Podcast
Questions and Answers
What symptom is not associated with severe disease in this context?
What symptom is not associated with severe disease in this context?
- Abdominal pain
- Severe anemia
- More than six bloody bowel movements per day
- Loss of appetite (correct)
What is the primary reason to administer TPN in patients with severe disease?
What is the primary reason to administer TPN in patients with severe disease?
- To increase bowel movements
- If feedings cannot be reinstituted within 7-10 days (correct)
- To provide immediate pain relief
- To treat hypoalbuminemia directly
What complication develops in over 40% of patients with severe disease?
What complication develops in over 40% of patients with severe disease?
- Toxic megacolon
- Intestinal perforation
- Pouchitis (correct)
- Fulminant colitis
Which of the following interventions is recommended for managing severe disease?
Which of the following interventions is recommended for managing severe disease?
What should be done for patients receiving long-term immunosuppressive therapy who are unresponsive to corticosteroid treatment?
What should be done for patients receiving long-term immunosuppressive therapy who are unresponsive to corticosteroid treatment?
What dietary recommendation is appropriate for patients with symptoms of diarrhea?
What dietary recommendation is appropriate for patients with symptoms of diarrhea?
Which dietary adjustment is suggested for patients who have undergone resection of more than 100 cm of the terminal ileum?
Which dietary adjustment is suggested for patients who have undergone resection of more than 100 cm of the terminal ileum?
What is the most prominent symptom of ulcerative colitis that practitioners should inquire about?
What is the most prominent symptom of ulcerative colitis that practitioners should inquire about?
How is the disease severity classified in patients with ulcerative colitis?
How is the disease severity classified in patients with ulcerative colitis?
What laboratory finding is indicative of disease severity in ulcerative colitis?
What laboratory finding is indicative of disease severity in ulcerative colitis?
What diagnostic procedure is considered key for identifying ulcerative colitis?
What diagnostic procedure is considered key for identifying ulcerative colitis?
What is a typical characteristic of patients with mild disease in ulcerative colitis?
What is a typical characteristic of patients with mild disease in ulcerative colitis?
What percentage of Crohn's disease cases involve both the small bowel and colon?
What percentage of Crohn's disease cases involve both the small bowel and colon?
For children and adolescents with poor intake due to growth retardation, what therapy may be beneficial?
For children and adolescents with poor intake due to growth retardation, what therapy may be beneficial?
Which symptom is least likely to be associated with Crohn's disease?
Which symptom is least likely to be associated with Crohn's disease?
Which complication is NOT commonly associated with Crohn's disease?
Which complication is NOT commonly associated with Crohn's disease?
What laboratory finding is indicative of anemia in Crohn's disease patients?
What laboratory finding is indicative of anemia in Crohn's disease patients?
Which factor is strongly associated with the development and progression of Crohn's disease?
Which factor is strongly associated with the development and progression of Crohn's disease?
Which diagnostic study is primarily used for visualizing the small intestine in Crohn's disease?
Which diagnostic study is primarily used for visualizing the small intestine in Crohn's disease?
Which of these extraintestinal manifestations is associated with Crohn's disease?
Which of these extraintestinal manifestations is associated with Crohn's disease?
What type of pain is commonly reported by patients with ileitis or ileocolitis in Crohn's disease?
What type of pain is commonly reported by patients with ileitis or ileocolitis in Crohn's disease?
Flashcards are hidden until you start studying
Study Notes
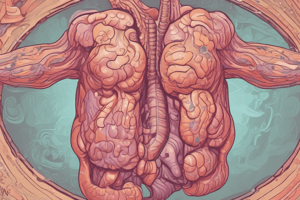
Crohn's Disease
- Crohn's disease affects different parts of the digestive tract, with the small bowel (ileitis) being the most commonly affected area (30%), followed by the small bowel and colon (ileococolitis) (50%).
- The colon is affected alone only in 20% of cases.
- Crohn's disease is a serious condition that can lead to a variety of complications, including obstruction, fistula formation, and abscesses.
- Cigarette smoking increases the risk of developing Crohn's disease, makes treatment less effective, and causes earlier relapses.
Symptoms and Signs
- General symptoms include fatigue, weight loss, and lack of energy.
- Diarrhea is common, especially in patients with ileitis or ileococolitis, and it's usually non-bloody and intermittent.
- In patients with colitis, bloody diarrhea and fecal urgency can occur, making it difficult to distinguish from ulcerative colitis.
- Abdominal pain is often present in the right lower quadrant or around the belly button.
Physical Examination
- Examination may reveal tenderness in the right lower quadrant.
