Podcast
Questions and Answers
What is the primary cause of PNS injuries?
What is the primary cause of PNS injuries?
- Disruption of the nerve due to fractured bone (correct)
- Disruption of the nerve due to laceration or crush injuries (correct)
- Infection of the nerve
- All of the above
What is the difference between partial and complete nerve lesions?
What is the difference between partial and complete nerve lesions?
- Partial lesions are less severe, complete lesions are more severe
- Partial lesions are more severe, complete lesions are less severe
- Partial lesions affect some fibres of a nerve, complete lesions affect all fibres (correct)
- Partial lesions affect all fibres of a nerve, complete lesions affect some fibres
What is Neuropraxia?
What is Neuropraxia?
- Severance of a nerve and its connective tissue coverings
- Prolonged severe compression or crush injury to a nerve
- Wallerian degeneration distal to the lesion site
- Compression of a nerve by internal or external forces (correct)
What happens in Axonotmesis?
What happens in Axonotmesis?
What is the outcome of Neurotmesis?
What is the outcome of Neurotmesis?
What is common in Axonotmesis and Neurotmesis?
What is common in Axonotmesis and Neurotmesis?
What can be a result of Neuropraxia?
What can be a result of Neuropraxia?
What is a common outcome of Axonotmesis and Neurotmesis?
What is a common outcome of Axonotmesis and Neurotmesis?
What happens to the regenerating nerve fibres if they grow to the wrong muscle or sensory receptor?
What happens to the regenerating nerve fibres if they grow to the wrong muscle or sensory receptor?
Why is massage and movement of the affected limb contraindicated up to 3 weeks post-surgery?
Why is massage and movement of the affected limb contraindicated up to 3 weeks post-surgery?
What is the purpose of sewing the epineurium back together during surgery?
What is the purpose of sewing the epineurium back together during surgery?
What happens to the nerve fibres during Wallerian degeneration?
What happens to the nerve fibres during Wallerian degeneration?
What is the rate of nerve regeneration?
What is the rate of nerve regeneration?
Why is a splint worn post-surgery?
Why is a splint worn post-surgery?
What is the outcome if the nerve did not regenerate successfully?
What is the outcome if the nerve did not regenerate successfully?
How long after reinnervation occurs before functional reflexes return?
How long after reinnervation occurs before functional reflexes return?
What is the anatomical origin of the radial nerve?
What is the anatomical origin of the radial nerve?
Which muscle is not innervated by the radial nerve?
Which muscle is not innervated by the radial nerve?
What is the sensory distribution of the radial nerve?
What is the sensory distribution of the radial nerve?
What is a common cause of radial nerve lesions at the axilla level?
What is a common cause of radial nerve lesions at the axilla level?
What is the purpose of a dorsal splint in radial nerve lesion rehabilitation?
What is the purpose of a dorsal splint in radial nerve lesion rehabilitation?
What is a characteristic sign of radial nerve lesion?
What is a characteristic sign of radial nerve lesion?
At which level can radial nerve lesions occur due to fractures?
At which level can radial nerve lesions occur due to fractures?
Why do motor and sensory branches of the radial nerve have different disability pictures?
Why do motor and sensory branches of the radial nerve have different disability pictures?
What is the median nerve often referred to as?
What is the median nerve often referred to as?
Which nerve roots are responsible for the median nerve?
Which nerve roots are responsible for the median nerve?
What is the primary function of the pronator teres muscle?
What is the primary function of the pronator teres muscle?
Which fingers receive sensory innervation from the median nerve?
Which fingers receive sensory innervation from the median nerve?
What is a characteristic sign of a median nerve lesion?
What is a characteristic sign of a median nerve lesion?
What is the result of autonomic dysfunction in a median nerve lesion?
What is the result of autonomic dysfunction in a median nerve lesion?
Why is hydrotherapy contraindicated in median nerve lesions until autonomic function returns?
Why is hydrotherapy contraindicated in median nerve lesions until autonomic function returns?
What is the 'benediction' sign in median nerve compression?
What is the 'benediction' sign in median nerve compression?
What is the primary purpose of splinting in median nerve injuries?
What is the primary purpose of splinting in median nerve injuries?
Where is the median nerve most commonly injured?
Where is the median nerve most commonly injured?
What is a common complication of median nerve injuries?
What is a common complication of median nerve injuries?
What is a characteristic of pain in causalgia?
What is a characteristic of pain in causalgia?
What is a common symptom of median nerve injuries?
What is a common symptom of median nerve injuries?
What is a motor function affected by median nerve injuries?
What is a motor function affected by median nerve injuries?
What is a sensory test used to assess median nerve injuries?
What is a sensory test used to assess median nerve injuries?
Why is it important to handle fragile tissue with care in median nerve injuries?
Why is it important to handle fragile tissue with care in median nerve injuries?
What is the anatomical origin of the ulnar nerve?
What is the anatomical origin of the ulnar nerve?
Which muscle is not innervated by the ulnar nerve?
Which muscle is not innervated by the ulnar nerve?
What is the characteristic sign of an ulnar nerve lesion?
What is the characteristic sign of an ulnar nerve lesion?
What is a common cause of ulnar nerve lesions at the elbow level?
What is a common cause of ulnar nerve lesions at the elbow level?
What is the sensory distribution of the ulnar nerve?
What is the sensory distribution of the ulnar nerve?
What is the motor function affected by an ulnar nerve lesion?
What is the motor function affected by an ulnar nerve lesion?
What is the purpose of splinting in ulnar nerve lesions?
What is the purpose of splinting in ulnar nerve lesions?
What is the nickname of the ulnar nerve?
What is the nickname of the ulnar nerve?
What is the primary aim of treatment in ulnar nerve compression?
What is the primary aim of treatment in ulnar nerve compression?
What is necessary to remove a splint after nerve repair?
What is necessary to remove a splint after nerve repair?
What is the purpose of active exercise in nerve injury treatment?
What is the purpose of active exercise in nerve injury treatment?
Why is early control of edema important in nerve injury treatment?
