Podcast
Questions and Answers
What is the primary characteristic of acute urinary retention?
What is the primary characteristic of acute urinary retention?
- Involuntary leakage of urine during exertion.
- The sudden, strong urge to urinate followed by leakage.
- A persistent urge to urinate without complete bladder emptying.
- The inability to urinate despite a full bladder. (correct)
Which of the following conditions is NOT a typical cause of urinary retention?
Which of the following conditions is NOT a typical cause of urinary retention?
- Congenital Conditions (correct)
- Kidney Stones
- Medication Side Effects
- Urinary Tract Infection
A patient complains of involuntary urine leakage when sneezing. Which type of incontinence is MOST LIKELY?
A patient complains of involuntary urine leakage when sneezing. Which type of incontinence is MOST LIKELY?
- Urge incontinence
- Overflow incontinence
- Functional incontinence
- Stress incontinence (correct)
Overflow incontinence results from which of the following?
Overflow incontinence results from which of the following?
What is the primary cause of neurogenic bladder?
What is the primary cause of neurogenic bladder?
Which of the following is a common characteristic of spastic bladder?
Which of the following is a common characteristic of spastic bladder?
What is the significance of measuring residual urine after urination?
What is the significance of measuring residual urine after urination?
Which of the following is NOT a possible treatment for urinary incontinence?
Which of the following is NOT a possible treatment for urinary incontinence?
Which condition is characterized by a lesion in the lower motor neuron, resulting in urine pooling and incomplete bladder emptying?
Which condition is characterized by a lesion in the lower motor neuron, resulting in urine pooling and incomplete bladder emptying?
What is a common cause of urinary tract infections (UTIs), particularly in women?
What is a common cause of urinary tract infections (UTIs), particularly in women?
Which of the following is a typical sign or symptom of a urinary tract infection (UTI)?
Which of the following is a typical sign or symptom of a urinary tract infection (UTI)?
Which of these is a nursing intervention for a patient with a UTI?
Which of these is a nursing intervention for a patient with a UTI?
What is a distinctive characteristic of urethritis?
What is a distinctive characteristic of urethritis?
Which symptom is most characteristic of cystitis?
Which symptom is most characteristic of cystitis?
Which condition is described as a severe form of cystitis, causing significant bladder pain?
Which condition is described as a severe form of cystitis, causing significant bladder pain?
What is a common cause of prostatitis?
What is a common cause of prostatitis?
What is a primary treatment for prostatitis, regardless of whether the infection is acute or chronic?
What is a primary treatment for prostatitis, regardless of whether the infection is acute or chronic?
What clinical manifestation is particularly associated with Pyelonephritis?
What clinical manifestation is particularly associated with Pyelonephritis?
Which of the following is a common diagnostic test for pyelonephritis?
Which of the following is a common diagnostic test for pyelonephritis?
What can cause a urinary obstruction?
What can cause a urinary obstruction?
What is a potential consequence of prolonged hydronephrosis?
What is a potential consequence of prolonged hydronephrosis?
Which of these is NOT a clinical manifestation of a urinary obstruction?
Which of these is NOT a clinical manifestation of a urinary obstruction?
Which condition involves the dilation of the renal pelvis and calyces?
Which condition involves the dilation of the renal pelvis and calyces?
Flashcards
Urinary retention
Urinary retention
The inability to urinate despite needing to. It can be sudden (acute) or ongoing (chronic).
Chronic urinary retention
Chronic urinary retention
The inability to completely empty the bladder, even with a need to urinate.
Stress incontinence
Stress incontinence
Involuntary leakage of urine due to exertion, like coughing or lifting.
