Podcast
Questions and Answers
Which of the following is NOT a sign of inadequate breathing?
Which of the following is NOT a sign of inadequate breathing?
- Slow pulse (especially in children)
- Shallow or deep breathing
- Normal breath sounds (correct)
- Uneven chest movement
What is the primary purpose of a pressure regulator in oxygen therapy?
What is the primary purpose of a pressure regulator in oxygen therapy?
- To monitor the oxygen concentration delivered to the patient
- To increase the flow rate of oxygen to the patient
- To reduce the high pressure of the oxygen cylinder to a safe working pressure (correct)
- To control the level of humidity in the oxygen stream
Which oxygen delivery device is most appropriate for a patient with severe hypoxia who is breathing adequately?
Which oxygen delivery device is most appropriate for a patient with severe hypoxia who is breathing adequately?
- Nasal cannula
- Venturi mask
- Non-rebreather mask (correct)
- Partial rebreather mask
Which of the following is NOT a special consideration for airway management in children?
Which of the following is NOT a special consideration for airway management in children?
What does the term 'complete stoma' refer to in airway management?
What does the term 'complete stoma' refer to in airway management?
Which of the following is a common misconception about oxygen therapy?
Which of the following is a common misconception about oxygen therapy?
What is the typical range of oxygen flow rate (in liters per minute) delivered by a nasal cannula?
What is the typical range of oxygen flow rate (in liters per minute) delivered by a nasal cannula?
What is the main role of an EMT in an advanced airway management procedure?
What is the main role of an EMT in an advanced airway management procedure?
Which of the following is NOT a recommended practice for oxygen cylinder storage?
Which of the following is NOT a recommended practice for oxygen cylinder storage?
What is the difference between a 'partial rebreather mask' and a 'non-rebreather mask'?
What is the difference between a 'partial rebreather mask' and a 'non-rebreather mask'?
What is the correct frequency of ventilation for a patient who has been intubated?
What is the correct frequency of ventilation for a patient who has been intubated?
Which of the following is a sign of respiratory failure, as opposed to respiratory arrest?
Which of the following is a sign of respiratory failure, as opposed to respiratory arrest?
What is the primary function of a humidifier in oxygen therapy?
What is the primary function of a humidifier in oxygen therapy?
Why is it important to monitor oxygen levels closely in children receiving oxygen therapy?
Why is it important to monitor oxygen levels closely in children receiving oxygen therapy?
Which of the following is NOT a typical sign of inadequate breathing?
Which of the following is NOT a typical sign of inadequate breathing?
What is the recommended pulse oximetry reading for a patient at low altitude?
What is the recommended pulse oximetry reading for a patient at low altitude?
Which of the following can cause a ventilation/perfusion mismatch due to mechanical failure?
Which of the following can cause a ventilation/perfusion mismatch due to mechanical failure?
What is the primary function of the alveoli in the respiratory system?
What is the primary function of the alveoli in the respiratory system?
Which of the following is NOT a sign of respiratory distress?
Which of the following is NOT a sign of respiratory distress?
What is the difference between ventilation and respiration?
What is the difference between ventilation and respiration?
What happens during inhalation?
What happens during inhalation?
What is the term for the volume of air moved in and out with each breath?
What is the term for the volume of air moved in and out with each breath?
Which of the following is NOT a cause of gas exchange failure?
Which of the following is NOT a cause of gas exchange failure?
What is the body's primary way of compensating for low oxygen levels and high carbon dioxide levels?
What is the body's primary way of compensating for low oxygen levels and high carbon dioxide levels?
Flashcards
Respiratory Failure
Respiratory Failure
A condition where the body's compensation fails, leading to inadequate oxygenation.
Signs of Cyanosis
Signs of Cyanosis
Blue-gray discoloration indicating lack of oxygen in the blood.
Altered Mental Status
Altered Mental Status
Changes in mental state, including irritability, confusion, and disorientation.
