Podcast
Questions and Answers
In the context of tissue repair, which cellular classification possesses the inherent capacity for sustained proliferation throughout the organism's lifespan, thereby facilitating continuous regeneration in response to physiological turnover and injury?
In the context of tissue repair, which cellular classification possesses the inherent capacity for sustained proliferation throughout the organism's lifespan, thereby facilitating continuous regeneration in response to physiological turnover and injury?
- Mesenchymal stem cells, due to their multipotent nature and capacity for differentiation into various connective tissue lineages.
- Permanent cells, exemplified by terminally differentiated neurons and cardiomyocytes, which have irreversibly exited the cell cycle.
- Labile cells, including the epithelial lining of the gastrointestinal tract and hematopoietic cells of the bone marrow. (correct)
- Stable cells, characterized by their quiescent state under homeostatic conditions but ability to enter the cell cycle upon specific stimulation.
Following a myocardial infarction, the infarcted tissue undergoes a repair process characterized by the formation of a non-contractile scar. Which of the following cellular and molecular events is the MOST critical determinant in the transition from granulation tissue to a mature, collagen-rich scar, influencing the long-term structural integrity and function of the remodeled myocardium?
Following a myocardial infarction, the infarcted tissue undergoes a repair process characterized by the formation of a non-contractile scar. Which of the following cellular and molecular events is the MOST critical determinant in the transition from granulation tissue to a mature, collagen-rich scar, influencing the long-term structural integrity and function of the remodeled myocardium?
- The deposition of fibronectin and provisional matrix components that act as a scaffold for migrating fibroblasts.
- The extent of angiogenesis and neovascularization within the granulation tissue, providing essential nutrients and oxygen for fibroblast survival.
- The initial influx of neutrophils and macrophages into the infarcted area, orchestrating the inflammatory cascade.
- The temporal expression and activity of matrix metalloproteinases (MMPs) and their tissue inhibitors (TIMPs) in regulating collagen turnover. (correct)
A patient presents with a chronic non-healing ulcer on their lower extremity. Histological examination reveals the presence of granulation tissue. Which of the following microscopic features would MOST strongly suggest impaired or dysregulated wound healing, potentially contributing to the chronicity of the ulcer?
A patient presents with a chronic non-healing ulcer on their lower extremity. Histological examination reveals the presence of granulation tissue. Which of the following microscopic features would MOST strongly suggest impaired or dysregulated wound healing, potentially contributing to the chronicity of the ulcer?
- Presence of myofibroblasts exhibiting α-smooth muscle actin (α-SMA) expression, indicative of contractile activity.
- A dense infiltrate of chronic inflammatory cells, dominated by lymphocytes and plasma cells, with scattered mast cells.
- Abundant newly formed capillaries with plump endothelial cells and minimal pericyte coverage.
- Disorganized collagen fiber deposition with excessive extracellular matrix accumulation and paucity of remodeling. (correct)
A surgeon is performing a skin closure following a meticulously executed excision of a benign lesion. To optimize healing by primary intention and minimize the risk of complications, which of the following intraoperative strategies would be MOST effective in promoting rapid and orderly tissue repair?
A surgeon is performing a skin closure following a meticulously executed excision of a benign lesion. To optimize healing by primary intention and minimize the risk of complications, which of the following intraoperative strategies would be MOST effective in promoting rapid and orderly tissue repair?
Upon histological examination of a skin biopsy from a patient with hypertrophic scarring, which of the following findings would be MOST indicative of the aberrant collagen remodeling processes driving the development of this pathological scar?
Upon histological examination of a skin biopsy from a patient with hypertrophic scarring, which of the following findings would be MOST indicative of the aberrant collagen remodeling processes driving the development of this pathological scar?
A researcher is investigating the effects of a novel therapeutic agent on wound healing in a murine model. To assess the impact of the agent on angiogenesis within granulation tissue, which of the following immunohistochemical markers would provide the MOST specific and quantitative measure of newly formed blood vessels?
A researcher is investigating the effects of a novel therapeutic agent on wound healing in a murine model. To assess the impact of the agent on angiogenesis within granulation tissue, which of the following immunohistochemical markers would provide the MOST specific and quantitative measure of newly formed blood vessels?
Which of the following complications of wound healing is characterized by the formation of a blind-ended, epithelium-lined tract that originates from a wound but does not connect to an internal organ or structure?
Which of the following complications of wound healing is characterized by the formation of a blind-ended, epithelium-lined tract that originates from a wound but does not connect to an internal organ or structure?
In the context of cutaneous wound healing, which of the following growth factors plays a central role in stimulating angiogenesis, fibroblast proliferation, and extracellular matrix deposition, thereby promoting the formation of granulation tissue and subsequent scar remodeling?
In the context of cutaneous wound healing, which of the following growth factors plays a central role in stimulating angiogenesis, fibroblast proliferation, and extracellular matrix deposition, thereby promoting the formation of granulation tissue and subsequent scar remodeling?
A patient presents with an incisional hernia following abdominal surgery. Which of the following factors would MOST significantly contribute to the development of this complication?
A patient presents with an incisional hernia following abdominal surgery. Which of the following factors would MOST significantly contribute to the development of this complication?
In dermal wound healing, which collagen type is initially predominant during early granulation tissue formation, providing a provisional matrix for fibroblast migration and subsequent collagen remodeling?
