluteal area?
Which artery supplies various muscles and tissues in the thigh and gluteal area?
Which artery bifurcates into anterior and posterior tibial arteries, with specific clinical considerations for protection during total knee arthroplasty?
Which artery bifurcates into anterior and posterior tibial arteries, with specific clinical considerations for protection during total knee arthroplasty?
Where does lymph drainage of the lower limb run parallel to venous drainage, with superficial and deep divisions and clinical implications for lymphadenopathy?
Where does lymph drainage of the lower limb run parallel to venous drainage, with superficial and deep divisions and clinical implications for lymphadenopathy?
Which bone in the lower limb terminates as the medial and lateral femoral condyles, which articulate with the tibia to form the knee?
Which bone in the lower limb terminates as the medial and lateral femoral condyles, which articulate with the tibia to form the knee?
What is the largest nerve in the body that can be affected by posterior hip dislocation, causing symptoms like positive straight leg raise and tenderness in the sciatic notch?
What is the largest nerve in the body that can be affected by posterior hip dislocation, causing symptoms like positive straight leg raise and tenderness in the sciatic notch?
Which ligament complex in the ankle joint prevents inversion?
Which ligament complex in the ankle joint prevents inversion?
Which nerve is important clinically and its dysfunction can cause foot drop or indicate brain injury or cerebral disease?
Which nerve is important clinically and its dysfunction can cause foot drop or indicate brain injury or cerebral disease?
Which compartment syndrome in the leg is characterized by pain, pallor, paresthesia, paralysis, and pulselessness?
Which compartment syndrome in the leg is characterized by pain, pallor, paresthesia, paralysis, and pulselessness?
Which nerve supplies the dermatomes of the lower limb, with specific patterns illustrated in Figure 5.9?
Which nerve supplies the dermatomes of the lower limb, with specific patterns illustrated in Figure 5.9?
Which muscle is part of the posterior compartment of the leg?
Which muscle is part of the posterior compartment of the leg?
Which joint is primarily a hinge joint supported by ligaments and menisci?
Which joint is primarily a hinge joint supported by ligaments and menisci?
Which band extends from the tensor fascia lata and gluteus maximus, providing lateral support for the anterolateral thigh muscles?
Which band extends from the tensor fascia lata and gluteus maximus, providing lateral support for the anterolateral thigh muscles?
Which anesthesia is used for intraoperative anesthesia and post-operative pain control in lower limb procedures?
Which anesthesia is used for intraoperative anesthesia and post-operative pain control in lower limb procedures?
Which triangle in the thigh contains the femoral nerve, femoral artery, femoral vein, and deep inguinal lymph nodes?
Which triangle in the thigh contains the femoral nerve, femoral artery, femoral vein, and deep inguinal lymph nodes?
Which joint is a large, multiaxial ball-and-socket joint stabilized by ligaments and muscles?
Which joint is a large, multiaxial ball-and-socket joint stabilized by ligaments and muscles?
Which nerve, sural nerve, and plantar reflex are important clinically, with potential dysfunction causing foot drop or indicating brain injury or cerebral disease?
Which nerve, sural nerve, and plantar reflex are important clinically, with potential dysfunction causing foot drop or indicating brain injury or cerebral disease?
Which muscle is often harvested for transplantation due to its weakness as an adductor muscle?
Which muscle is often harvested for transplantation due to its weakness as an adductor muscle?
Which muscle group consists of semitendinosus, semimembranosus, and biceps femoris?
Which muscle group consists of semitendinosus, semimembranosus, and biceps femoris?
Which muscle is a superficial muscle of the posterior leg compartment?
Which muscle is a superficial muscle of the posterior leg compartment?
Which nerve innervates the medial thigh muscles, such as adductor longus, brevis, and magnus?
Which nerve innervates the medial thigh muscles, such as adductor longus, brevis, and magnus?
Which muscle is part of the anterior leg compartment?
Which muscle is part of the anterior leg compartment?
Which muscle is a hip flexor with specific origins, insertions, and actions?
Which muscle is a hip flexor with specific origins, insertions, and actions?
Which muscle is commonly referred to as the "hip pointer" when contused?
Which muscle is commonly referred to as the "hip pointer" when contused?
