Podcast
Questions and Answers
Which of the following best describes the primary function of microcirculation?
Which of the following best describes the primary function of microcirculation?
- To facilitate the exchange of nutrients, gases, and waste products between blood and tissues. (correct)
- To regulate systemic blood pressure through large arteries.
- To store large volumes of blood for use during emergencies.
- To transport blood directly from the heart to the major organs.
What is the primary structural component of capillaries that facilitates exchange?
What is the primary structural component of capillaries that facilitates exchange?
- Valves that control the direction of blood flow
- A single layer of endothelial cells (correct)
- Thick layers of smooth muscle
- Multiple layers of connective tissue
Which of the following is NOT a component of the microcirculatory system?
Which of the following is NOT a component of the microcirculatory system?
- Capillaries
- Venules
- Aorta (correct)
- Arterioles
What is the role of precapillary sphincters in the microcirculation?
What is the role of precapillary sphincters in the microcirculation?
What is the primary mechanism by which oxygen and carbon dioxide are exchanged across the capillary wall?
What is the primary mechanism by which oxygen and carbon dioxide are exchanged across the capillary wall?
How do water-soluble substances typically cross the capillary wall?
How do water-soluble substances typically cross the capillary wall?
What characteristic of proteins limits their movement across the capillary wall?
What characteristic of proteins limits their movement across the capillary wall?
According to the principles of diffusion, what primarily drives the movement of a solute across the capillary wall?
According to the principles of diffusion, what primarily drives the movement of a solute across the capillary wall?
What is the role of osmosis in fluid movement across the capillary wall?
What is the role of osmosis in fluid movement across the capillary wall?
What does 'tonicity' refer to in the context of fluid movement?
What does 'tonicity' refer to in the context of fluid movement?
According to the Starling equation, what forces influence fluid movement across capillary walls?
According to the Starling equation, what forces influence fluid movement across capillary walls?
Which of the following best describes capillary hydrostatic pressure?
Which of the following best describes capillary hydrostatic pressure?
What primarily determines the capillary oncotic pressure?
What primarily determines the capillary oncotic pressure?
What effect does increased capillary hydrostatic pressure have on fluid movement across the capillary wall?
What effect does increased capillary hydrostatic pressure have on fluid movement across the capillary wall?
What effect does a decrease in plasma protein concentration have on fluid movement across the capillary wall?
What effect does a decrease in plasma protein concentration have on fluid movement across the capillary wall?
What is the role of the lymphatic system in microcirculation?
What is the role of the lymphatic system in microcirculation?
What is edema?
What is edema?
Which condition is NOT a typical cause of edema?
Which condition is NOT a typical cause of edema?
What characterizes capillaries with 'tight' clefts, such as those found in the brain-blood barrier?
What characterizes capillaries with 'tight' clefts, such as those found in the brain-blood barrier?
Which Starling force opposes filtration in the capillaries?
Which Starling force opposes filtration in the capillaries?
What does a reflection coefficient ($\sigma$) of 1.0 indicate in the context of capillary permeability?
What does a reflection coefficient ($\sigma$) of 1.0 indicate in the context of capillary permeability?
Which of the following Starling forces promotes filtration?
Which of the following Starling forces promotes filtration?
In the context of microcirculation, what does hydraulic conductance ($K_f$) represent?
In the context of microcirculation, what does hydraulic conductance ($K_f$) represent?
Which of the following scenarios would result in decreased fluid reabsorption into the capillary?
Which of the following scenarios would result in decreased fluid reabsorption into the capillary?
Which of the following is considered a primary function of arterioles?
Which of the following is considered a primary function of arterioles?
If a red blood cell is placed in a hypertonic solution, what will happen to the cell?
If a red blood cell is placed in a hypertonic solution, what will happen to the cell?
Which of the following factors increases hydraulic conductance ($K_f$)?
Which of the following factors increases hydraulic conductance ($K_f$)?
What is the functional significance of venules having thin walls with little smooth muscle?
What is the functional significance of venules having thin walls with little smooth muscle?
Which best explains how arteriovenous anastomoses help control skin temperature?
Which best explains how arteriovenous anastomoses help control skin temperature?
A patient with liver failure has a decreased ability to synthesize plasma proteins. How does this affect the Starling forces and fluid movement in the capillaries?
A patient with liver failure has a decreased ability to synthesize plasma proteins. How does this affect the Starling forces and fluid movement in the capillaries?
What changes in Starling forces would contribute to edema formation in a patient with nephrotic syndrome (characterized by significant protein loss in urine)?
What changes in Starling forces would contribute to edema formation in a patient with nephrotic syndrome (characterized by significant protein loss in urine)?
