Podcast
Questions and Answers
A patient is experiencing a psychological block to urinary elimination. Which nursing intervention is MOST appropriate to address this?
A patient is experiencing a psychological block to urinary elimination. Which nursing intervention is MOST appropriate to address this?
- Insert a urinary catheter to ensure bladder emptying.
- Administer a diuretic to stimulate urine production.
- Restrict fluid intake to reduce the urge to urinate.
- Encourage the patient to relax and provide privacy during attempts to void. (correct)
A patient reports experiencing burning during urination, increased urinary frequency, and lower abdominal discomfort. Which alteration in urinary elimination is the patient most likely experiencing?
A patient reports experiencing burning during urination, increased urinary frequency, and lower abdominal discomfort. Which alteration in urinary elimination is the patient most likely experiencing?
- Urinary retention
- Urinary diversion
- Urinary tract infection (UTI) (correct)
- Urinary incontinence
Which statement BEST describes the role of the urinary system in maintaining overall body homeostasis?
Which statement BEST describes the role of the urinary system in maintaining overall body homeostasis?
- The urinary system facilitates gas exchange between the blood and the atmosphere.
- The urinary system produces hormones that regulate blood sugar levels.
- The urinary system filters waste products from the blood and regulates fluid and electrolyte balance. (correct)
- The urinary system absorbs nutrients from digested food.
A patient's urine analysis reveals the presence of protein (proteinuria). Which structure of the urinary system is MOST likely impaired?
A patient's urine analysis reveals the presence of protein (proteinuria). Which structure of the urinary system is MOST likely impaired?
Which factor has the MOST direct impact on urine production?
Which factor has the MOST direct impact on urine production?
The functional unit of the kidney, responsible for filtration, is the:
The functional unit of the kidney, responsible for filtration, is the:
What physiological response is triggered by decreased blood supply to the kidneys?
What physiological response is triggered by decreased blood supply to the kidneys?
What is the primary function of the ureters?
What is the primary function of the ureters?
Why are females at a higher risk for urinary tract infections (UTIs) compared to males?
Why are females at a higher risk for urinary tract infections (UTIs) compared to males?
Normally, large proteins are not filtered by the glomerulus. What does the presence of large proteins in urine suggest?
Normally, large proteins are not filtered by the glomerulus. What does the presence of large proteins in urine suggest?
Which of the following is a direct effect of Angiotensin II?
Which of the following is a direct effect of Angiotensin II?
What condition can result from a ureter obstruction, such as a kidney stone?
What condition can result from a ureter obstruction, such as a kidney stone?
What is the role of erythropoietin, produced by the kidneys, in maintaining homeostasis?
What is the role of erythropoietin, produced by the kidneys, in maintaining homeostasis?
A patient with a ureterostomy (ileal conduit) requires education on managing their urinary diversion. Which of the following statements accurately describes the key aspects of this type of diversion?
A patient with a ureterostomy (ileal conduit) requires education on managing their urinary diversion. Which of the following statements accurately describes the key aspects of this type of diversion?
A patient is scheduled for the placement of nephrostomy tubes. What is the primary purpose of this intervention?
A patient is scheduled for the placement of nephrostomy tubes. What is the primary purpose of this intervention?
A nurse is assessing a patient with suspected urinary retention. After palpating the bladder, which of the following is the MOST appropriate next step?
A nurse is assessing a patient with suspected urinary retention. After palpating the bladder, which of the following is the MOST appropriate next step?
During an admission assessment, a patient reports nocturnal enuresis. Which of the following factors should the nurse consider as a potential contributing factor to this condition?
During an admission assessment, a patient reports nocturnal enuresis. Which of the following factors should the nurse consider as a potential contributing factor to this condition?
A nurse is caring for an elderly patient with urinary incontinence. What is the MOST important nursing intervention to prevent skin breakdown?
A nurse is caring for an elderly patient with urinary incontinence. What is the MOST important nursing intervention to prevent skin breakdown?
A patient reports a strong urge to urinate. Based on typical physiological responses, approximately how much urine has likely accumulated in their bladder?
A patient reports a strong urge to urinate. Based on typical physiological responses, approximately how much urine has likely accumulated in their bladder?
A nurse is caring for a postoperative patient who has not voided in 8 hours. Which action should the nurse prioritize to assess the patient's urinary function effectively?