Why is early control of edema important in nerve injury treatment?
What can be a result of untreated edema in nerve injuries?
What can be a result of untreated edema in nerve injuries?
What is the purpose of vibrations and soothing stroking in nerve injury treatment?
What is the purpose of vibrations and soothing stroking in nerve injury treatment?
When should active strengthening exercises begin in nerve injury treatment?
When should active strengthening exercises begin in nerve injury treatment?
Why is it important for the client to be supervised during strengthening exercises?
Why is it important for the client to be supervised during strengthening exercises?
What is the benefit of performing massage BEFORE physiotherapy treatment?
What is the benefit of performing massage BEFORE physiotherapy treatment?
What is the 'benediction' sign in ulnar nerve compression?
What is the 'benediction' sign in ulnar nerve compression?
What is the benefit of massage in physio treatments?
What is the benefit of massage in physio treatments?
What is done before removing the splint?
What is done before removing the splint?
Why is rhythmic mobilization avoided?
Why is rhythmic mobilization avoided?
What is done to the unaffected antagonists?
What is done to the unaffected antagonists?
What is the purpose of holding the limb after splint removal?
What is the purpose of holding the limb after splint removal?
Why is lubricant used during treatment?
Why is lubricant used during treatment?
What is used to bring awareness to the affected area?
What is used to bring awareness to the affected area?
Why is joint health maintained during treatment?
Why is joint health maintained during treatment?
What is done after the splint is put back on?
What is done after the splint is put back on?
What is stimulated during neuronal pathway stimulation?
What is stimulated during neuronal pathway stimulation?
What is the most important thing to determine when assessing a client with a peripheral nerve injury?
What is the most important thing to determine when assessing a client with a peripheral nerve injury?
What is a common issue that clients with severe or disfiguring peripheral nerve lesions may experience?
What is a common issue that clients with severe or disfiguring peripheral nerve lesions may experience?
Why is it important to receive written permission to perform massage on a client with a peripheral nerve injury?
Why is it important to receive written permission to perform massage on a client with a peripheral nerve injury?
What is the normal two-point discrimination distance on the finger pads?
What is the normal two-point discrimination distance on the finger pads?
What is a potential complication of peripheral nerve injuries?
What is a potential complication of peripheral nerve injuries?
What is the purpose of palpation in assessing a client with a peripheral nerve injury?
What is the purpose of palpation in assessing a client with a peripheral nerve injury?
What is an important consideration when observing a client with a peripheral nerve injury?
What is an important consideration when observing a client with a peripheral nerve injury?
Why is it essential to contact the neurologist and physiotherapist when treating a client with a peripheral nerve injury?
Why is it essential to contact the neurologist and physiotherapist when treating a client with a peripheral nerve injury?
What is Erb's paralysis commonly referred to as?
What is Erb's paralysis commonly referred to as?
What is typically affected in Erb's paralysis?
What is typically affected in Erb's paralysis?
What is the position of the shoulder in Erb's paralysis?
What is the position of the shoulder in Erb's paralysis?
What is the outcome of Erb's paralysis if C7 is involved?
What is the outcome of Erb's paralysis if C7 is involved?
What is the position of the forearm in Erb's paralysis?
What is the position of the forearm in Erb's paralysis?
What is lost in Erb's paralysis?
What is lost in Erb's paralysis?
What is a complication of Erb's paralysis?
What is a complication of Erb's paralysis?
What is the dermatome affected in Erb's paralysis?
What is the dermatome affected in Erb's paralysis?
What is the common name for Klumpke's paralysis?
What is the common name for Klumpke's paralysis?
Which nerve roots are primarily affected in Klumpke's paralysis?
Which nerve roots are primarily affected in Klumpke's paralysis?
What is a characteristic sign of Horner's Syndrome?
What is a characteristic sign of Horner's Syndrome?
What is a common cause of Klumpke's paralysis?
What is a common cause of Klumpke's paralysis?
What is a function lost in Klumpke's paralysis?
What is a function lost in Klumpke's paralysis?
What is the primary aim of treatment in Klumpke's paralysis?
What is the primary aim of treatment in Klumpke's paralysis?
What is a sensory loss associated with Klumpke's paralysis?
What is a sensory loss associated with Klumpke's paralysis?
What is a complication of Klumpke's paralysis?
What is a complication of Klumpke's paralysis?
What should be avoided when working with clients with nerve lesions?
What should be avoided when working with clients with nerve lesions?
What is the primary focus when treating uncompromised muscles distal to the lesion?
What is the primary focus when treating uncompromised muscles distal to the lesion?
What should be considered when performing hydrotherapy on clients with nerve lesions?
What should be considered when performing hydrotherapy on clients with nerve lesions?
Why should joints be supported during treatment?
Why should joints be supported during treatment?
What is a concern when positioning and pillowing the affected limb?
What is a concern when positioning and pillowing the affected limb?
What should be avoided in the early stages of hydrotherapy for clients with nerve lesions?
What should be avoided in the early stages of hydrotherapy for clients with nerve lesions?
When can testing PR ROM of the affected muscles be performed?
When can testing PR ROM of the affected muscles be performed?
Why should the neck be kept in neutral during treatment?
Why should the neck be kept in neutral during treatment?
What is the primary location of compression in Carpal Tunnel Syndrome?
What is the primary location of compression in Carpal Tunnel Syndrome?
What is the most common neuropraxia of the upper limb?
What is the most common neuropraxia of the upper limb?
What is the floor of the carpal tunnel composed of?
What is the floor of the carpal tunnel composed of?
Which of the following is NOT a structure that passes through the carpal tunnel?
Which of the following is NOT a structure that passes through the carpal tunnel?
What is a common symptom of Carpal Tunnel Syndrome?
What is a common symptom of Carpal Tunnel Syndrome?
What is the proximal border of the carpal tunnel?
What is the proximal border of the carpal tunnel?
What can cause compression of the median nerve in the carpal tunnel?
What can cause compression of the median nerve in the carpal tunnel?
What is the result of untreated Carpal Tunnel Syndrome?