Tripod Positioning
Tripod Positioning
Signup and view all the flashcards
Pulse Oximetry
Pulse Oximetry
Signup and view all the flashcards
Oxygen Therapy
Oxygen Therapy
Signup and view all the flashcards
Nasal Cannula
Nasal Cannula
Signup and view all the flashcards
Non-Rebreather Mask
Non-Rebreather Mask
Signup and view all the flashcards
Venturi Mask
Venturi Mask
Signup and view all the flashcards
Oxygen Cylinder Safety
Oxygen Cylinder Safety
Signup and view all the flashcards
Advanced Airway Placement
Advanced Airway Placement
Signup and view all the flashcards
Stoma Ventilation
Stoma Ventilation
Signup and view all the flashcards
Humidifiers in Therapy
Humidifiers in Therapy
Signup and view all the flashcards
Signs of Ineffective Breathing
Signs of Ineffective Breathing
Signup and view all the flashcards
Oxygen-Powered Ventilatory Devices
Oxygen-Powered Ventilatory Devices
Signup and view all the flashcards
Ventilation
Ventilation
Signup and view all the flashcards
Inhalation
Inhalation
Signup and view all the flashcards
Exhalation
Exhalation
Signup and view all the flashcards
Tidal Volume
Tidal Volume
Signup and view all the flashcards
Minute Volume
Minute Volume
Signup and view all the flashcards
Alveolar Ventilation
Alveolar Ventilation
Signup and view all the flashcards
Diffusion
Diffusion
Signup and view all the flashcards
Hypoxia
Hypoxia
Signup and view all the flashcards
Study Notes
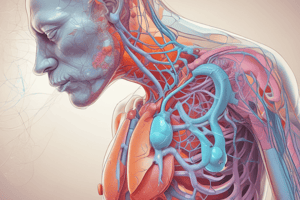
Ventilation and Respiration
- Ventilation: Process of moving air in and out of the lungs
- Inhalation/Inspiration: Chest muscles expand, diaphragm contracts pulling air into the lungs
- Exhalation/Expiration: Muscles relax, chest cavity decreases forcing air out
- Tidal Volume: Volume of air moved in and out with each breath
- Minute Volume: Total volume of air moved in and out per minute
- Alveolar Ventilation: Gas exchange occurs in the alveoli, where oxygen moves into the blood and carbon dioxide moves out
- Diffusion: Movement of gas from an area of high concentration to an area of low concentration
- Oxygen diffusion: From alveoli (21% oxygen) to blood cells (0% oxygen)
- Carbon Dioxide diffusion: From blood cells (higher concentration) to the alveoli
- VQ Mismatch: Ventilation/Perfusion mismatch occurs when one system fails, creating a mismatch and impacting oxygenation
- Mechanical Failure: Problems with chest movement, nerves, or airway
- Chest wall: Stab wounds, gunshot wounds, or painful injuries (fractured ribs)
- Nervous System: Damage to C3-C5 nerves that control the diaphragm
- Airway: Obstruction (asthma, bronchitis, pneumonia, COVID-19), foreign object
- Gas Exchange Failure: Insufficient oxygen in the air, mucus buildup, or damage to alveoli
- Circulatory Failure: Insufficient blood flow (anemia, blood clots, carbon monoxide poisoning, heart attack, stroke, pulmonary embolism)
- Mechanical Failure: Problems with chest movement, nerves, or airway
Respiratory Distress, Failure, and Arrest
- Hypoxia: Insufficient blood supply to tissues due to low oxygen levels or impaired gas exchange
- Hypercapnia: High levels of carbon dioxide in the blood
- Compensation: The body tries to compensate for low oxygen and high carbon dioxide to maintain homeostasis through increasing breathing rate, heart rate, and blood pressure.
- Respiratory Distress: Signs of compensation but with no apparent medical emergency.
- Respiratory Failure: When compensation fails
- Signs: Cyanosis, altered mental status, poor end-organ perfusion (e.g., weak pulse)
- Respiratory Arrest: Complete cessation of breathing
Signs of Inadequate Breathing
- Altered Mental Status: Irritability, confusion, disorientation
- Uneven Chest Movement: One side rising more than the other
- Slow Pulse: Especially in children
- Belly Breathing: Use of abdominal muscles to help breathe
- Muscle Retractions: Muscle pulling inwards around the clavicles and ribs during breathing
- Abnormal Breath Sounds: Wheezing, crowing (stridor), gurgling, gasping
- Fast or Slow Breathing: Below 8 or above 24 breaths per minute
- Shallow or Deep Breathing: Difficulty moving air in and out
- Cyanosis: Blue-gray discoloration of skin, lips, tongue, ears, nailbeds
- Inability to Speak in Complete Sentences:
- Tripod Positioning: Leaning forward with hands on knees, chest arched to improve breath capacity
- Pulse Oximetry: Less than 95% or less than 90% for those at altitude
Oxygen Therapy
- Oxygen is a Drug: Can be harmful in large doses for patients with heart conditions or stroke
- Use professional judgment: Assess patient's oxygen needs based on symptoms and pulse oximetry.