In dermal wound healing, which collagen type is initially predominant during early granulation tissue formation, providing a provisional matrix for fibroblast migration and subsequent collagen remodeling?
Flashcards
Repair (Definition)
Repair (Definition)
Replacement of damaged tissue by living tissue.
Regeneration
Regeneration
Replacement of destroyed tissue by the same cells.
Labile Cells
Labile Cells
Cells with a good power of continuous proliferation to replace aging cells.
Stable Cells
Stable Cells
Signup and view all the flashcards
Permanent Cells
Permanent Cells
Signup and view all the flashcards
Repair by Fibrosis
Repair by Fibrosis
Signup and view all the flashcards
Granulation Tissue
Granulation Tissue
Signup and view all the flashcards
Healing by Primary Intention
Healing by Primary Intention
Signup and view all the flashcards
Healing by Secondary Intention
Healing by Secondary Intention
Signup and view all the flashcards
Sinus (Wound Healing)
Sinus (Wound Healing)
Signup and view all the flashcards
Study Notes
- Repair describes the replacement of damaged tissue by living tissue.
Types of Repair
- Regeneration involves the replacement of destroyed tissue by the same cells, such as in bone fracture repair.
- Repair by fibrosis involves the replacement of destroyed tissue by granulation tissue, which matures into fibrosis.
Cell Proliferation Capacity
- Cells are classified by their proliferative capacity.
- Labile cells have a good power of continuous proliferation to replace aging cells, exemplified by stratified squamous epithelium of skin and columnar epithelium of the GIT.
- Stable cells do not proliferate under normal conditions but do so when needed, including parenchymatous cells like liver, pancreas, and renal tubules, and mesenchymal cells like fibroblasts, chondroblasts, and osteoblasts.
- Permanent cells cannot proliferate at all, such as muscle cells and nerve cells.
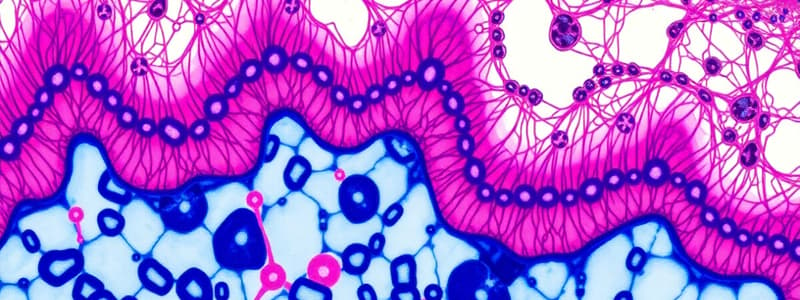
Granulation Tissue
- Granulation tissue is red, granular, soft, painless, and bleeds easily, forming in the gap of healing wounds.
- It consists of fibroblasts surrounded by collagen, newly formed blood vessels, scattered macrophages, and some other inflammatory cells.
- Scar formation occurs after excess collagen deposition and obliteration of the capillaries.
Characteristics of Granulation Tissue
- Light red or dark pink due to perfusion with new capillary loops.
- Soft to the touch.
- Moist and granular in appearance due to punctate hemorrhages.
- Pulsatile on palpation.
- Painless when healthy.
Wound Healing by Primary Intention
- Occurs in clean surgical wounds with minimal tissue destruction, minimal bleeding, no bacterial infection, and good apposition of wound edges.
- Initial hemorrhage results in the wound cavity filling with a blood clot.
- Inflammation occurs within 24 hours, with PNLs infiltrating the blood clot.
- Epithelial changes occur within 48 hours, as epithelial cells from wound edges proliferate.
- Early granulation tissue forms on the 3rd day as macrophages replace PNLs.
- Macrophages stimulate the ingrowth of fibroblasts and angioblasts, which start forming collagen type III, and epidermal cells form a bridge to seal off the defect.
- Fully developed granulation tissue occurs around days 4–6, characterized by neovascularization, and granulation tissue fills the wound gap.
- Scar formation occurs in the 2nd week, with inflammation subsiding as fibroblastic proliferation and collagen deposition continue.
- Remodeling of the scar occurs by the end of the 1st month.
Healing by Secondary Intention
- Occurs in gaping wounds with marked tissue destruction, bleeding, infection, and poor apposition of wound edges.
- The steps are the same as healing by primary intention, but the inflammatory response is greater.
- Abundant granulation tissue forms.
- Epithelization takes more time according to the wound gap.
- Excessive fibrosis and wound contraction occur.
- There is more liability to infection and complications.
Factors Affecting Wound Healing
- Local factors include the size and site of the wound, infection, foreign bodies, and blood supply to the area; poor blood supply delays repair.
- Systemic factors include age, nutritional disorders like anemia and malnutrition (which delay repair), metabolic disorders, chronic debilitating diseases and diabetes (which increase susceptibility to infection), and drugs like steroids and cytotoxic drugs (which delay repair).
Complications of Wound Healing
- Infection.
- Sinus: a blind duct lined by epithelium between the wound and external surface.
- Fistula: a duct lined by epithelium between the wound and a hollow organ.
- Ulcer: loss of continuity of surface epithelium.
- Keloid: excessive granulation tissue and scar formation.
- Incisional hernia.
- Cicatrization: a scar on flexures that interferes with movement.
- Implantation (epidermal) cyst.
- Malignant transformation: squamous cell carcinoma.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.