What is the result of untreated Carpal Tunnel Syndrome?
What is a common cause of pain in the forearm and shoulder in Carpal Tunnel Syndrome?
What is a common cause of pain in the forearm and shoulder in Carpal Tunnel Syndrome?
What is a possible weakness and atrophy of in long-standing Carpal Tunnel Syndrome?
What is a possible weakness and atrophy of in long-standing Carpal Tunnel Syndrome?
What is a contributing factor to Carpal Tunnel Syndrome?
What is a contributing factor to Carpal Tunnel Syndrome?
What can be used to relieve pain and altered sensation in Carpal Tunnel Syndrome?
What can be used to relieve pain and altered sensation in Carpal Tunnel Syndrome?
What can cause a decrease in canal space in Carpal Tunnel Syndrome?
What can cause a decrease in canal space in Carpal Tunnel Syndrome?
What is a differential diagnosis for Carpal Tunnel Syndrome?
What is a differential diagnosis for Carpal Tunnel Syndrome?
What can be a complication of long-standing Carpal Tunnel Syndrome?
What can be a complication of long-standing Carpal Tunnel Syndrome?
What is a possible cause of swelling in the Carpal Tunnel?
What is a possible cause of swelling in the Carpal Tunnel?
What is the primary function of the pronator teres muscle?
What is the primary function of the pronator teres muscle?
What can be a symptom of median nerve compression at the Pronator Teres muscle?
What can be a symptom of median nerve compression at the Pronator Teres muscle?
What is the primary goal of treatment for PNS?
What is the primary goal of treatment for PNS?
What is palpated to rule out trigger points which may mimic the condition or contribute to it?
What is palpated to rule out trigger points which may mimic the condition or contribute to it?
What is tested during Phalen's test?
What is tested during Phalen's test?
What is a contraindication for friction techniques?
What is a contraindication for friction techniques?
What is the purpose of wearing a wrist splint?
What is the purpose of wearing a wrist splint?
What is the frequency of treatment?
What is the frequency of treatment?
What is the focus of passive stretches?
What is the focus of passive stretches?
What is a medical treatment for PNS?
What is a medical treatment for PNS?
What is a characteristic sign of PNS?
What is a characteristic sign of PNS?
What is the purpose of remedial exercise and self-care?
What is the purpose of remedial exercise and self-care?
What is the result of compression of the median nerve as it passes through the carpal tunnel?
What is the result of compression of the median nerve as it passes through the carpal tunnel?
What is the roof of the carpal tunnel comprised of?
What is the roof of the carpal tunnel comprised of?
Which of the following structures pass through the carpal tunnel?
Which of the following structures pass through the carpal tunnel?
What is the usual presentation of carpal tunnel syndrome in terms of laterality?
What is the usual presentation of carpal tunnel syndrome in terms of laterality?
Which of the following digits is affected by paraesthesia and sensory deficit in carpal tunnel syndrome?
Which of the following digits is affected by paraesthesia and sensory deficit in carpal tunnel syndrome?
What should be observed during palpation and observation in relation to the thenar eminence?
What should be observed during palpation and observation in relation to the thenar eminence?
What is the purpose of Spurlings, Jacksons, and Maximum Cervical Compression tests?
What is the purpose of Spurlings, Jacksons, and Maximum Cervical Compression tests?
What is a common symptom of carpal tunnel syndrome?
What is a common symptom of carpal tunnel syndrome?
What is the outcome if carpal tunnel syndrome is left untreated?
What is the outcome if carpal tunnel syndrome is left untreated?
What is the goal of treatment in relation to the sympathetic nervous system (SNS)?
What is the goal of treatment in relation to the sympathetic nervous system (SNS)?
What is the floor of the carpal tunnel comprised of?
What is the floor of the carpal tunnel comprised of?
What is the purpose of Phalen's and Reverse Phalen's tests?
What is the purpose of Phalen's and Reverse Phalen's tests?
What should be avoided in cases of pregnancy and R.A. in flare up?
What should be avoided in cases of pregnancy and R.A. in flare up?
What is the purpose of remedial exercises and self-care in the treatment of carpal tunnel syndrome?
What is the purpose of remedial exercises and self-care in the treatment of carpal tunnel syndrome?
What is the purpose of wearing wrist splints, especially at night?
What is the purpose of wearing wrist splints, especially at night?
What should be considered first in the treatment of carpal tunnel syndrome?
What should be considered first in the treatment of carpal tunnel syndrome?
What is the purpose of frictions in the treatment of carpal tunnel syndrome?
What is the purpose of frictions in the treatment of carpal tunnel syndrome?
What should be watched for in cases of long-standing conditions or chronic pathologies?
What should be watched for in cases of long-standing conditions or chronic pathologies?
What is a common symptom of Carpal Tunnel Syndrome?
What is a common symptom of Carpal Tunnel Syndrome?
Which of the following is a cause of Carpal Tunnel Syndrome?
Which of the following is a cause of Carpal Tunnel Syndrome?
What is a characteristic of the pain in Carpal Tunnel Syndrome?
What is a characteristic of the pain in Carpal Tunnel Syndrome?
What is a possible weakness or atrophy in Carpal Tunnel Syndrome?
What is a possible weakness or atrophy in Carpal Tunnel Syndrome?
What is a differential diagnosis of Carpal Tunnel Syndrome?
What is a differential diagnosis of Carpal Tunnel Syndrome?
Why is Vitamin B6 important for Carpal Tunnel Syndrome?
Why is Vitamin B6 important for Carpal Tunnel Syndrome?
What is the significance of the sensory branch of the median nerve before it passes through the tunnel?
What is the significance of the sensory branch of the median nerve before it passes through the tunnel?
What is a common occupation that may lead to Carpal Tunnel Syndrome?
What is a common occupation that may lead to Carpal Tunnel Syndrome?
What is a contributor to Carpal Tunnel Syndrome?
What is a contributor to Carpal Tunnel Syndrome?
What is a possible treatment for Carpal Tunnel Syndrome?
What is a possible treatment for Carpal Tunnel Syndrome?