A nurse is caring for a postoperative patient who has not voided in 8 hours. Which action should the nurse prioritize to assess the patient's urinary function effectively?
An elderly patient in a long-term care facility exhibits new onset confusion, fatigue, and a decline in function. The patient denies dysuria or frequency. Which of the following conditions should the nurse suspect?
An elderly patient in a long-term care facility exhibits new onset confusion, fatigue, and a decline in function. The patient denies dysuria or frequency. Which of the following conditions should the nurse suspect?
A patient is diagnosed with stress incontinence. Which intervention should the nurse prioritize to address this type of incontinence?
A patient is diagnosed with stress incontinence. Which intervention should the nurse prioritize to address this type of incontinence?
A patient with urinary retention is prescribed intermittent catheterization. What is the primary goal of this intervention?
A patient with urinary retention is prescribed intermittent catheterization. What is the primary goal of this intervention?
A nurse is preparing to insert an indwelling urinary catheter in a female patient. To minimize the risk of urinary tract infection (UTI), which of the following actions is most important?
A nurse is preparing to insert an indwelling urinary catheter in a female patient. To minimize the risk of urinary tract infection (UTI), which of the following actions is most important?
A patient with urge incontinence is being discharged. Which of the following instructions should the nurse include in the discharge teaching to help manage their condition?
A patient with urge incontinence is being discharged. Which of the following instructions should the nurse include in the discharge teaching to help manage their condition?
Which of the following catheter types is designed to be inserted through an incision in the lower abdomen, offering a long-term solution for bladder drainage while potentially reducing the risk of infection compared to other indwelling methods?
Which of the following catheter types is designed to be inserted through an incision in the lower abdomen, offering a long-term solution for bladder drainage while potentially reducing the risk of infection compared to other indwelling methods?
A patient with a long-term urinary catheter is being scheduled for routine maintenance. How often should the catheter be changed to minimize complications?
A patient with a long-term urinary catheter is being scheduled for routine maintenance. How often should the catheter be changed to minimize complications?
What is the primary purpose of using acetic acid for bladder irrigations in patients with urinary catheters?
What is the primary purpose of using acetic acid for bladder irrigations in patients with urinary catheters?
A post-operative patient with a urinary catheter is showing signs of bleeding in the bladder. What type of bladder irrigation is most appropriate for removing blood clots in this situation?
A post-operative patient with a urinary catheter is showing signs of bleeding in the bladder. What type of bladder irrigation is most appropriate for removing blood clots in this situation?
A patient with an indwelling urinary catheter develops a urinary tract infection (UTI). Besides administering antibiotics, what is a crucial nursing intervention to address the source of the infection?
A patient with an indwelling urinary catheter develops a urinary tract infection (UTI). Besides administering antibiotics, what is a crucial nursing intervention to address the source of the infection?
Which of the following strategies is most effective in preventing catheter-associated urinary tract infections (CAUTIs) in hospitalized patients, according to the Joint Commission's National Patient Safety Goals?
Which of the following strategies is most effective in preventing catheter-associated urinary tract infections (CAUTIs) in hospitalized patients, according to the Joint Commission's National Patient Safety Goals?
A patient with bladder cancer requires a urinary diversion. What is the key difference between a continent and an incontinent urinary diversion?
A patient with bladder cancer requires a urinary diversion. What is the key difference between a continent and an incontinent urinary diversion?
A patient is scheduled for an orthotopic neobladder procedure following a cystectomy. What is the primary benefit of this type of urinary diversion compared to other continent diversions?
A patient is scheduled for an orthotopic neobladder procedure following a cystectomy. What is the primary benefit of this type of urinary diversion compared to other continent diversions?
What would be the most appropriate action for a nurse to take when a patient with a urinary catheter reports sudden lower abdominal pain and bladder spasms?
What would be the most appropriate action for a nurse to take when a patient with a urinary catheter reports sudden lower abdominal pain and bladder spasms?
A patient's urinalysis results show a pH of 4.2. Which of the following is the most appropriate initial nursing action?
A patient's urinalysis results show a pH of 4.2. Which of the following is the most appropriate initial nursing action?
Following a cystography, a patient reports difficulty voiding and lower abdominal discomfort. Which of the following nursing interventions is most appropriate?
Following a cystography, a patient reports difficulty voiding and lower abdominal discomfort. Which of the following nursing interventions is most appropriate?
