Podcast
Questions and Answers
What is the initial step in the treatment of Thoracic Outlet Syndrome (TOS) before considering surgical management?
What is the initial step in the treatment of Thoracic Outlet Syndrome (TOS) before considering surgical management?
- Surgical intervention should be immediately applied.
- Physiotherapy treatment should be deemed unnecessary.
- Complete bed rest is recommended.
- Conservative treatment must be proven ineffective. (correct)
Which physiotherapy technique involves using a sheet strap for mobilization of the first rib?
Which physiotherapy technique involves using a sheet strap for mobilization of the first rib?
- Glenohumeral mobilization
- Massage therapy
- Cervical traction
- First rib self-mobilization (correct)
Which muscles should be stretched to help alleviate symptoms related to thoracic outlet syndrome?
Which muscles should be stretched to help alleviate symptoms related to thoracic outlet syndrome?
- Pectoralis and lower trapezius (correct)
- Biceps and triceps
- Quadriceps and hamstrings
- Gluteus maximus and abdominal muscles
What is the purpose of cervical traction in the treatment of acute TOS patients?
What is the purpose of cervical traction in the treatment of acute TOS patients?
Which muscle group is primarily targeted for strengthening in TOS rehabilitation?
Which muscle group is primarily targeted for strengthening in TOS rehabilitation?
What condition can arise from tight hip flexors and weak hip extensors leading to poor pelvic alignment?
What condition can arise from tight hip flexors and weak hip extensors leading to poor pelvic alignment?
Which muscle is primarily involved in generating a torque couple to resist hip flexors?
Which muscle is primarily involved in generating a torque couple to resist hip flexors?
What is primarily required to confirm a diagnosis of thoracic outlet syndrome (TOS)?
What is primarily required to confirm a diagnosis of thoracic outlet syndrome (TOS)?
Which condition may develop due to repetitive overhead activities like swimming?
Which condition may develop due to repetitive overhead activities like swimming?
What is a characteristic feature of thoracic outlet syndrome's clinical presentation?
What is a characteristic feature of thoracic outlet syndrome's clinical presentation?
What is often the primary challenge in diagnosing thoracic outlet syndrome?
What is often the primary challenge in diagnosing thoracic outlet syndrome?
Which types of trauma can contribute to symptoms related to thoracic outlet syndrome?
Which types of trauma can contribute to symptoms related to thoracic outlet syndrome?
What diagnostic tool is NOT commonly used in the evaluation of suspected thoracic outlet syndrome?
What diagnostic tool is NOT commonly used in the evaluation of suspected thoracic outlet syndrome?
What percentage of normal function do the best knee replacements typically offer?
What percentage of normal function do the best knee replacements typically offer?
Which of the following is a post-operative guideline for cemented knee replacement regarding range of motion after 3-4 weeks?
Which of the following is a post-operative guideline for cemented knee replacement regarding range of motion after 3-4 weeks?
When should resisted exercises begin for a patient undergoing a knee replacement?
When should resisted exercises begin for a patient undergoing a knee replacement?
What is the correct timeline for partial weight bearing after cemented knee replacement?
What is the correct timeline for partial weight bearing after cemented knee replacement?
What does WBAT stand for in the context of cemented-less knee replacement ambulation?
What does WBAT stand for in the context of cemented-less knee replacement ambulation?
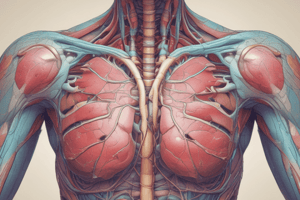
What is the primary anatomical region associated with thoracic outlet syndrome?
What is the primary anatomical region associated with thoracic outlet syndrome?
Which of the following is NOT a potential cause for a hot, painful knee joint shortly after surgery?
Which of the following is NOT a potential cause for a hot, painful knee joint shortly after surgery?
Which of the following is NOT a common method for preventing issues related to thoracic outlet syndrome?
Which of the following is NOT a common method for preventing issues related to thoracic outlet syndrome?