What is the purpose of Phalen's test?
What is the purpose of Phalen's test?
What is the primary goal of treatment for carpal tunnel syndrome?
What is the primary goal of treatment for carpal tunnel syndrome?
What is a contraindication for joint play in carpal tunnel syndrome treatment?
What is a contraindication for joint play in carpal tunnel syndrome treatment?
What is the recommended frequency of treatment for carpal tunnel syndrome?
What is the recommended frequency of treatment for carpal tunnel syndrome?
What is a remedial exercise used to treat carpal tunnel syndrome?
What is a remedial exercise used to treat carpal tunnel syndrome?
What is a medical treatment option for carpal tunnel syndrome?
What is a medical treatment option for carpal tunnel syndrome?
What is a goal of massage therapy in treating carpal tunnel syndrome?
What is a goal of massage therapy in treating carpal tunnel syndrome?
Why is hydrotherapy contraindicated in median nerve lesions until autonomic function returns?
Why is hydrotherapy contraindicated in median nerve lesions until autonomic function returns?
What is the primary function of the pronator teres muscle?
What is the primary function of the pronator teres muscle?
Which of the following muscles are innervated by the median nerve?
Which of the following muscles are innervated by the median nerve?
What is a characteristic of Pronator Teres Syndrome?
What is a characteristic of Pronator Teres Syndrome?
What can be felt in the palm of the hand in Pronator Teres Syndrome?
What can be felt in the palm of the hand in Pronator Teres Syndrome?
What is the purpose of palpation and observation in Pronator Teres Syndrome?
What is the purpose of palpation and observation in Pronator Teres Syndrome?
Which of the following tests is used to rule out Pronator Teres Syndrome?
Which of the following tests is used to rule out Pronator Teres Syndrome?
What is a common symptom of Pronator Teres Syndrome?
What is a common symptom of Pronator Teres Syndrome?
What is a characteristic of pain in Pronator Teres Syndrome?
What is a characteristic of pain in Pronator Teres Syndrome?
Flashcards are hidden until you start studying
Study Notes
Upper Limb Nerve Lesions
- PNS injuries often occur due to disruption of the nerve from fractured bone, laceration, or crush injuries.
- Nerve lesions can be partial (only some fibers affected) or complete (all fibers affected).
- The extent of sensory loss, motor loss, weakness, sensory impairment, autonomic dysfunction, and pain depends on the severity and location of the lesion.
Classification of Nerve Injuries
- Neuropraxia:
- Compression of a nerve causing local conduction impairment.
- No structural damage to axons.
- Symptoms include paresthesia, paresis, and dysesthesia.
- Autonomics remain unaffected.
- Prognosis is good if compression site is relieved.
- Axonotmesis:
- Prolonged severe compression or crush injury.
- Epineurial, perineurial, and epineurial tube remain intact.
- Wallerian degeneration distal to the lesion site.
- Motor losses, sensory losses, and autonomic dysfunction.
- Holding patterns present, and contracture formation possible.
- Prognosis is good due to intact endoneurial tube.
- Neurotmesis:
- Partial or complete severance of a nerve and its connective tissue coverings.
- Wallerian degeneration distal to the lesion site.
- Motor losses, sensory losses, and autonomic dysfunction.
- Holding patterns present, and contracture formation possible.
- Gap between proximal regenerating stump and distal connective tissue sheath.
- Surgical treatment necessary.
Wallerian Degeneration and Regeneration
- Wallerian Degeneration:
- Schwann cells and macrophages responsible for degeneration process.
- Begins 24-36 hours post-injury and occurs over several days.
- Regeneration:
- Occurs at a rate of approximately 1-2mm/day.
- Rate of regeneration slower further away from the cell body.
- Splints may be worn to prevent contracture formation and excessive stretch on affected tissues.
Reinnervation and Recovery
- Reinnervation:
- 18-day delay before innervation produces a contraction.
- Another five days for functional reflexes to return.
- Removal of Splint:
- Done with permission from the client's neurologist.
- Care taken not to traction the healing nerve.
- Splint removed to increase circulation, maintain ROM, stimulate flaccid muscles, and reduce contracture formation.
- Permanent Damage:
- Results when the nerve did not regenerate successfully.
- Judged by non-return of muscle bulk and function, and sensation losses.
- Therapist does not need to worry about tractioning the affected nerve at this point.
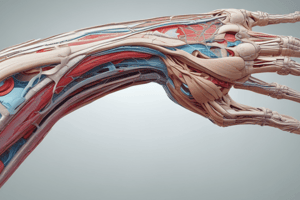
Radial Nerve Anatomy
- Originates from Posterior Cord fibers from C5, C6, C7, C8, T1 nerve roots
- Motor innervation to Extensor-Supinator group of muscles:
- Triceps and Anconeus
- Brachioradialis
- Extensor Carpi Radialis Longus and Brevis
- Extensor Digitorum
- Extensor Digiti Minimi
- Extensor Indicis
- Extensor Carpi Ulnaris
- Supinator
- Abductor Pollicis Longus
- Extensor Pollicis Brevis and Longus
- Sensory innervation to:
- Posterior arm
- Forearm
- Dorsum of the hand including the thumb, index, middle, and lateral half of the ring finger (excluding distal to the PIP’s)
Signs and Symptoms
- Disability picture:
- Sensory loss of the Radial nerve does not commonly result in dysfunction of the hand
- Motor loss results in:
- Wrist drop
- Pronation with the thumb in abduction
- Treatment:
- Dorsal splint provides wrist extension and thumb extension to protect the forearm extensors during the healing process
Causes of Radial Nerve Lesions
- Axilla:
- Posterior or inferior GH dislocations
- Compression (crutches)
- Saturday Night Palsy: compression prolonged positioning of the arm draped over the back of a chair
- Arm:
- Blows to posterior or lateral arm
- Fractures of humerus (mid-shaft, spiral groove)
- Elbows:
- Dislocations of the humeroradial or radioulnar joints
- Compression to the lateral arm from unrelieved pressure (e.g. poor positioning during surgery)
- Forearm:
- Gashing/Blocking injuries
- Fractures
- Wrist:
- Fractures
- Dislocations
- Severe sprains
- Hand:
- Branches may be damaged in various types of injuries to the thumb, 1st, and 2nd fingers, particularly dorsal injuries
- Note: Injuries affecting the radial nerve in the wrist or hand result only in sensory loss
Assessment Testing
- Motor:
- Wrist Extension
- Thumb Extension
- Sensory:
- Dorsal web space between thumb and index finger
Median Nerve Anatomy
- The median nerve is often referred to as the "eyes of the hand" due to its importance in providing sensory innervation to the palmar aspect of the hand.
