Podcast
Questions and Answers
What primarily determines the color of urine?
What primarily determines the color of urine?
- The concentration of electrolytes
- The presence of dietary factors
- The pH level of the urine
- Breakdown products of red blood cell destruction (correct)
What does an increased presence of ketones in urine typically indicate?
What does an increased presence of ketones in urine typically indicate?
- The body is metabolizing carbohydrates effectively
- Kidney function is optimal
- Fat is being used as the primary energy source (correct)
- Excessive hydration is occurring
What role does the glomerulus play in the urinary system?
What role does the glomerulus play in the urinary system?
- It regulates blood pressure and pH
- It produces bile for secretion
- It is responsible for the composition of urine (correct)
- It synthesizes vitamin D
In what condition would nitrates in urine convert to nitrites, indicating a possible infection?
In what condition would nitrates in urine convert to nitrites, indicating a possible infection?
Which factor is NOT likely to affect the color of urine?
Which factor is NOT likely to affect the color of urine?
What is the primary function of the renal pyramids in the kidney?
What is the primary function of the renal pyramids in the kidney?
What structural feature of the kidney is responsible for the separation of glomerular capillaries and peritubular capillaries?
What structural feature of the kidney is responsible for the separation of glomerular capillaries and peritubular capillaries?
The medial surface of the kidney features a cleft known as what?
The medial surface of the kidney features a cleft known as what?
What is the composition of the nephron that facilitates the movement of glomerular filtrate?
What is the composition of the nephron that facilitates the movement of glomerular filtrate?
Which of the following accurately describes the blood flow sequence through the renal blood vessels?
Which of the following accurately describes the blood flow sequence through the renal blood vessels?
Flashcards
Urine Color
Urine Color
The color of urine is primarily determined by the breakdown products of red blood cell destruction.
Glomerulus Function
Glomerulus Function
The glomerulus is the first part of the nephron and is responsible for determining the composition of urine.
Ketones in Urine
Ketones in Urine
Ketones in urine indicate the body is using fat for energy instead of glucose.
Damaged Glomerulus
Damaged Glomerulus
Signup and view all the flashcards
Nitrates in Urine
Nitrates in Urine
Signup and view all the flashcards
Renal Sinus
Renal Sinus
Signup and view all the flashcards
Renal Pyramids
Renal Pyramids
Signup and view all the flashcards
Nephron Function
Nephron Function
Signup and view all the flashcards
Podocytes
Podocytes
Signup and view all the flashcards
Efferent Arteriole
Efferent Arteriole
Signup and view all the flashcards
Study Notes
Urinary System
- The urinary system cleanses the blood and eliminates wastes.
- It regulates pH and blood pressure.
- It plays a role in red blood cell concentration and vitamin D production.
- Urine color is primarily determined by the breakdown products of red blood cell destruction (urochrome).
- Liver heme, from hemoglobin, is converted to water-soluble forms and excreted in bile and urine.
- Urine color can be affected by liver disease, kidney stones, dehydration, and certain foods.
- Kidneys need to produce a minimum of 500ml of urine daily to eliminate waste.
- Urine pH typically ranges from 4.5 to 8.0 and is influenced by diet and disease.
- Specific gravity measures the concentration of solutes in urine.
Urine Characteristics
- Normal values:
- Color: Pale yellow to deep amber
- Odor: Odorless
- Volume: 750-2000 ml/24 hours
- pH: 4.5-8.0
- Specific gravity: 1.003-1.032
- Osmolarity: 40-1350 mOsmol/kg
- Urobilinogen: 0.2-1.0 mg/100 mL
- White blood cells: 0-2 HPF
- Leukocyte esterase: None
- Protein: None or trace
- Bilirubin: <0.3 mg/100 mL
- Ketones: None
- Nitrites: None
- Blood: None
- Glucose: None
Nephron Structure
- The nephron is the functional unit of the kidney.
- It has two major components: glomerulus and tubules.
- The glomerulus is a tuft of capillaries that filters blood, and the tubules are responsible for reabsorption and secretion.
- Filtration occurs in the glomerulus.
- The glomerulus and Bowman's capsule form the renal corpuscle.
- Tubules include proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct.
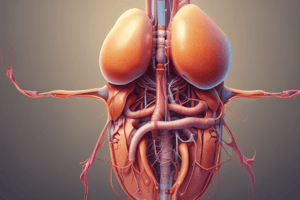
Renal Blood Flow
- The kidneys have two capillary beds: Glomerular and peritubular.
- The arrangement of these vessels helps regulate the hydrostatic pressures.
- The renal blood flow is regulated by the kidneys to maintain a constant glomerular filtration rate (GFR) despite changes in blood pressure.
Glomerular Filtration Rate (GFR)
- GFR is the volume of filtrate formed by both kidneys per minute.
- It's a crucial indicator of kidney function.
- Factors influencing GFR include net filtration pressure (NFP), hydrostatic and osmotic pressure and membrane surface area.
- Disruptions to GFR can lead to conditions like edema and altered urine volume.
Urine Formation
- Urine formation involves three main processes: filtration, reabsorption, and secretion.
- The glomerulus filters blood to form initial urine.
- Reabsorption is the process of reclaiming useful substances (water, glucose, amino acids).
- Tubular secretion removes unwanted substances from the blood into the filtrate.
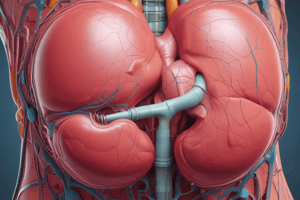
Kidney Anatomy
- Outer Cortex: Light-colored, granular appearance.
- Renal Pyramids: Cone-shaped structures in the medulla.
- Renal Pelvis: Funnel-shaped structure.
- Ureters: Tubes that carry urine from the kidneys to the bladder.
- Bladder: Stores urine until micturition.
- Urethra: Tube that transports urine from the bladder to the outside.
Types of Nephrons
- Cortical nephrons: Located mainly in the cortex, responsible for most of the glomerular filtration.
- Juxtamedullary nephrons: Located near the cortex-medullary junction, crucial for concentrating urine.
Tubular System Function
- Reabsorption and secretion of materials
- Reabsorption of water and solutes.
- Regulation of the filtrate, maintaining stable urine output
- The tubular system, including the proximal convoluted tubule, loop of Henle, and distal convoluted tubule, plays a major role in this process.
- It plays a critical role in maintaining homeostasis by regulating the composition and volume of urine, and regulating blood pressure and electrolyte balance.
Urinary System Regulation (e.g.: hormonal influences)
- The Renin-Angiotensin-Aldosterone System (RAAS) is a collection of hormones/enzymes that regulate blood pressure via multiple mechanisms.
- The hormone ADH (antidiuretic hormone) plays a role in regulating water balance.
- Other hormones and factors also influence urine production, including nitric oxide, prostaglandins, endothelin.
Additional Clinical Considerations
- GFR measurements and estimations are used to assess kidney function.
- Blood pressure has a direct relationship with GFR.
- Specific diseases and conditions (e.g. diabetes, kidney stones) can impact urine characteristics, production, and the urinary system.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.