At what week do patients typically begin the transition to full weight bearing after a cemented-less knee replacement?
At what week do patients typically begin the transition to full weight bearing after a cemented-less knee replacement?
In regards to the neurovascular bundle associated with thoracic outlet syndrome, which structure does it NOT include?
In regards to the neurovascular bundle associated with thoracic outlet syndrome, which structure does it NOT include?
What percentage of body weight is a patient expected to bear by week 8 after a cemented-less knee replacement?
What percentage of body weight is a patient expected to bear by week 8 after a cemented-less knee replacement?
Which muscle is located anteriorly to the thoracic outlet?
Which muscle is located anteriorly to the thoracic outlet?
What is a benefit of switching from high-impact to low-impact exercises for individuals with Achilles tendon issues?
What is a benefit of switching from high-impact to low-impact exercises for individuals with Achilles tendon issues?
What can exacerbate symptoms of thoracic outlet syndrome?
What can exacerbate symptoms of thoracic outlet syndrome?
What is the purpose of the crossover effect in rehabilitation for Achilles tendinopathy?
What is the purpose of the crossover effect in rehabilitation for Achilles tendinopathy?
What is the correct classification of thoracic outlet syndrome based on its pathophysiology?
What is the correct classification of thoracic outlet syndrome based on its pathophysiology?
What is a potential sign or symptom of thoracic outlet syndrome?
What is a potential sign or symptom of thoracic outlet syndrome?
Which treatment is not typically recommended for the acute stage of Achilles tendon pain?
Which treatment is not typically recommended for the acute stage of Achilles tendon pain?
Which of the following does NOT contribute to the complexity of diagnosing thoracic outlet syndrome?
Which of the following does NOT contribute to the complexity of diagnosing thoracic outlet syndrome?
How does a heel lift affect the Achilles tendon during weight bearing?
How does a heel lift affect the Achilles tendon during weight bearing?
What should be avoided to minimize stress during rehabilitation of the Achilles tendon?
What should be avoided to minimize stress during rehabilitation of the Achilles tendon?
What type of exercise is recommended to initially strengthen the plantar flexor muscle during rehabilitation?
What type of exercise is recommended to initially strengthen the plantar flexor muscle during rehabilitation?
Which of the following statements is true regarding ant pronation taping?
Which of the following statements is true regarding ant pronation taping?
What is one potential consequence of prolonged use of a walking boot for Achilles tendon treatment?
What is one potential consequence of prolonged use of a walking boot for Achilles tendon treatment?
What typically characterizes nerve conduction studies in patients with thoracic outlet syndrome?
What typically characterizes nerve conduction studies in patients with thoracic outlet syndrome?
Which muscle groups should be assessed for adaptive shortening during the physical examination for thoracic outlet syndrome?
Which muscle groups should be assessed for adaptive shortening during the physical examination for thoracic outlet syndrome?
What imaging technique is primarily used to identify vascular thoracic outlet syndrome?
What imaging technique is primarily used to identify vascular thoracic outlet syndrome?
What should a clinician assess to determine the mobility of the first rib?
What should a clinician assess to determine the mobility of the first rib?
Which symptom is commonly exacerbated by arm abduction and external rotation in thoracic outlet syndrome?
Which symptom is commonly exacerbated by arm abduction and external rotation in thoracic outlet syndrome?
What finding indicates rib hypomobility during examination in thoracic outlet syndrome?
What finding indicates rib hypomobility during examination in thoracic outlet syndrome?
What is a common position change expected in the clavicle during a thoracic outlet syndrome assessment?
What is a common position change expected in the clavicle during a thoracic outlet syndrome assessment?
How is thoracic outlet syndrome usually differentiated from other conditions?
How is thoracic outlet syndrome usually differentiated from other conditions?
Flashcards
Low-Impact Activities for Achilles Tendon
Low-Impact Activities for Achilles Tendon
Switching from high-impact activities, such as running, to low-impact exercises like biking or swimming can reduce stress on your Achilles tendon.