- Nerve roots: Lateral Cord C5, C6, C7, Medial Cord C8, T1
- Motor innervation: Forearm flexors, pronators, and thenar eminence
- Supplies muscles including pronator teres, pronator quadratus, palmaris longus, flexor carpi radialis, and others
- Sensory innervation: Palmer surface of the thumb, index, middle, and lateral half of the ring finger, extending to the PIP's on the extensor surface
- Autonomic function: Carries autonomic function from the elbow to the hand, affecting sweat glands and vasomotor tone
Signs and Symptoms
- Disability picture: "Ape Hand" with wasting of the thenar eminence
- Thumb falls back in line with the fingers due to unopposed extensors and loss of function of palmaris longus
- Inability to oppose or flex thumb
- In high-level lesions, the wrist may deviate and flex to the ulnar side
- "Oath hand" presents when the client attempts to make a fist
- "Benediction" sign appears when the patient attempts to make a fist, but is not present with the hand open
Causes of Median Nerve Lesions
- Shoulder/arm: Direct trauma, some fractures
- Elbow: Fractures
- Forearm: Fractures (Colle's fracture), deep blows or gashes to the anterior forearm
- Wrist: Most common site of median nerve injury, suicide attempts, fractures of carpals, dislocations, contusions from a fall on the wrist, long-standing Carpal Tunnel Syndrome
- Hand: Palmer injuries to the thumb, 1st and 2nd fingers causing damage to specific branches
Complications
- Sensory loss can be very disabling, leading to avoidance of hand use due to lack of sensation
- Tissue dystrophy, edema, and poor circulation make the tissue extremely fragile, subject to injury, and poor healing
- Median nerve injuries are highly susceptible to Causaliga, a severe pain syndrome
- Causaliga symptoms: Sudden, intense burning pain, autonomic dysfunction, and muscle wasting
Assessment Testing
- Motor: Opposition of thumb, abduction of thumb
- Sensory: Distal 2nd and 3rd phalanges
Ulnar Nerve Anatomy
- Nerve roots: Medial cord C8, T1
- Motor innervation:
- Forearm: Flexor Carpi Ulnaris, medial 1⁄2 of Flexor Digitorum Profundus
- Hand: intrinsic muscles, hypothenar muscles, adductor pollicis
- Sensory innervation:
- Dorsal and palmar surfaces of the 5th digit and ulnar 1⁄2 of ring finger
- Ulnar side of the hand
Signs and Symptoms
- "Claw hand/hand of benediction" due to wasting of hypothenar eminence, interossei, and medial two lumbricals
- Loss of function of the pinky finger, hyperextended and abducted position
- Splinting prevents injury to the little finger
- Wrist may take on a slight radial deviation due to loss of Flexor Carpi Ulnaris
Causes
- Axilla/arm: Compression (crutch use)
- Elbow:
- Resting the elbow on a hard surface for prolonged periods
- Sleeping or poor positioning during surgery with the elbow flexed
- Contusion at the elbow or a severe blow to the elbow
- Dislocation or medial epicondyle fractures
- Forearm: Fractures, especially of the ulna, gashes, or protective blocking injuries
- Wrist:
- Wearing a wrist band that is too tight or handcuffs
- Resting wrist on handlebars with bicycling (competitive cyclists)
- Suicide attempt (may be combination lesion with median nerve)
- Fractures, dislocations, severe sprains (especially radial deviation sprains)
- Hand:
- Very susceptible to all types of hand and finger injuries
- Lacerations or contusions to the palm of the hand
Assessment Testing
- Motor: Little finger actions are lost, Froment's sign is positive
- Sensory: Ulnar aspect of little finger
Treatment
- Post-operative management following nerve repair:
- Immobilizing the hand in a position that minimizes tension on the nerve
- Complete immobilization for 2-3 weeks, followed by a program of protective stretching
- Aims and techniques:
- Contracture prevention
- Edema control
- Active exercise and strengthening
- Joint mobilizations and passive movement
- Massage for pain reduction and anxiety
- Splint removal: special consent, skin scan, and holding the limb to prevent traction on the healing nerve
- Example of a specific treatment:
- Positioning the client supine or side lying with the affected limb elevated
- Slow stroking and gentle compressions to the entire limb
- Lubricant application to prevent drag on flaccid tissues
- Effleurage and petrissage techniques with a block above the splint
- Segmental fascial work, gentle compressions, and tapping on affected tissues
- Inner-mid range ROM to maintain joint health
Remedial Exercise and Self-Care
- FDB and relaxation exercises
- Retrograde massage with an emollient cream to maintain tissue health, increase circulation, and decrease edema
- Education regarding awareness of limb and areas of altered sensation to prevent injury
- Encouraging the client to keep a progress chart to track rehabilitation progress
ERB'S & KLUMPKE'S PARALYSIS
- The client's symptom picture depends on which nerves or nerve root from a plexus has been ruptured, torn, cut, crushed, or stretched.