Urge incontinence
Urge incontinence
Signup and view all the flashcards
Overflow incontinence
Overflow incontinence
Signup and view all the flashcards
Neurogenic bladder
Neurogenic bladder
Signup and view all the flashcards
Spastic bladder
Spastic bladder
Signup and view all the flashcards
Flaccid bladder
Flaccid bladder
Signup and view all the flashcards
Urinary Tract Infection (UTI)
Urinary Tract Infection (UTI)
Signup and view all the flashcards
Urethritis
Urethritis
Signup and view all the flashcards
Cystitis
Cystitis
Signup and view all the flashcards
Interstitial Cystitis
Interstitial Cystitis
Signup and view all the flashcards
Prostatitis
Prostatitis
Signup and view all the flashcards
Pyelonephritis
Pyelonephritis
Signup and view all the flashcards
Urinary Obstruction
Urinary Obstruction
Signup and view all the flashcards
Hydronephrosis
Hydronephrosis
Signup and view all the flashcards
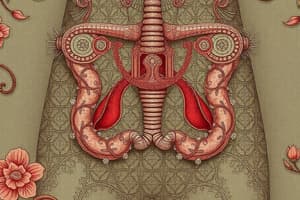
Urinary Control System
Urinary Control System
Signup and view all the flashcards
Urinary Incontinence
Urinary Incontinence
Signup and view all the flashcards
Bladder Training
Bladder Training
Signup and view all the flashcards
Study Notes
Urinary Retention
- Urinary retention is the inability to urinate despite having the urge.
- It can be acute or chronic.
- Acute retention is the complete inability to urinate despite a full bladder.
- Chronic retention is a persistent urge to urinate but an inability to empty the bladder completely.
- Causes include: stress, surgery involving the sphincter, kidney stones (calculi), infection, tumors, medication side effects, trauma (especially in women with rapid deliveries), and strictures.
- Urinary retention is painful and uncomfortable, leading to anxiety.
- A full bladder can feel like a baseball above the symphysis pubis.
- Patients with retention may be restless and irritable.
- Treatment typically involves a urinary catheter or surgical release of an obstruction.
- Analgesia and antispasmodics can assist with bladder relaxation.
- Post-void residual (PVR) urine is measured using a catheter.
- A PVR exceeding 50 milliliters suggests retention.
Urinary Incontinence
- Urinary incontinence is the involuntary leakage of urine.
- Types include:
- Stress incontinence: Leakage during exertion, like lifting or sneezing.
- Causes include: infection, loss of sphincter control, and pressure changes in the abdomen.
- Treatment options include: collagen implant injections and Kegel exercises.
- Urge incontinence: A sudden, strong urge to urinate resulting in leakage before reaching the bathroom.
- Overflow incontinence: Repeated inability to fully empty the bladder, leading to leakage because the bladder is overfull.
- Mixed incontinence: A combination of stress and urge incontinence.
- Functional incontinence: Incontinence due to a physical or mental impairment preventing timely access to the bathroom.
- Total incontinence: Complete, involuntary urine loss unresponsive to treatment.
- Treatment may involve temporary or permanent urinary diversion or management with an indwelling catheter.
- Stress incontinence: Leakage during exertion, like lifting or sneezing.
Neurogenic Bladder
-
Neurogenic bladder is the loss of voluntary control over urination, leading to retention or incontinence.
-
It arises from a lesion in the nervous system affecting bladder nerve pathways.
-
Causes include: congenital conditions, neurological disorders (like stroke), or trauma.
-
Types:
- Spastic bladder: Caused by a lesion above the voiding reflex (typically T12 or higher).
- Loss of sensation and motor control leads to bladder atrophy and decreased capacity.
- Urine release is reflexive, with little to no conscious control.
- Flaccid bladder: Caused by a lesion in the lower motor neuron (T12 to L1/L2).
- Results in urine pooling and incomplete bladder emptying due to lacking sensation.
- Patients may be unaware of retention.
- Spastic bladder: Caused by a lesion above the voiding reflex (typically T12 or higher).
-
Treatment includes bladder training, self-stimulation (every 2 hours for emptying), and monitoring PVR.
-
Manifestations can include infections from retention, urinary reflux, diaphoresis (sweating), flushing, nausea, and infrequent voiding.
Urinary Tract Infection (UTI)
-
UTI is the presence of bacteria in the urinary tract.
-
Women are more prone due to a shorter urethra and potential fecal/vaginal contamination.
-
Causes include: improper catheterization, bladder obstruction, incomplete bladder emptying, decreased prostate secretions, sexual activity, diabetes, multiple sclerosis, spinal cord injury, and kidney disease.
-
Bacteria enter through the meatus, causing infection.
-
Symptoms:
- Urgency and frequency of urination.
- Burning during urination (dysuria).
- Microscopic or gross hematuria (blood in urine).
- Nocturia (nighttime urination).
- Asthenia (fatigue or weakness).
- Back pain, abdominal discomfort, perineal pain, and confusion, especially in the elderly.
