Podcast
Questions and Answers
What are some clinical complications associated with mechanical ventilation?
What are some clinical complications associated with mechanical ventilation?
- VAP, sepsis, ARDS (correct)
- Liver failure, kidney stones, pancreatitis
- DVT, stroke, heart failure
- Hypertension, diabetes, anemia
Which ventilator mode allows the patient to breathe spontaneously between set ventilator breaths?
Which ventilator mode allows the patient to breathe spontaneously between set ventilator breaths?
- Assist-control (AC)
- Bi-level positive airway pressure (BiPAP)
- Pressure support (PS) (correct)
- Continuous positive airway pressure (CPAP)
What are some physiological complications associated with mechanical ventilation?
What are some physiological complications associated with mechanical ventilation?
- Atelectasis, pulmonary edema (correct)
- Migraine, insomnia
- Hemorrhage, embolism
- Osteoporosis, arthritis
Which of the following is NOT a preventive strategy for complications of mechanical ventilation?
Which of the following is NOT a preventive strategy for complications of mechanical ventilation?
What is a common complication that can increase morbidity and mortality in patients on mechanical ventilation?
What is a common complication that can increase morbidity and mortality in patients on mechanical ventilation?
Which ventilator mode provides a set number of breaths per minute at a set volume regardless of the patient's effort?
Which ventilator mode provides a set number of breaths per minute at a set volume regardless of the patient's effort?
What is the key factor that determines the choice of ventilator mode for a patient?
What is the key factor that determines the choice of ventilator mode for a patient?
Which setting can be adjusted to optimize oxygenation and ventilation in mechanically ventilated patients?
Which setting can be adjusted to optimize oxygenation and ventilation in mechanically ventilated patients?
What is a key parameter to monitor during regular patient assessments to identify complications early?
What is a key parameter to monitor during regular patient assessments to identify complications early?
Which tool provides valuable information on oxygenation, ventilation, and acid-base balance in mechanically ventilated patients?
Which tool provides valuable information on oxygenation, ventilation, and acid-base balance in mechanically ventilated patients?
Invasive ventilation with positive end-expiratory pressure (PEEP) is often used in which type of patients?
Invasive ventilation with positive end-expiratory pressure (PEEP) is often used in which type of patients?
Which collaboration among healthcare professionals can significantly improve patient outcomes in ventilator management?
Which collaboration among healthcare professionals can significantly improve patient outcomes in ventilator management?
Flashcards
Mechanical Ventilation
Mechanical Ventilation
Life-saving support, but carries the risk of complications like VAP and ARDS.
Ventilator Complications
Ventilator Complications
VAP, sepsis, ARDS, atelectasis and pulmonary edema
Ventilator-Associated Pneumonia (VAP)
Ventilator-Associated Pneumonia (VAP)
Infection of the lungs that occurs in patients on mechanical ventilation.
VAP Prevention
VAP Prevention
Signup and view all the flashcards
Ventilator Modes (AC, PS)
Ventilator Modes (AC, PS)
Signup and view all the flashcards
Key Ventilator Settings
Key Ventilator Settings
Signup and view all the flashcards
Noninvasive Ventilation
Noninvasive Ventilation
Signup and view all the flashcards
Patient Monitoring
Patient Monitoring
Signup and view all the flashcards
Arterial Blood Gas (ABG) Analysis
Arterial Blood Gas (ABG) Analysis
Signup and view all the flashcards
ABG Guided Adjustments
ABG Guided Adjustments
Signup and view all the flashcards
Effective Ventilator Management
Effective Ventilator Management
Signup and view all the flashcards
PEEP
PEEP
Signup and view all the flashcards
Study Notes
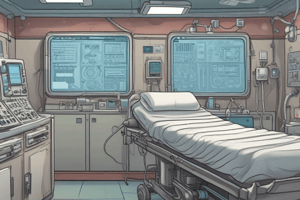
Ventilator Management: Complications Management, Ventilator Modes, Ventilator Settings, and Patient Assessment
Introduction
Mechanical ventilation is a critical life-saving intervention in the context of critical illness. However, it is associated with a risk of significant, potentially preventable complications. Among these are ventilator-associated pneumonia (VAP), sepsis, acute respiratory distress syndrome (ARDS), atelectasis, and pulmonary edema. These complications can increase morbidity and mortality, prolong the duration of mechanical ventilation, and extend the length of hospital stay or ICU stay, leading to increased healthcare costs.
Complications Management
Complications associated with mechanical ventilation can be categorized as clinical and physiological. Clinical complications include ventilator-associated pneumonia (VAP), sepsis, and ARDS, while physiological complications include atelectasis and pulmonary edema. Preventive strategies often involve multidisciplinary collaboration and a ventilator bundle approach, which generally comprises measures such as strict hand hygiene, chlorhexidine-impregnated endotracheal tubes, and a protocol for insertion and maintenance of endotracheal tubes.
Ventilator Modes
Different ventilator modes are available, including assist-control (AC), pressure support (PS), and continuous positive airway pressure (CPAP) modes. AC ventilation provides support for patients with impaired respiratory drive, while PS ventilation allows patients to breathe spontaneously with or without additional support. The choice of ventilator mode depends on the patient's respiratory status, the severity of the underlying condition, and the potential for complications.
Ventilator Settings
Ventilator settings can be adjusted to optimize oxygenation and ventilation, minimize complications, and improve patient outcomes. Key settings include inspiratory positive airway pressure (IPAP), expiratory positive airway pressure (EPAP), and peak inspiratory pressure (PIP). Invasive ventilation with positive end-expiratory pressure (PEEP) is often used in patients with acute respiratory failure, while noninvasive ventilation is a viable alternative for patients with less severe respiratory compromise.
Patient Assessment
Regular patient assessment is crucial to identify complications early and initiate appropriate interventions. Key parameters to monitor include oxygen saturation, respiratory rate, blood pressure, and hemodynamic stability. Patients should also be assessed for signs of infection, atelectasis, and barotrauma.
Abgs
Arterial blood gas (ABG) analysis is a valuable tool in the management of mechanically ventilated patients. It provides information on oxygenation, ventilation, and acid-base balance. ABG values can be used to adjust ventilator settings, monitor patient response to therapy, and identify potential complications such as VAP, ARDS, and metabolic imbalances.
Conclusion
Effective ventilator management involves a multifaceted approach, including optimizing ventilator modes and settings, monitoring patient status, and identifying and managing complications. Safe, effective strategies often require collaboration among healthcare professionals and can significantly improve patient outcomes and reduce healthcare costs.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.