Peripheral Nerve Injuries
- Can be partial or complete, permanent or temporary
- Recovery, if it occurs, can take months or years and requires physiotherapy and the care of a neurologist
- Depression can become an issue for those recovering from severe or disfiguring peripheral nerve lesions
General Assessment Case History
- Includes general health, how the lesion occurred, areas of sensation loss or unusual sensations, past and current treatment, and results to date
- Require permission to contact M.D., neurologist, and physiotherapist
- If the nerve is regenerating, it is vital to contact the neurologist and physiotherapist to determine how far past the injury site the nerve has grown
- Receive written permission to perform massage
Supports, Braces, Splints
- Check if the splint can be removed for massage therapy
Emotional Status and Activities of Daily Living
- Observe antalgic gait or posture, pained facial expression, and autonomic dysfunction causing trophic changes to the skin and nails
- Deformity of the limb due to flaccid paralysis and paresis of one group of muscles causing contracture of the unopposed ones
Palpation
- Check for changes in temperature, tone, or texture of the skin
Testing
- Muscle Strength Grading
- Dermatome and Two-point discrimination test for affected dermatomes
- Normal two-point discrimination is 2-3 mm on the finger pads
- Inability to discriminate two points 10mm distant represents a severe impairment
- Tinel's Test (Sign)
- Tests a regenerating nerve to assess the degree of regeneration past the lesion site
- Begin tapping gently distally and continue to percuss proximally until the client indicates they feel a tingling or shock-like sensation
- This point represents the nerve generated so far
- Motor testing
- Test active free ROM
- Likely response will be flaccid paralysis or paresis depending upon the ROM tested
- If testing regenerating nerves, trace (minor) nerve conduction may be seen as a twitch or flicker of muscle contraction
ERB's Paralysis: C5-C6
- Also known as "Waiter's Tip Deformity" due to the characteristic arm position
- Typically involves unilateral traction injury to C5-C6 nerve roots, occasionally C7
- Most common presentation: complete/severe C5 involvement with incomplete C6 involvement
- In severe cases, C7 involvement can lead to weakness in wrist and finger extension
Characteristics
- Shoulder adducted and internally rotated
- Elbow extended
- Forearm pronated
- Wrist and fingers flexed
- Scapula protracted
Function Loss
- Shoulder abduction, external rotation, and forward flexion
- Elbow flexion
- Forearm supination
Function Weakened
- Shoulder adduction and internal rotation
- Scapular retraction and elevation
- Forearm pronation
- Wrist extension and abduction
- Finger extension
Sensory Loss
- Lateral arm and forearm (C5-C6 dermatome)
Causes
- Trauma in infants: baby pulled from birth canal with head in extension, rotation, and lateral flexion
- Trauma in adults: neck and shoulder separation during accidents (e.g., motorcycle, bike, skateboard crashes)
- Cervical rib compressing C5-C6 nerve roots
Complications
- Loss of rotator cuff muscles, deltoid, combined with sensory losses
- Shoulder/GH joint instability
- Frozen shoulder and osteoarthritis (OA)
Klumpke's Paralysis: C8-T1
- Also known as "Claw Hand" or "Rake Hand" due to clawed fingers and thumb lying in the same plane as the palm
- Caused by traction of the arm, avulsing the C8-T1 nerve roots
- T1 is generally more affected than C8
Autonomic Dysfunction
- May present like a median nerve lesion
- Can include traction of the proximal sympathetic chain, resulting in Horner's Syndrome
- Ipsilateral presentation of:
- Miosis (constriction of pupil)
- Ptosis (drooping eyelid)
- Enophthalmos (eyeball recedes into socket)
- Anhydrosis (loss of sweating on the ipsilateral face and neck)
- Ipsilateral presentation of:
Signs and Symptoms
- Fingers are clawed and pulled into extension and flexion by unopposed extensors
- Wrist is pulled into extension
- Thumb is pulled towards extension and abducted
- Wrist is extended, but some weak pronation may be possible
- Extension of MCP joints
- Tunneling between metacarpals is prominent
- Autonomic changes, including severe edema and trophic changes due to involvement of the median nerve
- Loss of sympathetic stimulation
- Horner's Syndrome
Functions Affected
- Lost:
- Wrist flexion
- Finger flexion, abduction, adduction
- Thumb flexion, adduction, opposition
- Weakened:
- Forearm pronation
- Wrist extension
- Finger extension
- Thumb extension and abduction
- Sensory loss in C8-T1 dermatomes, anteromedial arm, and 4th and 5th digits
Causes
- Fetal malpositioning during birth
- Falling from a height and grabbing onto something to break the fall
- Traction or overstretch of C8-T1 nerve roots
- Shoulder injury complications
- Cervical rib
Treatment Aims
- DO NOT INTERFERE WITH THE HEALING PROCESS
- DO NOT TRACTION THE REGENERATING NERVE
- Reduce unopposed contracture
- Maintain tissue health and circulation
- Maintain neuronal pathways (if nerve is regenerating)
- If lesion is permanent, encourage functional contracture and provide emotional support
- Treat compensatory posture and holding patterns
Techniques
- ALWAYS MAKE SURE THE NERVE IS NOT BEING TRACTIONED!
- Unaffected muscles proximal to lesion:
- Trigger Point treatment
- Manual lymphatic drainage
- Unopposed antagonist muscles distal to lesion:
- Modified fascial techniques
- Modified Swedish techniques
- Compromised muscles distal to lesion:
- Light stroking
- Gentle compressions
- Affected joints:
- Passive relaxed range of motion in direction that shortens the affected nerve and tissue
- Needs to be approved by neurologist before performing
Contraindications and Precautions
- Massage is contraindicated if causalgia is present
- Do not grasp flaccid or weak muscles
- Support all joints of the affected limb
- Do not perform rhythmic mobilizations as they may traction the nerve or make the client apprehensive
- Erb's and Klumpke's injuries occur from the neck, so keep the neck in neutral and avoid rotating the head
- Do not mobilize joints immediately above or below the regenerating nerve
- Testing PR ROM of affected muscles should only be performed once normal protective reflexes have been regained
- Hydrotherapy may need to be altered due to sensory impairment and possible vasomotor involvement
Carpal Tunnel Syndrome
- A compression/neuropraxia of the median nerve as it passes through the narrow carpal tunnel at the wrist, resulting in numbness and tingling along the median nerve distribution distal to the wrist.
- The median nerve is compressed between the transverse carpal ligament/flexor retinaculum of the hand, tendons that pass through the tunnel, and the bony carpals of the wrist.