A researcher is studying a new drug that selectively dilates arterioles. What effect would this drug have on capillary hydrostatic pressure and fluid filtration in the treated tissue?
A researcher is studying a new drug that selectively dilates arterioles. What effect would this drug have on capillary hydrostatic pressure and fluid filtration in the treated tissue?
Which statement BEST describes the relationship between the lymphatic system and edema?
Which statement BEST describes the relationship between the lymphatic system and edema?
A patient is experiencing severe inflammation due to a burn injury which is impacting microcirculation. What effect will this have on hydraulic conductance and net fluid movement, assuming other Starling forces remain constant?
A patient is experiencing severe inflammation due to a burn injury which is impacting microcirculation. What effect will this have on hydraulic conductance and net fluid movement, assuming other Starling forces remain constant?
In a scenario where the thoracic duct is blocked, what immediate effect would this have on microcirculation and fluid balance?
In a scenario where the thoracic duct is blocked, what immediate effect would this have on microcirculation and fluid balance?
Consider a scenario where both capillary hydrostatic pressure ($P_c$) and interstitial oncotic pressure ($\pi_i$) are significantly elevated due to specific pathological changes. How would this condition influence the overall movement of fluid across the capillary membrane, and what clinical manifestation might be expected?
Consider a scenario where both capillary hydrostatic pressure ($P_c$) and interstitial oncotic pressure ($\pi_i$) are significantly elevated due to specific pathological changes. How would this condition influence the overall movement of fluid across the capillary membrane, and what clinical manifestation might be expected?
A novel drug is developed that selectively increases the number of aquaporins (water channels) in capillary endothelial cells. How would this drug impact fluid exchange in the microcirculation, assuming all other Starling forces remain constant, and what is a potential therapeutic application?
A novel drug is developed that selectively increases the number of aquaporins (water channels) in capillary endothelial cells. How would this drug impact fluid exchange in the microcirculation, assuming all other Starling forces remain constant, and what is a potential therapeutic application?
Imagine a hypothetical scenario involving a newly discovered pathogen that selectively colonizes the endothelial glycocalyx of capillaries, significantly altering its charge and structure without directly damaging the endothelial cells themselves. Assuming no other physiological changes, how would this most likely impact microvascular permeability & what implications would it have for transcapillary exchange?
Imagine a hypothetical scenario involving a newly discovered pathogen that selectively colonizes the endothelial glycocalyx of capillaries, significantly altering its charge and structure without directly damaging the endothelial cells themselves. Assuming no other physiological changes, how would this most likely impact microvascular permeability & what implications would it have for transcapillary exchange?
Flashcards
Microcirculation
Microcirculation
The circulation of blood in the smallest blood vessels.
Arterioles
Arterioles
Smallest branches of arteries, high smooth muscle composition and highly innervated.
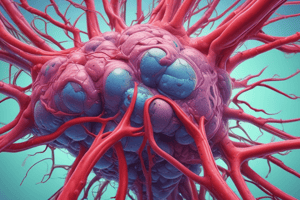
Capillaries
Capillaries
Single layer of endothelial cells (thin wall) surrounded by basal lamina; exchange of nutrients, gases, water and solutes between blood and tissues
Venules
Venules
Signup and view all the flashcards
Capillary Bed
Capillary Bed
Signup and view all the flashcards
Arteriovenous Anastomoses
Arteriovenous Anastomoses
Signup and view all the flashcards
Simple Diffusion
Simple Diffusion
Signup and view all the flashcards
Osmosis
Osmosis
Signup and view all the flashcards
Tonicity
Tonicity
Signup and view all the flashcards
Isotonic Solution
Isotonic Solution
Signup and view all the flashcards
Hypotonic Solution
Hypotonic Solution
Signup and view all the flashcards
Hypertonic Solution
Hypertonic Solution
Signup and view all the flashcards
Reflection Coefficient (σ)
Reflection Coefficient (σ)
Signup and view all the flashcards
Effective Osmotic Pressure
Effective Osmotic Pressure
Signup and view all the flashcards
Starling Equation
Starling Equation
Signup and view all the flashcards
Causes of Edema
Causes of Edema
Signup and view all the flashcards
Decreased capillary oncotic pressure
Decreased capillary oncotic pressure
Signup and view all the flashcards
Increased capillary permeability
Increased capillary permeability
Signup and view all the flashcards
Impaired lymphatic drainage
Impaired lymphatic drainage
Signup and view all the flashcards
Hydrostatic Pressure
Hydrostatic Pressure
Signup and view all the flashcards
Oncotic Pressure
Oncotic Pressure