Which muscle group consists of four parts with distinct origins, insertions, and functions?
Which muscle group consists of four parts with distinct origins, insertions, and functions?
Which muscle is not part of the "hamstrings" group?
Which muscle is not part of the "hamstrings" group?
Which muscle is not a part of the lateral leg compartment?
Which muscle is not a part of the lateral leg compartment?
Which muscle is often used for transplantation due to its minimal impact on lower limb function?
Which muscle is often used for transplantation due to its minimal impact on lower limb function?
Which muscle is responsible for dorsiflexion and inversion of the foot?
Which muscle is responsible for dorsiflexion and inversion of the foot?
Which artery becomes the dorsalis pedis artery and feeds the dorsum of the foot?
Which artery becomes the dorsalis pedis artery and feeds the dorsum of the foot?
Which veins are formed by convergence of dorsal metatarsal, dorsal venous, and plantar venous networks in the leg?
Which veins are formed by convergence of dorsal metatarsal, dorsal venous, and plantar venous networks in the leg?
Which veins mimic the arterial system and run alongside major arteries in the lower extremity?
Which veins mimic the arterial system and run alongside major arteries in the lower extremity?
Which veins empty into the femoral and popliteal veins respectively?
Which veins empty into the femoral and popliteal veins respectively?
What is the primary cause of varicose veins according to the text?
What is the primary cause of varicose veins according to the text?
Where do the deep veins of the leg, including the anterior tibial, posterior tibial, and fibular veins, empty?
Where do the deep veins of the leg, including the anterior tibial, posterior tibial, and fibular veins, empty?
What is the primary function of the great and small saphenous veins?
What is the primary function of the great and small saphenous veins?
Which veins have a mirror venous complex that empties into the popliteal vein?
Which veins have a mirror venous complex that empties into the popliteal vein?
Which artery bifurcates into medial and lateral plantar arteries?
Which artery bifurcates into medial and lateral plantar arteries?
Which artery feeds the deep posterior compartment and lateral aspect of the leg?
Which artery feeds the deep posterior compartment and lateral aspect of the leg?
What do the deep and superficial networks in the foot work together to drain?
What do the deep and superficial networks in the foot work together to drain?
Which veins run alongside major arteries in the lower extremity?
Which veins run alongside major arteries in the lower extremity?
Flashcards are hidden until you start studying
Study Notes
Chief Characteristics and Anatomy of the Vertebral Column
- The vertebral column has distinct regional characteristics, including the presence of transverse foramina in cervical vertebrae and costal facets in thoracic vertebrae.
- Lumbar vertebrae lack transverse foramina and costal facets, and adjacent sacral vertebrae can fuse.
- The vertebral column has various joints, including symphyses between vertebral bodies, uncovertebral joints in the C3-C7 region, and facet joints that permit gliding movements and can cause dermatomal pain with degenerative changes.
- Ligaments like the ligamenta flava and anterior/posterior longitudinal ligaments play roles in preserving normal spinal curvature and preventing abrupt flexion.
- The vertebral column allows movements such as flexion, extension, lateral bending, and rotation, with specific muscles responsible for each movement.
- The arterial blood supply of the vertebrae involves segmental arteries supplying vertebral bodies, while spinal branches enter through IV foramina to supply bones, periosteum, ligaments, and meninges.
- Venous drainage parallels arterial supply and involves external and internal vertebral venous plexuses, with basivertebral veins forming within the vertebral bodies.
- Nerves of the vertebral column include medial branches, meningeal branches, and branches supplying periosteum, ligaments, and the spinal cord, contributing to the origin of back pain.
- The vertebral canal contains the spinal cord, spinal nerve roots, and spinal meninges with cerebrospinal fluid (CSF), including the dura, arachnoid, and pia mater.
- The spinal cord is approximately 42-45cm long in adults, extending from the foramen magnum to L1-L2 and enlarged in the cervical and lumbar regions for limb innervation.
- Spinal nerve roots emerge between specific vertebrae, and the spinal nerves exit the vertebral column through intervertebral foramina, forming mixed spinal nerves carrying motor and sensory fibers.
- The meninges, including the dura, arachnoid, and pia mater, surround and protect the spinal cord and nerve roots, containing CSF in the subarachnoid space and supporting the cauda equina.