A patient's urine is noted to be tea-colored. Which of the following conditions might this finding indicate?
A patient's urine is noted to be tea-colored. Which of the following conditions might this finding indicate?
Which of the following instructions is most important for the nurse to provide to a patient scheduled for a renal angiogram?
Which of the following instructions is most important for the nurse to provide to a patient scheduled for a renal angiogram?
A nurse is caring for a patient with a urinary tract infection (UTI). Which urine characteristic is the nurse most likely to observe?
A nurse is caring for a patient with a urinary tract infection (UTI). Which urine characteristic is the nurse most likely to observe?
A patient undergoing diagnostic testing for urinary system dysfunction has a known iodine allergy. Which intervention is most important for the nurse to implement?
A patient undergoing diagnostic testing for urinary system dysfunction has a known iodine allergy. Which intervention is most important for the nurse to implement?
The nurse is reviewing urinalysis results. Which value requires immediate follow-up?
The nurse is reviewing urinalysis results. Which value requires immediate follow-up?
A nurse is caring for a patient post-pyelogram. Which assessment finding requires immediate notification of the healthcare provider?
A nurse is caring for a patient post-pyelogram. Which assessment finding requires immediate notification of the healthcare provider?
Flashcards
Urinary System Functions
Urinary System Functions
The urinary system's role includes regulating fluid balance, filtering blood, and eliminating waste through urine.
Gastrointestinal Organs
Gastrointestinal Organs
Gastrointestinal organs help in digestion and elimination of food waste, impacting overall urinary function.
Factors Impacting Urinary Elimination
Factors Impacting Urinary Elimination
Common factors affecting urinary elimination include hydration status, medications, and psychological factors.
Normal vs Abnormal Urine
Normal vs Abnormal Urine
Signup and view all the flashcards
Nursing Interventions
Nursing Interventions
Signup and view all the flashcards
Urinary Tract Organs
Urinary Tract Organs
Signup and view all the flashcards
Nephrons
Nephrons
Signup and view all the flashcards
Glomerulus
Glomerulus
Signup and view all the flashcards
Erythropoietin
Erythropoietin
Signup and view all the flashcards
Renin-angiotensin System
Renin-angiotensin System
Signup and view all the flashcards
Ureters
Ureters
Signup and view all the flashcards
Bladder
Bladder
Signup and view all the flashcards
Urethra Length
Urethra Length
Signup and view all the flashcards
Valsalva Technique
Valsalva Technique
Signup and view all the flashcards
Incontinent Urinary Diversion
Incontinent Urinary Diversion
Signup and view all the flashcards
Nephrostomy Tubes
Nephrostomy Tubes
Signup and view all the flashcards
Ureterostomy
Ureterostomy
Signup and view all the flashcards
Infection Control Principles
Infection Control Principles
Signup and view all the flashcards
Urge to urinate
Urge to urinate
Signup and view all the flashcards
Nurses’ role in urinary care
Nurses’ role in urinary care
Signup and view all the flashcards
Urinary retention
Urinary retention
Signup and view all the flashcards
Bladder scanner
Bladder scanner
Signup and view all the flashcards
Urinary tract infection (UTI)
Urinary tract infection (UTI)
Signup and view all the flashcards
CAUTI causes
CAUTI causes
Signup and view all the flashcards
Types of urinary incontinence
Types of urinary incontinence
Signup and view all the flashcards
Indwelling catheter
Indwelling catheter
Signup and view all the flashcards
Urinary Catheter Maintenance
Urinary Catheter Maintenance
Signup and view all the flashcards
Catheter Change Frequency
Catheter Change Frequency
Signup and view all the flashcards
Continuous Bladder Irrigation
Continuous Bladder Irrigation
Signup and view all the flashcards
Complications of Catheterization
Complications of Catheterization
Signup and view all the flashcards
CAUTI Prevention Measures
CAUTI Prevention Measures
Signup and view all the flashcards
Continent Urinary Reservoir
Continent Urinary Reservoir
Signup and view all the flashcards
Orthotopic Neobladder
Orthotopic Neobladder
Signup and view all the flashcards
Signs of Catheter Infection
Signs of Catheter Infection
Signup and view all the flashcards
Normal Urine pH
Normal Urine pH
Signup and view all the flashcards
Specific Gravity of Urine
Specific Gravity of Urine
Signup and view all the flashcards
Normal Urine Glucose Levels
Normal Urine Glucose Levels
Signup and view all the flashcards
Normal Urine WBC Count
Normal Urine WBC Count
Signup and view all the flashcards
Cloudy Urine
Cloudy Urine
Signup and view all the flashcards
Normal Urine Color
Normal Urine Color
Signup and view all the flashcards
Renal Imaging Techniques
Renal Imaging Techniques
Signup and view all the flashcards
Nursing Responsibilities in Urinary Tests
Nursing Responsibilities in Urinary Tests
Signup and view all the flashcards
Study Notes
Urinary Elimination
- Urinary elimination is a basic human function.