- Urosepsis: Systemic infection from urinary products entering tissues, potentially life-threatening.
-
Nursing interventions:
- Monitor for drug interactions.
- Encourage hydration (at least 2,000 mL daily).
- Instruct patients to complete antibiotic course to prevent resistance.
- Soothe skin irritation with cornstarch, baking soda baths, or diluted vinegar.
- Implement an ash diet (high in fruits, vegetables, legumes) to maintain urine pH near 5.5.
- Educate patients on prevention:
- Frequent sanitary product changes during menstruation.
- Cotton underwear and avoiding irritating products.
- Wipe from front to back.
- Urinate before and after sexual activity.
- Adequate hydration.
- Proper catheter care and handwashing.
- Avoid powders near urethra.
Urethritis
- Urethritis is inflammation of the urethra.
- Can be associated with or without gonorrhea.
- It's an acute infection of the urethral mucous membrane, causing pus discharge and urination discomfort.
Cystitis
- Cystitis is bladder wall inflammation.
- Often associated with catheterization or fecal contamination.
- More common in women.
- Symptoms: dysuria, urinary frequency, nocturia, pyuria (pus in urine), and lower abdominal discomfort.
- Diagnosed via urinalysis and urine culture.
- Treatment: adequate hydration (2,000 mL daily), good perineal hygiene, early symptom treatment (urine dipsticks), and avoidance of urinary irritants (alcohol, tea, coffee, chocolate).
Interstitial Cystitis
- Interstitial cystitis is a severe bladder pain syndrome.
- Management often involves dietary modifications and avoidance of urinary irritants.
Prostatitis
- Prostatitis is inflammation/infection of the prostate gland.
- Frequently caused by bacteria ascending the urethra.
- Can also be non-bacterial, often involving urethral occlusion.
- Symptoms: burning sensations, discomfort in perineum, urethra, lower back, and abdomen; urinary frequency and urgency; edema causing urethral occlusion.
- Complications include epididymitis, pyelonephritis, and sepsis.
- Treatment involves broad-spectrum antibiotics (2 to 16 weeks), regardless of acute or chronic nature.
- Avoid sexual arousal and intercourse during acute phases for prostate rest.
Pyelonephritis
- Pyelonephritis is inflammation of kidney structures (renal pelvis, tubules, and interstitial tissue).
- Commonly caused by E. coli.
- Associated with pregnancy, other chronic conditions, catheterization, infection, obstruction, trauma.
- Kidney inflammation with congested blood vessels leading to pus formation.
- Clinical manifestations: chills, fever, fatigue, flank pain, costovertebral angle (CVA) tenderness.
- Diagnosis: urinalysis (bacteria, pus, blood, WBCs), urine culture, ultrasound (abnormalities, obstruction, hydronephrosis), IVP (obstruction or degenerative changes), and blood tests (BUN, creatinine).
- Treatment: high fluid intake, urinary analgesics, and antibiotics targeted to the cultured organism.
Urinary Obstruction
- Urinary obstruction can be caused by strictures, kinks, cysts, tumors, calculi, or enlarged prostate.
- Results in alterations in blood chemistry, infection, ischemia, and renal tissue atrophy.
- Clinical manifestations: frequent urination urge, pain, distended bladder, and dribbling urine.
- Diagnosis: KUB (X-ray), renal ultrasound, IVP, and blood tests.
- Treatment: indwelling catheter, pain management, anticholinergics, suprapubic catheterization, and stenting.
Hydronephrosis
- Hydronephrosis is dilation of the renal pelvis and calyces (cup-shaped structures of the kidney).
- Can be unilateral or bilateral.
- Causes: congenital conditions or urinary tract obstruction.
- Obstruction creates pressure, leading to functional or anatomical kidney damage.
- The renal pelvis and ureters dilate and hypertrophy.
- Prolonged hydronephrosis causes fibrosis and nephron damage leading to decreased function.
- Clinical manifestations: pain, nausea, vomiting, urinary frequency/urgency, trouble starting urine stream, dribbling urine, nocturia, dysuria, hematuria, decreased output, edema, palpable abdominal mass, bladder distention, tenderness over kidneys/bladder.
- Treatment: surgical intervention to relieve obstruction.
- Severe cases may require nephrectomy (kidney removal).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.