Rest for Achilles Tendinopathy
Rest for Achilles Tendinopathy
For non-acute Achilles tendinopathy, complete rest is not recommended. Continue with recreational activities within your pain tolerance while participating in rehabilitation.
Cross-Training for Achilles Tendinopathy
Cross-Training for Achilles Tendinopathy
Exercising the uninjured ankle can help prevent muscle atrophy in the injured ankle by stimulating the injured muscles.
Ice Therapy for Achilles Tendinopathy
Ice Therapy for Achilles Tendinopathy
Signup and view all the flashcards
Electrotherapy for Achilles Tendinopathy
Electrotherapy for Achilles Tendinopathy
Signup and view all the flashcards
Extracorporeal Shockwave Therapy (ESWT)
Extracorporeal Shockwave Therapy (ESWT)
Signup and view all the flashcards
Taping for Achilles Tendinopathy
Taping for Achilles Tendinopathy
Signup and view all the flashcards
Orthotics for Achilles Tendinopathy
Orthotics for Achilles Tendinopathy
Signup and view all the flashcards
What is Thoracic Outlet Syndrome?
What is Thoracic Outlet Syndrome?
Signup and view all the flashcards
Describe the Thoracic Outlet.
Describe the Thoracic Outlet.
Signup and view all the flashcards
What is Thoracic Outlet Syndrome (TOS)?
What is Thoracic Outlet Syndrome (TOS)?
Signup and view all the flashcards
What is the neurovascular bundle?
What is the neurovascular bundle?
Signup and view all the flashcards
What is the costoclavicular space?
What is the costoclavicular space?
Signup and view all the flashcards
What is the subcoracoid space?
What is the subcoracoid space?
Signup and view all the flashcards
What is the scalene triangle?
What is the scalene triangle?
Signup and view all the flashcards
How does TOS happen?
How does TOS happen?
Signup and view all the flashcards
How does posture affect TOS?
How does posture affect TOS?
Signup and view all the flashcards
How can tight muscles cause TOS?
How can tight muscles cause TOS?
Signup and view all the flashcards
How does repetitive activity contribute to TOS?
How does repetitive activity contribute to TOS?
Signup and view all the flashcards
How does trauma affect TOS?
How does trauma affect TOS?
Signup and view all the flashcards
How is TOS diagnosed?
How is TOS diagnosed?
Signup and view all the flashcards
What are the types of TOS?
What are the types of TOS?
Signup and view all the flashcards
Why is differential diagnosis important for TOS?
Why is differential diagnosis important for TOS?
Signup and view all the flashcards
First Rib Mobilization
First Rib Mobilization
Signup and view all the flashcards
MWM for First Rib
MWM for First Rib
Signup and view all the flashcards
Strengthening for TOS
Strengthening for TOS
Signup and view all the flashcards
Cervical and Thoracic Mobilization
Cervical and Thoracic Mobilization
Signup and view all the flashcards
Glenohumeral Mobilizations for TOS
Glenohumeral Mobilizations for TOS
Signup and view all the flashcards
Nerve Conduction Studies in TOS
Nerve Conduction Studies in TOS
Signup and view all the flashcards
TOS & Dermatomal/Myotomal Pattern
TOS & Dermatomal/Myotomal Pattern
Signup and view all the flashcards
Diagnosing Vascular TOS
Diagnosing Vascular TOS
Signup and view all the flashcards
Imaging for TOS
Imaging for TOS
Signup and view all the flashcards
Breathing Assessment in TOS
Breathing Assessment in TOS
Signup and view all the flashcards
Muscle Assessment in TOS
Muscle Assessment in TOS
Signup and view all the flashcards
First Rib Assessment in TOS
First Rib Assessment in TOS
Signup and view all the flashcards
Cervical Rotation-Side Bending Test
Cervical Rotation-Side Bending Test
Signup and view all the flashcards
Total Knee Replacement Function
Total Knee Replacement Function
Signup and view all the flashcards
Total Hip Replacement Function
Total Hip Replacement Function
Signup and view all the flashcards
Cemented Knee Replacement: Early Range of Motion
Cemented Knee Replacement: Early Range of Motion
Signup and view all the flashcards
Cementless Knee Replacement: Early Range of Motion
Cementless Knee Replacement: Early Range of Motion
Signup and view all the flashcards
Immediate Postoperative Exercise
Immediate Postoperative Exercise
Signup and view all the flashcards
Starting Resistive Exercises
Starting Resistive Exercises
Signup and view all the flashcards
Cemented Knee Replacement: Ambulation
Cemented Knee Replacement: Ambulation
Signup and view all the flashcards
Cementless Knee Replacement: Ambulation
Cementless Knee Replacement: Ambulation
Signup and view all the flashcards
Study Notes
Achilles Tendinopathy/Tendinosis/Tendinopathy
- Achilles tendinopathy is a common overuse injury.
