Podcast
Questions and Answers
What type of cells are found in the distal convoluted tubule that respond to changes in solute concentration of the filtrate?
What type of cells are found in the distal convoluted tubule that respond to changes in solute concentration of the filtrate?
- Glomerular cells
- Vasa recta cells
- Macula densa cells (correct)
- Juxtaglomerular cells
What is the main function of the vasa recta?
What is the main function of the vasa recta?
- To regulate the glomerular filtration rate
- To filter out waste and water from the glomerular capillary
- To form a bundle of long straight vessels (correct)
- To secrete vasoconstriction substances
What is the first step in urine formation?
What is the first step in urine formation?
- Tubular reabsorption
- Tubular secretion
- Urinary excretion
- Glomerular filtration (correct)
What is the equation for urinary excretion?
What is the equation for urinary excretion?
Why are glomerular capillaries more permeable than capillaries in other tissues?
Why are glomerular capillaries more permeable than capillaries in other tissues?
What is the net force acting to move material out of the glomerulus and into the glomerular capsule?
What is the net force acting to move material out of the glomerulus and into the glomerular capsule?
What is the mechanism of neural regulation of GFR?
What is the mechanism of neural regulation of GFR?
What is the function of the juxtaglomerular apparatus (JGA) in regulating GFR?
What is the function of the juxtaglomerular apparatus (JGA) in regulating GFR?
What is the primary function of the urinary system in relation to waste removal?
What is the primary function of the urinary system in relation to waste removal?
Which of the following organs is responsible for blood filtering and urine formation?
Which of the following organs is responsible for blood filtering and urine formation?
What is the function of the renal cortex?
What is the function of the renal cortex?
What is the role of the renal calyx in the urinary system?
What is the role of the renal calyx in the urinary system?
What is the function of the ureter in the urinary system?
What is the function of the ureter in the urinary system?
What is the main role of the urinary bladder in the urinary system?
What is the main role of the urinary bladder in the urinary system?
Which of the following is NOT a function of the urinary system?
Which of the following is NOT a function of the urinary system?
What is the function of the renal medulla in the urinary system?
What is the function of the renal medulla in the urinary system?
What is the primary function of the glomerulus in the nephron?
What is the primary function of the glomerulus in the nephron?
Which of the following substances is reabsorbed by active transport in the proximal convoluted tubule?
Which of the following substances is reabsorbed by active transport in the proximal convoluted tubule?
What is the primary function of the juxtaglomerular apparatus?
What is the primary function of the juxtaglomerular apparatus?
Which of the following is NOT a function of the proximal convoluted tubule?
Which of the following is NOT a function of the proximal convoluted tubule?
What is the primary function of the ascending limb of the nephron loop?
What is the primary function of the ascending limb of the nephron loop?
What is the primary function of the distal convoluted tubule?
What is the primary function of the distal convoluted tubule?
What is the mechanism by which the proximal convoluted tubule reabsorbs proteins?
What is the mechanism by which the proximal convoluted tubule reabsorbs proteins?
What is the primary function of the collecting duct?
What is the primary function of the collecting duct?
What is the primary effect of ADH on the distal convoluted tubules and collecting ducts?
What is the primary effect of ADH on the distal convoluted tubules and collecting ducts?
What happens to urine volume when ADH is present?
What happens to urine volume when ADH is present?
What are the three major processes involved in urine formation and adjustment of blood composition?
What are the three major processes involved in urine formation and adjustment of blood composition?
What is the primary function of the preritubular capillary?
What is the primary function of the preritubular capillary?
What mode of transport is used to reabsorb glucose and amino acids in the proximal tubule?
What mode of transport is used to reabsorb glucose and amino acids in the proximal tubule?
What is the driving force behind water reabsorption in the proximal tubule?
What is the driving force behind water reabsorption in the proximal tubule?
What is the osmolarity of the fluid entering the loop of Henle?
What is the osmolarity of the fluid entering the loop of Henle?
What is the purpose of the countercurrent mechanism in the loop of Henle?
What is the purpose of the countercurrent mechanism in the loop of Henle?
What is the direction of Na+ movement in the ascending limb?
What is the direction of Na+ movement in the ascending limb?
What is the reason for the increase in osmolarity in the ISF as you go deeper in the medulla?
What is the reason for the increase in osmolarity in the ISF as you go deeper in the medulla?
What is the characteristic of the descending limb in the loop of Henle?
What is the characteristic of the descending limb in the loop of Henle?
What is the result of active pumping of salt out of the ascending limb?
What is the result of active pumping of salt out of the ascending limb?
What happens to the fluid in the ascending limb as you go up?
What happens to the fluid in the ascending limb as you go up?
What is the net overall result in the ISF as one progresses from the beginning to the end in the loop of Henle?
What is the net overall result in the ISF as one progresses from the beginning to the end in the loop of Henle?
What happens to H2O in the descending limb?
What happens to H2O in the descending limb?
What is the result of the mechanisms in the loop of Henle?
What is the result of the mechanisms in the loop of Henle?