- Carpal tunnel syndrome is the most common neuropraxia of the upper limb.
- If left untreated, it can lead to muscle wasting of the muscles of the thenar eminence and weakening of the grip of the hand.
Anatomy of the Carpal Tunnel
- The carpal tunnel is a narrow fibro-osseous opening through which several structures pass into the hand.
- The roof of the carpal tunnel is comprised of the dense transverse carpal ligament, which stretches across the wrist attaching to:
- The hook of hamate and the pisiform on the ulnar side of the hand
- The scaphoid tubercle and the trapezium on the radial side of the hand
- The floor of the carpal tunnel is made up of the carpal bones.
- Structures that pass through the tunnel include the median nerve, four tendons of flexor digitorum superficialis, four tendons of flexor digitorum profundus, and the tendon of flexor pollicis longus.
Signs and Symptoms of Carpal Tunnel Syndrome
- Usually unilateral presentation in the dominant hand, but can be bilateral with systemic edema.
- Paraesthesia and sensory deficit affecting only the 1st, 2nd, 3rd digit and lateral half of the 4th digit (volar aspect).
- Pain may occur in the wrist and/or palm with repetitive movements.
- Pain increases at night (as the wrist flexes during sleep).
- Possible weakness and atrophy of the thenar muscles controlling thumb abduction, flexion, and opposition.
Causes of Carpal Tunnel Syndrome
- Increase in carpal tunnel contents:
- Repetitive strain: Occupations that require repetitive wrist or finger flexion, or repeated wrist stabilization causing local tenosynovitis of the wrist flexors with resultant thickening and fibrosing.
- Trauma to the flexor retinaculum leading to scar tissue and thickening.
- Edema-related conditions such as pregnancy, premenstrual edema, diabetes.
- Decreased canal space:
- Bony callus (post wrist or carpal bone fracture).
- Ganglia, lipoma (fatty cysts), hematoma.
- Osteophytes due to arthritis, RA.
Contributors to Carpal Tunnel Syndrome
- Familial tendency (congenitally smaller shaped tunnel).
- Vitamin B6 deficiency, which can be treated with supplementation and found in various food sources.
Assessment and Differential Diagnosis
- Before the median nerve passes through the tunnel, it gives off a sensory branch that travels over the tunnel, supplying the base of the thenar eminence of the hand.
- Presentation is similar to a C6-7 radiculopathy, and examination of the c-spine is encouraged.
- Also rule out Pronator Teres Syndrome.
Pronator Teres Syndrome
- The median nerve can also be compressed at the Pronator Teres Muscle of the forearm.
- The median nerve passes (in most cases) between the heads of the Pronator Teres and is compressed with repetitive pronation/supination activities.
- Presentation is similar to that of Carpal Tunnel Syndrome, but with additional compromise of wrist, index, and middle finger flexion.
- Sensory disturbances (parasthesia) will also be felt in the palm of the hand.
Palpation and Observation
- Observe for muscle wasting of the thenar eminence and tissue changes to the fingers.
- Observe for edema over the wrist.
- Palpate muscles of cervical spine and shoulder (esp. Subscapularis) to rule out trigger points.
- Palpate for thickening, scarring, and adhesions of the Transverse Carpal Ligament (a.k.a. Flexor Retinaculum).
Testing
- Rule out the cervical spine, TOS, and pronator teres.
- Phalen's, Reverse Phalen's, Tinel's test at the wrist.
- AR Testing of the thenar muscles and grip strength.
Treatment Aims
- Decrease SNS firing and pain.
- Decrease edema that may be contributing to the condition.
- Decrease adhesions and scar tissue contributing to the condition.
- Decrease contributing hypertonicity and Trigger points in the shoulders and arms.
- Increase ROM and stretch the flexor retinaculum.
- Increase circulation.
- Increase joint and tissue health.
- Increase muscle strength of the thenar muscles.
- Reduce compensation.
Techniques
- Will be determined based on the symptoms and the root cause of the symptoms (carpal tunnel or pronator teres syndrome).
- Consider what is compressing on the median nerve and where:
- Scar tissue: consider frictions.
- Edema: consider MLD.
- Hypertonic muscle or Trigger points: consider myofascial release, petrissage, myofascial trigger point release, stretching techniques, etc.
Carpal Tunnel Syndrome
- A compression/neuropraxia of the median nerve as it passes through the narrow carpal tunnel at the wrist, resulting in numbness and tingling along the median nerve distribution distal to the wrist.
- The median nerve is compressed between the transverse carpal ligament/flexor retinaculum of the hand, tendons that pass through the tunnel, and the bony carpals of the wrist.
- Carpal tunnel syndrome is the most common neuropraxia of the upper limb.
- If left untreated, it can lead to muscle wasting of the muscles of the thenar eminence and weakening of the grip of the hand.
Anatomy of the Carpal Tunnel
- The carpal tunnel is a narrow fibro-osseous opening through which several structures pass into the hand.
- The roof of the carpal tunnel is comprised of the dense transverse carpal ligament, which stretches across the wrist attaching to:
- The hook of hamate and the pisiform on the ulnar side of the hand
- The scaphoid tubercle and the trapezium on the radial side of the hand
- The floor of the carpal tunnel is made up of the carpal bones.
- Structures that pass through the tunnel include the median nerve, four tendons of flexor digitorum superficialis, four tendons of flexor digitorum profundus, and the tendon of flexor pollicis longus.
Signs and Symptoms of Carpal Tunnel Syndrome
- Usually unilateral presentation in the dominant hand, but can be bilateral with systemic edema.
- Paraesthesia and sensory deficit affecting only the 1st, 2nd, 3rd digit and lateral half of the 4th digit (volar aspect).
- Pain may occur in the wrist and/or palm with repetitive movements.
- Pain increases at night (as the wrist flexes during sleep).
- Possible weakness and atrophy of the thenar muscles controlling thumb abduction, flexion, and opposition.