- It can be compromised by illness or certain procedures.
- Urination involves the bladder, urinary sphincter, and central nervous system (CNS).
- Most people experience a strong urge to urinate when the bladder holds approximately 400-600 milliliters of urine.
Class Objectives
- Reading: Fundamentals of Nursing, P&P, Chapters 46 & 47
- Explain the function and role of urinary system structures in urine formation and elimination. (CO 1)
- Understand factors that commonly impact urinary elimination. (CO 1,7)
- Know common alterations associated with urinary elimination. (CO 8)
- Interpret features of normal and abnormal urine. (CO 2)
- Be familiar with common diagnostic tests of the urinary system. (CO 1,2)
- Know the role of the gastrointestinal organs and their physiological function in digestion and elimination. (CO 1)
- Understand how psychological and physiological factors may alter the elimination process. (CO 4,5)
- Discuss Nursing interventions to promote normal elimination and reduce the issues.
Assigned Reading
- Pages 1255-1273 (This is lab content and does not need to be reviewed for this lecture.)
- Catheter insertion and straight catheter techniques are not required for this lecture.
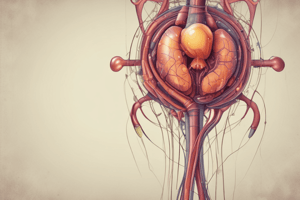
Urinary Tract Organs
- Urinary tract organs: Kidneys, Ureters, Bladder, Urethra
- Upper urinary tract: Kidneys and Ureters
- Lower urinary tract: Bladder and Urethra
Kidneys
- Nephrons are the functional units of the kidneys.
- Glomerulus act as a filter.
- Large proteins do not normally filter through the glomerulus.
- 99% of glomerular filtrate is reabsorbed.
- 1% of glomerular filtrate is excreted as waste.
- The kidneys play an essential role in erythropoietin production which stimulates red blood cell production and maturation in the bone marrow.
- Decreased blood supply triggers renin release, an enzyme that converts angiotensinogen into angiotensin I.
- Angiotensin I is converted to angiotensin II in the lungs.
- Angiotensin II stimulates aldosterone release, which increases water retention and increases blood pressure.
Ureters
- Function: Carry urine to the bladder.
- Urine is sterile.
- Obstruction (e.g., stone) can cause backflow, causing distention (hydronephrosis).
Bladder
- Distensible muscular organ that acts as a reservoir.
- Expands as it fills.
- Pressure is low during filling to prevent backflow and risk of infection.
Urethra
- Urine travels from bladder through the urethra.
- Female urethra is 3-4 cm (1-1.5 inches) – shorter length increases UTI risk.
- Male urethra is 18-20 cm (7-8 inches)
Nurse's Role in Urinary Elimination Management
- Urinary elimination is a basic human function.
- It can be compromised by illness and procedures.
- Most experience a strong urge to urinate when the bladder holds 400-600 milliliters of urine.
- Nurse's role: Assess urinary tract functions and support bladder emptying.
- Minimum hourly urinary output for an adult: Not specified.
Common Urinary Elimination Problems
- Urinary Retention: Accumulation of urine due to the inability of the bladder to empty. Check for post-void residual with bladder scanner.
- Urinary Tract Infection (UTI): Characterized by location (upper-kidney, lower-bladder or urethra). Bacteria are a primary cause of UTIs. E. coli is a common bacterial cause for UTIs.
UTI's (Urinary Tract Infections)
- What causes UTIs? CAUTIs, E. coli
- Who is at risk for UTIs? Elderly persons with atypical presentations, can have nonspecific symptoms, such as delirium, confusion, fatigue, loss of appetite, decline in function, incontinence, falls, temperature.