Signup and view all the flashcards
Increased Pc
Increased Pc
Signup and view all the flashcards
Decreased π.c
Decreased π.c
Signup and view all the flashcards
Lymphatic System
Lymphatic System
Signup and view all the flashcards
Edema
Edema
Signup and view all the flashcards
Study Notes
- Microcirculation involves capillaries, the lymphatic system, and fluid exchange
- It refers to the function of arterioles, capillaries, venules, and neighboring lymphatic vessels
Microcirculation Function
- Blood circulates through the smallest blood vessels
- Nutrients, gases, and waste products are exchanged in tissues
- Fluid is exchanged between vascular and interstitial compartments
- Capillaries deliver blood and act as sites for nutrient and waste exchange
- They also facilitate fluid exchange between vascular and interstitial compartments
Macro vs Microcirculation
- Macrocirculation includes arteries that are greater than 400 micrometers
- Arteries are conduit vessels with 5% of total resistance
- Microcirculation includes pre-arterioles (100-400 micrometers), arterioles (40-100 micrometers), and capillaries (less than 10 micrometers)
- Pre-arterioles and arterioles regulate flow through metabolic control and flow regulation
- They contribute 20% and 60% of total resistance, respectively
- Capillaries are exchange vessels made of endothelial cells only, and contribute 15% of total resistance
Vessels
- Arterioles, which are the smallest branches of arteries, have a high smooth muscle composition
- They are highly innervated
- Arterioles respond to sympathetic stimulation or vasoactive substances and have the highest resistance to blood flow
- Capillaries have a single layer of endothelial cells surrounded by a basal lamina
- They allow for the exchange of nutrients, gases, water, and solutes between blood and tissues
- Capillaries can be selectively perfused with blood
- Venules are thin-walled, lack smooth muscle, and have elastic tissue, which increases capacitance and causes low pressure
Capillary Beds
- In capillary beds, terminal arterioles flow into metarterioles, then precapillary sphincters, forming true capillaries, postcapillary venules, and ultimately venules
- Blood is delivered to capillary beds via arterioles
- Constriction or relaxation of arterioles affects blood flow to the capillaries
- Precapillary sphincters are bands of smooth muscle that control blood flow into the capillaries, functioning as switches
- True capillaries merge into venules, carrying blood from tissues to veins and back to the macrocirculation
Capillary Bed Pathway
- In the capillary bed blood flows from the:
- Arteriole
- Meta-arteriole
- Capillary bed
- Venule
- Vein
- Arteriovenous anastomoses have no nutrient or fluid exchange
- They help control skin temperature through volume changes in the superficial venous bed
Substance Exchange across the Capillary Wall
- Exchange of solutes and gases across capillary walls occurs by simple diffusion
- Some solutes diffuse through endothelial cells, while others diffuse between them, depending on whether they are lipophilic
- Capillaries contain a single endothelial layer and water-filled clefts between cells
- O₂ and CO₂ (non-polar), diffuse through endothelial cells because they are highly lipid-soluble, as are N₂ and NO
- Water-soluble molecules (hydrophilic) must diffuse through aqueous clefts between endothelial cells (pores)
- Examples include H₂O, charged ions, glucose, and amino acids
- Proteins are generally too large to cross capillary walls via clefts and are, therefore, retained in the vascular compartment
- Some tissues can have capillaries with 'tight' clefts (brain-blood-barrier)
- Other capillaries may have ‘fenestrations’ allowing few small proteins to pass
- Proteins may cross through pinocytotic vesicles (transcytosis)
Simple Diffusion
- During simple diffusion, solutes and gases exchange across the capillary wall if the membrane is permeable to them
- Molecules move either through the membrane or between the endothelial cells (clefts)
- It’s driven by a partial pressure/concentration gradient in which individual gases or solutes move downwards until equilibrium is achieved
- The rate of diffusion depends on driving force and surface area, and more capillaries increase surface area
Osmosis and Hydrostatic Pressure
- Osmosis and hydrostatic pressure drive fluid movement across the capillary wall
- Osmosis is the flow of water across a semipermeable membrane that is impermeable to the solute
- Solute concentration needs to be equalized on each side of the membrane
- Concentration differences of impermeate solutes create osmotic pressure differences, causing water to flow by osmosis
- Solute concentration contributes to the effective osmotic pressure
- Capillary hydrostatic pressure is the pressure of blood inside capillaries, pushing fluid out into surrounding tissues (interstitial area)
Tonicity
- Tonicity measures effective osmotic pressure gradient
- Isotonic solutions have the same “isos" meaning equal, similar
- In isotonic, effective osmotic pressure is the same