- A palpable, tender mass in the lower abdomen could be a cluster of inflamed intestinal segments.
- Intestinal obstruction can occur due to inflammation, spasms, or scarring, causing a narrowing of the bowel.
- If the bowel wall breaks, it can lead to an abscess in the abdomen or behind the abdominal cavity.
- Signs of abscess include fever, chills, a tender abdominal mass, and increased white blood cell count.
Extraintestinal Manifestations
- Crohn's disease is associated with symptoms outside the digestive tract, such as joint pain, eye problems, and skin rashes.
- Mouth sores are a common occurrence.
- Other complications include gallstones and kidney stones.
Laboratory Values
- Blood tests may show signs of anemia (iron deficiency or vitamin B12 malabsorption) and increased white blood cell count.
- Protein levels in blood (albumin) may be low.
- High levels of ESR (sedimentation rate) or C-reactive protein indicate inflammation.
- Stool tests for lactoferrin, calprotectin, bacteria, parasites, white blood cells, fat, and C difficile toxin can help with diagnosis.
Special Diagnostic Studies
- Colonoscopy: Examining the colon with a camera.
- CT or MR Enterography: Imaging tests to look at the small intestine.
- Small bowel follow-through: Imaging test using a contrast material to examine the small intestine.
- Capsule endoscopy: Swallowing a small camera to examine the small intestine.
Complications
- Abscesses: Pockets of infection.
- Obstruction: Blockage of the bowel.
- Fistulas: Abnormal connections between the digestive tract and other organs.
- Carcinoma: Cancer.
- Hemorrhage: Bleeding.
- Malabsorption: Difficulty absorbing nutrients.
Treatment of Active Disease
- Nutrition plays a vital role in managing Crohn's disease.
- Restricting certain foods, like fried foods, and adjusting meal frequency is crucial.
- Patients with obstruction may need a low-roughage diet.
- If the terminal ileum has been removed, a low-fat diet with vitamin B12 supplements is recommended.
- Enteral therapy (feeding through a tube in the nose) can be beneficial for children and adolescents.
- Total parenteral nutrition (TPN), providing nutrients through a vein, is used in severe cases while awaiting surgery.
Ulcerative Colitis
- Ulcerative colitis primarily affects the colon, causing inflammation and ulcers.
- Bloody diarrhea is a key symptom, often accompanied by abdominal cramps and urgency.
- Sigmoidoscopy, a test to examine the rectum and lower colon, is vital for diagnosis.
Clinical Findings
- Bloody diarrhea is the most prominent symptom, along with lower abdominal cramps and tenesmus (a feeling of needing to have a bowel movement).
- Physical examination focuses on the patient's hydration status, nutritional status, and tenderness in the abdomen.
- Blood tests reveal the severity of anemia, inflammation (sedimentation rate), and protein levels.
- Endoscopy allows for a detailed view of the colon, aiding in determining the extent and severity of inflammation.
- Mild ulcerative colitis: Gradual onset, infrequent diarrhea, intermittent bleeding with mucus, mild abdominal pain relieved by bowel movements.
- Moderate ulcerative colitis: More severe diarrhea, frequent bleeding, possible abdominal pain and tenderness.
- Severe ulcerative colitis: Frequent bloody bowel movements, significant anemia, dehydration, impaired nutrition, and significant pain.
- Fulminant colitis: A rapidly worsening form of severe colitis with signs of toxicity.
General Measures for Severe Ulcerative Colitis
- Stopping all oral intake for up to 48 hours, until improvement is observed, is crucial.
- Total parenteral nutrition (TPN) may be needed for patients with severe malnutrition or inability to eat.
- Opioids and anticholinergic medications should be discontinued.
- Rehydration, electrolyte correction, and blood transfusions for anemia are essential.
- Close monitoring for worsening abdominal pain and distention is critical.
- X-rays of the abdomen are obtained to assess possible colonic dilation.
- Stool tests for bacteria, C difficile toxin, and parasites are performed.
- If long-term immunosuppressants are used, CMV infection needs to be considered.
- Blood clot prevention strategies are employed.
- Surgical consultation is required for patients with severe disease.
Treatment Options
- Corticosteroids are used to reduce inflammation.
- Anti-TNF therapies such as infliximab are effective in managing inflammation.
- Cyclosporine, an immunosuppressant, may be used If other treatments fail.
- Surgery is considered for severe disease unresponsive to medication.
Complications
- Pouchitis, inflammation in the ileal pouch (a surgically constructed reservoir for waste), develops in over 40% of patients after a colectomy, resembling symptoms of ulcerative colitis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.