Causes of Carpal Tunnel Syndrome
- Increase in carpal tunnel contents:
- Repetitive strain: Occupations that require repetitive wrist or finger flexion, or repeated wrist stabilization causing local tenosynovitis of the wrist flexors with resultant thickening and fibrosing.
- Trauma to the flexor retinaculum leading to scar tissue and thickening.
- Edema-related conditions such as pregnancy, premenstrual edema, diabetes.
- Decreased canal space:
- Bony callus (post wrist or carpal bone fracture).
- Ganglia, lipoma (fatty cysts), hematoma.
- Osteophytes due to arthritis, RA.
Contributors to Carpal Tunnel Syndrome
- Familial tendency (congenitally smaller shaped tunnel).
- Vitamin B6 deficiency, which can be treated with supplementation and found in various food sources.
Assessment and Differential Diagnosis
- Before the median nerve passes through the tunnel, it gives off a sensory branch that travels over the tunnel, supplying the base of the thenar eminence of the hand.
- Presentation is similar to a C6-7 radiculopathy, and examination of the c-spine is encouraged.
- Also rule out Pronator Teres Syndrome.
Pronator Teres Syndrome
- The median nerve can also be compressed at the Pronator Teres Muscle of the forearm.
- The median nerve passes (in most cases) between the heads of the Pronator Teres and is compressed with repetitive pronation/supination activities.
- Presentation is similar to that of Carpal Tunnel Syndrome, but with additional compromise of wrist, index, and middle finger flexion.
- Sensory disturbances (parasthesia) will also be felt in the palm of the hand.
Palpation and Observation
- Observe for muscle wasting of the thenar eminence and tissue changes to the fingers.
- Observe for edema over the wrist.
- Palpate muscles of cervical spine and shoulder (esp. Subscapularis) to rule out trigger points.
- Palpate for thickening, scarring, and adhesions of the Transverse Carpal Ligament (a.k.a. Flexor Retinaculum).
Testing
- Rule out the cervical spine, TOS, and pronator teres.
- Phalen's, Reverse Phalen's, Tinel's test at the wrist.
- AR Testing of the thenar muscles and grip strength.
Treatment Aims
- Decrease SNS firing and pain.
- Decrease edema that may be contributing to the condition.
- Decrease adhesions and scar tissue contributing to the condition.
- Decrease contributing hypertonicity and Trigger points in the shoulders and arms.
- Increase ROM and stretch the flexor retinaculum.
- Increase circulation.
- Increase joint and tissue health.
- Increase muscle strength of the thenar muscles.
- Reduce compensation.
Techniques
- Will be determined based on the symptoms and the root cause of the symptoms (carpal tunnel or pronator teres syndrome).
- Consider what is compressing on the median nerve and where:
- Scar tissue: consider frictions.
- Edema: consider MLD.
- Hypertonic muscle or Trigger points: consider myofascial release, petrissage, myofascial trigger point release, stretching techniques, etc.
Pronator Teres Syndrome
- The median nerve can be compressed at the Pronator Teres Muscle of the forearm, leading to Pronator Teres Syndrome.
- The median nerve passes between the heads of the Pronator Teres and is compressed with repetitive pronation/supination activities.
- Presentation is similar to Carpal Tunnel Syndrome, but with additional symptoms:
- Compromised wrist, index, and middle finger flexion
- Sensory disturbances (parasthesia) in the palm of the hand
- Achy feeling over the anterior forearm
- Tenderness and pain with palpation and repetitive movements of the elbow at the proximal attachments of pronator teres
- No nocturnal symptoms are present in Pronator Teres Syndrome.
Palpation and Observation
- Observe for muscle wasting of the thenar eminence and tissue changes to the fingers.
- Observe for edema over the wrist.
- Palpate muscles of the cervical spine and shoulder (especially Subscapularis) to rule out trigger points.
- Palpate for hypertonicity and trigger points in the forearms from overuse.
- Palpate sensation over the palm of the hand (normal unless Pronator Teres is involved).
- Palpate for thickening, scarring, and adhesions of the Transverse Carpal Ligament (Flexor Retinaculum).
- Palpate for edema in the wrist and fingers.
- Palpate muscles of the thenar eminence for wasting.
Testing
- Rule out the cervical spine, TOS, and pronator teres using:
- Spurlings, Jacksons, Maximum Cervical Compression, Distraction
- Adson's, Halsteads/Allen's, Wright's Hyperabduction, Eden's
- Phalen's, Reverse Phalen's, Tinel's test at the wrist
- AR Testing of the thenar muscles and grip strength
Treatment
- Aims:
- Decrease SNS firing and pain
- Decrease edema and adhesions
- Increase ROM and stretch the flexor retinaculum
- Increase circulation and joint and tissue health
- Increase muscle strength of the thenar muscles
- Reduce compensation
- Long-term: Increase client awareness of good ergonomics, wrist and arm biomechanics, and posture
Techniques
- Determined based on symptoms and root cause of symptoms (carpal tunnel or pronator teres syndrome)
- Consider what is compressing on the median nerve and where:
- Scar tissue: consider frictions
- Edema: consider MLD
- Hypertonic muscle or trigger points: consider myofascial release, petrissage, myofascial trigger point release, stretching techniques, etc
Contraindications and Precautions
- Watch for fragile tissue that cannot withstand heavy fascial work or frictions
- Avoid joint play to the wrist in cases of pregnancy and R.A. in flare-up
- Don't friction if the client is on anti-inflammatories
- Don't use hydro (no heat or cold) while autonomic symptoms are not under control
Frequency and Remedial Exercise
- Treat in 1/2 hour sessions, 2-3 times weekly for 3 weeks
- Reassess and treat as required
- Remedial exercises:
- Hand Alphabet (have the client draw the alphabet in the air with hands)
- Passive stretches with a focus on extension of the wrist
- Neck and pectoral stretches
- Gentle squeezing or gripping exercises after surgery
- Avoid activities that increase symptoms if possible
- Appropriate hydrotherapy and elevation (if edema is a factor)
- Wrist and hand stretching
- Encourage use of wrist splint if advised by M.D.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.