Urinary Incontinence
- Involuntary loss of urine. Common in older adults and elderly.
- Types of incontinence: transient, functional, overflow, stress, urge/urgency, reflex.
Urinary Catheterization
- When should a catheter be used?
- Minimize risk of infection: CDC infection control guidelines.
- More about healthcare associated infections (HAIs): CDC HAIS.
Urinary Catheterization Types
- Indwelling catheter (Foley): Balloon filled with water keeps one end inside the bladder.
- External female catheter (PureWick): (Video reference provided)
- Intermittent catheters (Straight catheters): Can be used several times a day at scheduled times or when the bladder feels full.
- Suprapubic catheter: Inserted through an incision in the lower abdomen; less risk of infection.
- Condom catheter: An option for some men.
Urinary Catheters
- Catheter changes every 4-6 weeks for long-term use.
- Closed drainage system.
- Catheter irrigations and installations.
- Acetic acid used to cleanse and irrigate inside the bladder.
- Continuous bladder irrigation: Flushes the bladder with normal saline to remove clots from bleeding during or after surgery.
Potential Complications of Urinary Catheterization
- Infection: Most common problem; bacteria from catheter can cause infection.
- Cues for monitoring infection: See page 19 for details.
- Other complications: Leaks, bladder spasms, pain, bladder stones/renal calculus, injury to urethra, kidney damage (with long-term use).
Nursing Measures to Prevent CAUTI
- The Joint Commission- National Patient Safety Goals (NPSG) - prevent inappropriate short-term catheter use, and timely removal of urinary catheters.
- Appropriate sterile technique during placement.
- Meticulous catheter care.
Urinary Diversions
- Types of diversions: temporary or permanent, continent or incontinent.
- Continent urinary reservoir: Catheter inserted into stoma to empty urine from pouch; requires catheterization 4-6 times a day.
- Orthotopic neobladder: Ileal pouch replaces the bladder in the same anatomical position; allows voiding through the urethra.
- Incontinent urinary diversion (Ureterostomy/Ileal conduit): Ureters come out the abdominal wall; no sensation of voiding. Nephrostomy tubes (posterior): Small tubes tunneled through the skin are used to drain the renal pelvis when the ureter is obstructed.
Knowledge Base
- Infection control and hygiene: Use infection control principles to help prevent the development and spread of UTIs.
- Growth and development (e.g., nocturnal enuresis, pregnancy, normal aging).
- Psychosocial implications (e.g., cultural influences, self-image, body image, sexuality).
Assessment
- Intake and output measurements: What should be included?
- Kidneys: Where are they located? Percuss for flank pain/costovertebral angle tenderness.
- Bladder: Palpate for distention, tenderness, and pain; use bladder scanner if retention is suspected.
- External genitalia and urethral meatus: Inspect for drainage, inflammation, swelling, rash, or lesions.
- Perineal skin: Inspect for erythema, skin erosion, itching, or burning pain.
Common Diagnostic Tests of Urinary System
- Urinalysis: Normal values: pH 4.6-8; Specific gravity 1.005-1.030; Glucose, Ketones, Blood, White Blood Cells (WBCs), Bacteria, Crystals.
- Imaging: Pyelogram, Cystography, CT scan, Ultrasound, Prostate/rectal sonogram, Renal angiogram.
Recognize Features of Normal and Abnormal Urine
- Color: Normal is pale straw to amber; Red, pink, or tea-colored urine is usually abnormal and can be caused by certain medications.
- Clarity: Normally transparent; Cloudy or milky urine can be a sign of infection.
- Odor: Characteristic ammonia smell; can be stronger when urine stands. Foul odor is abnormal.
Nursing Responsibilities
- Provide education about: laboratory procedures, specimen handling, infection control policies, diagnostic evaluations, patient care, and preventing potential complications.
- Diagnostic examinations: Obtaining informed consent, assessing for allergies (iodine or contrast dye), adherence to specific diets (e.g., clear liquids), and monitoring I&O.
Evaluation
- Evaluate patient outcomes through patient's perspective (self-image, social interactions, sexuality, emotional status).
Safety Guidelines
- Follow principles of surgical and medical asepsis as indicated.
- Identify patients at risk for latex or povidone-iodine (Betadine) allergies and provide alternatives like chlorhexidine.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.