- It is a combination of pathological changes affecting the Achilles tendon.
- It's usually caused by overuse and chronic stress on the tendon.
- It can occur in both athletes and non-athletes.
- A lack of flexibility or a stiff Achilles tendon can increase the risk.
- The Achilles tendon is the thickest and strongest tendon in the body.
- Its origin is from the gastrocnemius and soleus muscles, and it inserts on the calcaneal tuberosity.
- It's approximately 15 cm (6 inches) long.
- The tendon experiences 3.9 times body weight during walking and 7.7 times during running.
- It's surrounded by a connective tissue sheath (paratenon) instead of a synovial sheath.
- The paratenon provides the major blood supply to the tendon.
- The blood supply is distal from intraosseous vessels of the calcaneus and proximally from intramuscular branches.
- An area of avascularity exists 2-6 cm from the calcaneal insertion, making the tendon vulnerable to degeneration and injury.
- Vascular density is greatest proximally and least in the midportion.
- Repetitive impact loading from activities like running and jumping commonly leads to Achilles tendon injuries.
- The tendon or paratenon (or both) can become inflamed, leading to tendonitis or peritendinitis.
- Excessive compression during repetitive energy storage and release can lead to sudden injury or, rarely, rupture.
- "Tendinosis" is a more accurate term than "tendonitis" because inflammation isn't always present.
- The condition is classified as insertional or mid-substance/noninsertional based on location.
Classification of Achilles Tendinopathy
- Insertional: within 2cm of the insertion.
- Mid-substance/noninsertional: 2-6cm proximal to the insertion.
Causes of Achilles Tendonitis
- Overuse: Forces within the physiological range repeated with poor recovery time lead to tendon fatigue, making it susceptible to micro tears.
- Sudden loading of excessive force, particularly during eccentric motion.
- Poor flexibility in the gastrocnemius and soleus muscles, increasing strain on the tendon.
- Muscle weakness of the gastrocnemius and soleus muscles resulting in micro tears and inflammation to the tendon.
- Joint restrictions (e.g., pes cavus) decrease shock absorption and affect adaptability to uneven terrain.
- Excessive pronation creates an internal tibial rotation, drawing the tendon medially and causing a whipping action.
- Systemic diseases like diabetes, lupus, and gout related to weakness within the tendon structure.
- Corticosteroid injections can contribute to tendon rupture.
- Training errors, such as poor footwear choices (too small, worn-out, inadequate heel counter) or running on hard or uneven surfaces.
Physical Examination and Findings
- Morning pain is a hallmark symptom as the tendon must tolerate stretching immediately after waking.
- Pain is diffuse in the back of the ankle (calf to heel).
- Activity aggravates the pain, especially uphill running and stair climbing.
- Pain is somewhat relieved by wearing high-heeled shoes or boots.
- Patients often report an increase in activity levels or a change in footwear.
- Observable, palpable edema and thickening of the Achilles tendon.
- Painful lumps or nodules within the tendon can be present.
- Crepitus during plantar and dorsiflexion is possible.
- A positive arc sign: the examiner palpates the tendon, and the patient performs dorsiflexion and plantarflexion.