Flashcards are hidden until you start studying
Study Notes
Functions of the Urinary System
- Excretion: removal of waste material from blood plasma and disposal of waste in urine
- Elimination: removal of waste from other organ systems
- Water balance: kidney tubules regulate water reabsorption and urine concentration
- Regulation of pH: volume, and composition of body fluids
- Production of erythropoietin for hematopoiesis and renin for blood pressure regulation
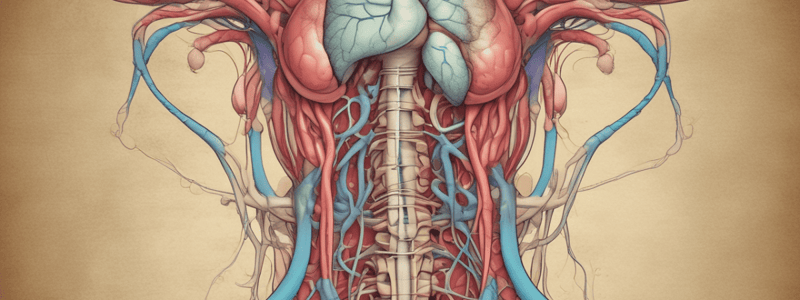
Anatomy of the Urinary System
- Kidneys: pair of bean-shaped organs located retroperitoneally, responsible for blood filtering and urine formation
- Renal capsule: layer of fibrous connective tissue covering the kidneys
- Renal cortex: outer region of the kidneys where most nephrons are located
- Renal medulla: inner region of the kidneys where some nephrons are located, and urine is collected to be excreted outward
- Renal calyx: duct-like sections of renal medulla for collecting urine from nephrons and directing urine into renal pelvis
- Renal pyramid: connective tissues in the renal medulla binding various structures together
- Renal pelvis: central urine collecting area of renal medulla
- Hilum: concave notch of kidneys where renal artery, renal vein, ureter, nerves, and lymphatic vessels converge
- Ureter: tubule that transports urine (mainly by peristalsis) from the kidney to the urinary bladder
- Urinary bladder: spherical storage organ that contains up to 400 ml of urine
Functions of Nephron Components
- Renal capsule: filteration of H2O and dissolved substances from the plasma
- Glomerulus: filtration of H2O and dissolved substances from the plasma
- Glomerular capsule: receives the glomerular filtrate
- Proximal convoluted tubule:
- Reabsorption of glucose, amino acids, creatine, lactic acid, citric acid, uric acid, and ascorbic acid by active transport
- Reabsorption of proteins by pinocytosis
- Reabsorption of H2O by osmosis
- Reabsorption of Cl- and other negatively charged ions by electrochemical attraction
- Active secretion of substances such as penicillin and hydrogen ions
- Descending limb of nephron loop: reabsorption of H2O by osmosis
- Ascending limb of nephron loop: reabsorption of Na, K, and Cl- by active transport
- Distal convoluted tubule:
- Reabsorption of Na by active transport
- Reabsorption of H2O by osmosis
- Active secretion of hydrogen ions
- Secretion of K both actively and by electrochemical attraction
- Collecting duct: reabsorption of H2O by osmosis
Juxtaglomerular Apparatus
- Located at the point of contact between the distal convoluted tubule and the afferent and efferent arterioles
- JG cells detect changes in blood pressure in the afferent arterioles and secrete renin
- Macula densa cells respond to changes in the solute concentration of the filtrate in the tubule
Glomerular Filtration
- Urine formation begins when waste and water and dissolved materials are filtered out of the glomerular capillary
- Urinary excretion = glomerular filtration + Tubular secretion - Tubular reabsorption
- Glomerular capillaries are much more permeable than capillaries in other tissues
- Filtration pressure = forces favoring filtration (Glomerular capillary hydrostatic pressure & capsular osmotic pressure) - forces opposing filtration (capsular hydrostatic pressure & Glomerular capillary osmotic pressure)
Regulation of GFR
- Neural regulation: sympathetic nerves can cause the constriction or relaxation of the afferent arteriole, resulting in a change of GFR
- Renal autoregulation: the juxtaglomerular apparatus secretes vasoconstriction substances to either afferent arteriole, in response to GFR changes and NaCl levels
- ADH causes the distal convoluted tubules and collecting ducts to become more permeable and increase H2O reabsorption by osmosis
Mechanism of forming dilute & concentrated urine
- Urine formation and adjustment of blood composition involves three major processes: Glomerular filtration, Tubular reabsorption, and Secretion
- Tubular reabsorption: the kidney must have mechanisms for reabsorption of the many solutes (Na+, K+, glucose, chloride -) and H2O that it filters each day
- Substances are selectively reabsorbed from the glomerular filtrate
- The peritubular capillary is adapted for reabsorption, carrying low-pressure blood and being very permeable
- Most reabsorption (70%) occurs in the proximal tubule
- Different modes of transport reabsorb various substances in particular segments of the renal tubule
Countercurrent Mechanism
- The fluid entering the loop of Henle has an osmolarity of 100 mosm/l
- The descending limb is very permeable to H2O, and Na+ and Cl- ions are reabsorbed
- The ascending limb is impermeable to H2O but actively transports Cl- out of the tubular fluid into interstitial fluid, with Na+ ion following passively
- Thus, a small horizontal gradient of 200 is established between the ascending and descending limbs
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.