- Cardiac Arrest Patients: Most will need oxygen
- Oxygen Equipment: Must be safe, lightweight, portable, dependable, and compatible with various airway devices
- Oxygen Cylinders: Made from steel or aluminum alloy, available in D, E, and M sizes
- Green or Green with White: Indicates medical grade oxygen
- Pressure Regulators: Reduce high cylinder pressure to a safe working pressure (30 to 70 psi)
- Flow Meters: Control the oxygen flow rate (0.25 to 25 liters per minute).
- Pressure-compensated flow meter: Used in ambulances for constant flow
- Constant flow selector: Used with rescue bags
- Humidifiers: Add moisture to oxygen for patients in dry climates or those with extreme temperatures
- Used with long-term care patients or those on long transfers
- Oxygen Cylinders: Made from steel or aluminum alloy, available in D, E, and M sizes
- Oxygen Safety:
- Do not: Use welding oxygen, oil-based soaps, adhesive tape, or drag the cylinder
- Do: Store cylinders securely, cool, and well-ventilated, check for hydrostatic testing every five years, and open valves fully. Smoking Prohibited: Oxygen supports combustion
Oxygen Administration
- Nasal Cannula: Delivers 24-44% oxygen, used for mild hypoxia or patients who cannot tolerate masks.
- Non-Rebreather Mask: Delivers 80-90% oxygen, used for severe hypoxia with adequate breathing. Requires tight seal around the nose and face.
- Partial Rebreather Mask: Delivers 40-60% oxygen, not typically used in EMS
- Venturi Mask: Delivers specific oxygen concentration (e.g., 28%, 42%), used for patients with COPD
- Trach Mask: Provides oxygen for patients with tracheostomies
Special Considerations
- Facial Injuries: Ensure a secure airway, suction any fluids, utilize airway adjuncts (OPA, ET tube)
- Obstructions: Remove objects from the airway using suction, fingersweeps, or McGill forceps.
- Dentures: Leave them in place unless they become a hazard or if family members share them.
- Children:
- Large Tongues: Use tongue depressor to assist with airway management.
- Flexible Trachea: Be careful not to bend the trachea during airway manipulations.
- High Oxygen Consumption: Monitor closely, provide adequate ventilation and high oxygen concentrations.
- Oxygen-Powered Ventilatory Devices (Demand Valves):
- Provide high pressure ventilation
- Used for drowning victims or in specific system protocols. Do not use on children.
- Gastric Distension: Always monitor for signs of gastric distension during ventilation.
- Advanced Airway Placement:
- Paramedic Role: Placing advanced airways like endotracheal tubes
- EMT Role: Assist paramedic, holding airway tube in place, ensuring secure positioning, listening to chest and abdomen.
- Burping the Patient: Apply pressure to the cricoid cartilage to allow the paramedic to visualize the trachea.
- Ventilation After Intubation: Ventilate every 6 seconds, coordinate with chest compressions if CPR is in progress.
Stoma
- Complete Stoma: No air escapes from the mouth
- Partial Stoma: Air escapes through the mouth if the stoma is plugged
- Ventilation Through Stoma: Use a pediatric mask, ventilate directly into the trachea, ensure a neutral head position, and watch for chest rise and fall.
Key Takeaways
- Adequate Ventilation is Essential for Life
- EMTs are Critical in Airway Management
- Understanding Ventilation and Respiration is Crucial
- Be Safe with Oxygen
- Practice Makes Perfect: Practice airway management regularly.
- Stay Up-to-Date with Protocols: Know your local and system protocols for oxygen therapy and airway management.
- Work Together as a Team: EMTs and paramedics need to work as a cohesive unit to provide the best patient care.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.