Scoliosis and Spinal Anatomy Summary
- Scoliosis films should be done in a standing position to assess the degree of curvature, with attention to the heights of scapula and hemipelvis and measurement of truncal rotation with a scoliometer.
- The Risser classification grades skeletal maturity based on the level of ossification and fusion of the iliac crest apophyses, and MRI should be obtained in specific scoliosis cases, including rapid curve progression, unusual curve pattern, and neurologic deficit.
- Scoliosis can be degenerative, causing lateral tilt, listhesis of vertebral body, spinal stenosis, and sciatica.
- Landmarks on physical exam include the vertebra prominence, spinous process, L4-L5 disc space, and "dimples" of the posterior superior iliac spines.
- Typical vertebrae have various structures including spinous process, transverse process, lamina, superior articular facet, vertebral foramen, pedicle, and vertebral body.
- Cervical vertebrae are less tightly interlocked and more easily dislocated than fractured due to their horizontal facets.
- The C1-C2 articulation is a pivotal joint and visible in the "open mouth" or "water's view" X-ray.
- Cervical vertebrae have unique characteristics including foramina in transverse processes for the vertebral artery, with C1 as the atlas and C2 as the axis.
- Rheumatoid arthritis and psoriatic arthritis patients are prone to severe arthritis in the upper cervical spine, leading to restricted neck rotation.
- The transverse ligament of the atlas prevents spinal cord compromise by holding the dens of C2 in position and preventing displacement.
- Cervical spine distinctive features include the transverse foramen for vertebral arteries, veins, and large vertebral foramen accommodating cervical spinal nerves.
- Fractures like the burst fracture of C1, Jefferson or burst fracture, and cervical subluxation dislocations can lead to spinal cord compression and paralysis, with specific causes and mechanisms.
Muscles of the Hip and Leg Anatomy
- "Hip pointer" refers to a contusion at the origin, typically from contact sports
- Iliopsoas and iliacus are hip flexor muscles with specific origins, insertions, and actions
- Quadriceps femoris consists of four parts with distinct origins, insertions, and functions
- Medial thigh muscles, such as adductor longus, brevis, and magnus, are all innervated by the obturator nerve
- Gracilis is a weak adductor muscle and is often harvested for transplantation
- The "hamstrings" include semitendinosus, semimembranosus, and biceps femoris, which have dual actions
- Tibialis anterior, extensor hallucis longus, and extensor digitorum longus are muscles of the anterior leg compartment
- Fibularis tertius, longus, and brevis are muscles of the lateral leg compartment, each with specific actions and innervations
- Gastrocnemius is a superficial muscle of the posterior leg compartment with a specific origin and action
Anatomy of Lower Extremity Blood Vessels and Muscles
- The anterior tibial artery becomes the dorsalis pedis artery, feeding the dorsum of the foot and contributing to the plantar arch.
- The posterior tibial artery bifurcates into medial and lateral plantar arteries, feeding the posterior and lateral aspects of the leg and contributing to the knee.
- The fibula artery, a branch of the posterior tibial artery, also feeds the deep posterior compartment and lateral aspect of the leg.
- The venous return system mimics the arterial system, with deep and superficial systems running alongside major arteries.
- The deep and superficial networks in the foot work together to drain the soft tissue and structure.
- The great and small saphenous veins are formed by convergence of dorsal metatarsal, dorsal venous, and plantar venous networks in the leg.
- The great saphenous vein ascends anterior to the medial malleolus and empties into the femoral vein, while the small saphenous vein ascends posterior to the lateral malleolus and empties into the popliteal vein.
- Varicose veins are usually caused by valve incompetence between the deep venous and superficial circulation.
- The genicular arterial complex has a mirror venous complex that empties into the popliteal vein.
- The deep veins of the leg, including the anterior tibial, posterior tibial, and fibular veins, all empty into the popliteal vein in the popliteal fossa.
- The popliteal vein ascends and turns into the femoral vein proximal to the adductor hiatus, leading into the external iliac vein in the pelvis.
- Muscles of the gluteal region, including the gluteus maximus, gluteus medius, gluteus minimus, piriformis, and tensor of fascia lata, have specific origins, insertions, innervations, and actions.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.