- Lower osmotic pressure is hypotonic; higher osmotic pressure is hypertonic
- Water flows from hypotonic to hypertonic solutions
- The reflection coefficient measures how well a membrane prevents the passage of certain solutes, and ranges from 0 to 1
- A reflection coefficient of 0 means the membrane allows all solutes to pass freely
- A reflection coefficient of 1 means the membrane completely blocks the passage of solutes
- If σ = 1.0, the membrane is impermeable to the solute, effective osmotic pressure is maximal, and it causes maximal water flow
- An example is serum albumin inside capillaries
Effective Osmotic Pressure
- In the capillaries, capillary walls have a reflection coefficient of 1.0 (impermeable to proteins)
- Proteins cannot cross the wall, and they apply their full osmotic pressure inside of the capillaries, pulling fluid from the interstitial space
- In capillary blood, proteins (mainly albumin) contribute to the effective osmotic pressure
- The effective osmotic pressure contributed by protein can also be called colloid osmotic pressure or oncotic pressure
Starling Equation
- Starling pressures, described by the Starling Equation, describe the passive exchange of fluid between capillary microcirculation and the interstitial space with fluid movement across a capillary wall
- Jv = Net fluid movement (mL/min)
- Kf = Vascular permeability coefficient (mL/min per mm Hg)
- Pc = Capillary hydrostatic pressure (mm Hg)
- Pi = Interstitial hydrostatic pressure (mm Hg)
- πc = Capillary oncotic pressure (mm Hg)
- πi = Interstitial oncotic pressure (mm Hg)
- Fluid movement (Jv) across the capillary wall is determined by the net pressure across the wall
- Jv = Kf [(Pc – Pi) – (πc – πi)]
- Hydrostatic pressure is (Pc – Pi) and Oncotic pressure is (πc – πi)
- Direction of fluid movement can be either out of the capillary or into the capillary
- Movement out of the capillary to the interstitial fluid is called filtration
- Jv is a positive number
- Movement from the interstitium into the capillary is called reabsorption
- Jv will be a negative number
- Magnitude of fluid movement is determined by hydraulic conductance (Kf)
- Kf, the vascular permeability coefficient of the capillary wall, is highly dependent on the type of capillary
- This regulates how much fluid movement will take place at a certain pressure difference
- Pc capillary hydrostatic pressure forces filtration and is mainly arterial pressure, decreasing from blood resistance, along the capillary length
- Pi interstitial hydrostatic pressure opposes filtration
- Pi is normally nearly zero or slightly negative
- πc capillary oncotic pressure opposes filtration, is the oncotic pressure of the capillary blood, from protein plasma, and increases protein conc and decreased filtration
- πi interstitial oncotic pressure favors filtration, is determined by intersitital fluid protein conc, and it normally low due to low protein conc instertitial fluid
Summary of Starling Pressures
- In Filtration the Arterial end has net filtration pressure = +10 mm Hg
- Fluid exits here because the capillary hydrostatic pressure is greater than the blood colloidal osmotic pressure
- At mid capillary there is no net movement, and thus net filtration pressure = 0 mm Hg as capillary hydrostatic pressure = blood colloidal osmotic pressure
- In reabsoprtion, at the venous end net filtration pressure = -7 mm HG
- Fluid re-enters because capillary hydrostatic pressure is less thatn blood colloidal osmotic pressure
Changes in Starling Pressure
- Can influence the direction and magnitude of fluid movement across capillaries
- Several changes can produce increased filtration (fluid movement out of capillaries)
- Increasing the Starling forces that favor filtration or decreasing the Starling forces that favor absorption will increase fluid movement
- Increase in Pc i.e., caused by increased arterial pressure
- Decrease in πc i.e., caused by reduction of plasma protein concentration
Lymphatic System
- It controls returning interstitial fluid and small proteins to the vascular compartment
- The lymphatic capillaries are located close to the capillary bed
- They have one-way flap valves, allowing interstitial fluid and small proteins to enter, but not to leave the lymphatic vessels
- These lymphatic capillaries merge into larger lymphatic vessels and into the thoracic duct, taking lymph into the large veins
- Lymphatic vessels have smooth muscle walls that contract
- Lymph return flow is aided by smooth muscle contraction and compression by skeletal muscle around it
Edema
- Occurs from an increase in interstitial fluid volume, which is defined as edema or swelling
- Occurs when the amount of fluid that leaks out of capillaries exceeds the lymphatic system's capacity to drain and return it to the larger circulation
- Edema can form when there is increased filtration, decreased reabsorption, or reduced/impaired lymphatic drainage
- Starling Equation: Jv = Kf [(Pc – Pi) – (πc – πi)]
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.