- If the palpable thickening doesn't move but stays still with crepitation, it may indicate a tendon sheath injury.
- In the area of no swelling, 3cm proximal to the calcaneal insertion, palpation during movement.
- Positive Royal London Hospital test (RLH), pain on the tender spot disappears in maximal dorsiflexion.
- Decreased ankle dorsiflexion and hamstring tightness are common.
- Calf atrophy suggests a chronic condition.
- Pain during passive dorsiflexion or active/resisted plantarflexion is common.
- Damaged tendon fibers may calcify.
Diagnosis of tendinopathy
- History of symptoms
- Symptom behavior
- Clinical tests
- X-rays: can reveal calcification or hardening of the lower part of the tendon, indicating insertional tendinopathy. More severe non-insertional tendinopathy can show calcification in the midportion of the tendon.
- Ultrasound: A useful imaging tool indicating tendon width, water content, and collagen integrity, as well as bursal swelling.
- MRI: Not necessary for diagnosis but helpful for planning surgery.
Differential Diagnosis
- Plantar fasciitis
- Calcaneal fracture stress
- Heel pad syndrome
- Haglund deformity
- Sever's disease
- Posterior ankle impingement
- Medial tendinopathy
- Retrocalcaneal bursitis
- Sural nerve
- Lumbar radiculopathy
- Ankle osteoarthritis
- Deep vein thrombosis
- Partial Achilles tendon rupture
Management
-
Medical: Nonsteroidal anti-inflammatory drugs.
-
Botulinum injections: Temporarily reduce pain and spasm from neurovascular compression.
-
Surgery (for severe cases): Supraclavicular scalene surgery. Transaxillary resection of the first rib.
-
Physical therapy: Improves foot biomechanics, reduces pain/edema/inflammation, protects the inflamed tendon, enhance tendon healing, and optimizes muscle activity balance.
-
Rest, ice, compression, elevation (RICE) for initial symptom control.
-
Cross-training and exercise of non-involved muscles.
-
Orthotics (Air heel brace and/or night splints)
-
Heel-lifts.
-
Transverse friction massages
-
Stretching & strengthening exercises.
-
Isometric loading of the Achilles tendon.
-
Isotonic calf raises.
-
Plyometric exercises.
-
Mobilization techniques for the ankle and surrounding joints.
-
Proper foot wear
-
Maintenance of strength/flexibility for calf muscles
-
Monitoring activities and balancing mechanical abnormalities at the foot and ankle
-
Counterforce straps (to decrease symptoms and tension)
-
Proper conditioning and warm-ups during/after exercise
Thoracic Outlet Syndrome (TOS)
- Compression of neurovascular structures (nerves, blood vessels, or both).
- It can happen in the three spaces between the ribs: Interscalene triangle, Costoclavicular space or Sub-coracoid tunnel/sub-pectoralis minor space.
- May be categorized as vascular (vTOS, 3%) or neurological (nTOS, 97%), including true and disputed cases.
- Symptoms: Numbness/tingling in arm/fingers, pain/aches in neck, shoulder, arm, or hand, arm fatigue, weakening grip, possibly color changes (cyanosis or pallor)
- Etiology: Anatomical defects (extra rib, fibrous bands), poor posture, muscle imbalances, trauma (macro/micro), repetitive activity.
- Diagnosis: History, physical examination, provocative tests.
- Provocative tests: Roos test, scalene cramp test, scalene relief test
- Special vascular tests: Adson's Maneuver, Wright's test
- Electrodiagnostic tests/EMG studies help determine if nerve function is involved.
- Imaging tests (e.g., X-rays, venography, arteriography) may assess bony abnormalities or vascular narrowing.
- Management: Conservative (medical, physical therapy), Medical: NSAIDs, Botulinum injections, Surgery (for extreme cases), PT: First rib mobilization, neural/joint mobilization, postural correction, stretching and strengthening of related muscles, exercises, patient education/activity modification, disturbed sleep patterns.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.