Podcast
Questions and Answers
Where does the spinal cord originate from?
Where does the spinal cord originate from?
- Cerebellum
- Brain stem
- Medulla oblongata (correct)
- Cerebrum
What type of neurons have their cell bodies in the ventral horn of the spinal cord and use acetylcholine as their neurotransmitter?
What type of neurons have their cell bodies in the ventral horn of the spinal cord and use acetylcholine as their neurotransmitter?
- Lower Motor Neurons (correct)
- Sensory neurons
- Upper Motor Neurons
- Interneurons
What is the name of the nerve fibers that project from the end of the spinal cord beyond L1?
What is the name of the nerve fibers that project from the end of the spinal cord beyond L1?
- Cauda Equina (correct)
- Ventral Roots
- Conus Medullaris
- Dorsal Roots
What is the primary function of the dorsal horn of the gray matter in the spinal cord?
What is the primary function of the dorsal horn of the gray matter in the spinal cord?
What is the level of the vertebral column where the spinal cord terminates in adults?
What is the level of the vertebral column where the spinal cord terminates in adults?
What type of neurotransmitter is used by Upper Motor Neurons?
What type of neurotransmitter is used by Upper Motor Neurons?
Which type of reflex arc is responsible for maintaining posture?
Which type of reflex arc is responsible for maintaining posture?
In the Golgi Tendon Reflex, what is the primary function of the sensory receptors?
In the Golgi Tendon Reflex, what is the primary function of the sensory receptors?
Which of the following is NOT a part of the stretch reflex arc?
Which of the following is NOT a part of the stretch reflex arc?
What is the primary function of the ascending information pathway in the stretch reflex arc?
What is the primary function of the ascending information pathway in the stretch reflex arc?
What is the clinical correlation of the stretch reflex?
What is the clinical correlation of the stretch reflex?
Which of the following tracts is responsible for transmitting pain and temperature sensations?
Which of the following tracts is responsible for transmitting pain and temperature sensations?
What is the function of the Dermatomes in the spinal cord organization?
What is the function of the Dermatomes in the spinal cord organization?
Which of the following tracts contains upper motor neurons?
Which of the following tracts contains upper motor neurons?
Which of the following tracts carries information about pain and temperature?
Which of the following tracts carries information about pain and temperature?
What is the primary difference between a complete and incomplete spinal cord injury?
What is the primary difference between a complete and incomplete spinal cord injury?
Which of the following is a characteristic of a cord concussion?
Which of the following is a characteristic of a cord concussion?
What is the most common location of cord contusions?
What is the most common location of cord contusions?
What is the primary cause of cord infarction?
What is the primary cause of cord infarction?
What is the primary difference between primary and secondary cord injuries?
What is the primary difference between primary and secondary cord injuries?
Which of the following tracts is most lateral in the corticospinal tract?
Which of the following tracts is most lateral in the corticospinal tract?
What is the most common location of spinal cord injuries?
What is the most common location of spinal cord injuries?
What is the primary mechanism by which autoimmune diseases originate?
What is the primary mechanism by which autoimmune diseases originate?
What is the characteristic of autoantibodies in Systemic Lupus Erythematosus?
What is the characteristic of autoantibodies in Systemic Lupus Erythematosus?
What is the consequence of DNA deposition in the renal tubular basement membranes in Systemic Lupus Erythematosus?
What is the consequence of DNA deposition in the renal tubular basement membranes in Systemic Lupus Erythematosus?
What is the most common complication of hematologic abnormalities in Systemic Lupus Erythematosus?
What is the most common complication of hematologic abnormalities in Systemic Lupus Erythematosus?
What is the percentage of Systemic Lupus Erythematosus patients who develop cardiovascular diseases?
What is the percentage of Systemic Lupus Erythematosus patients who develop cardiovascular diseases?
What is the frequency of arthralgias or arthritis in Systemic Lupus Erythematosus patients?
What is the frequency of arthralgias or arthritis in Systemic Lupus Erythematosus patients?
What is the hallmark of the osteoarthritic process?
What is the hallmark of the osteoarthritic process?
Which joint disease is characterized by the presence of monosodium urate crystals in connective tissues throughout the body?
Which joint disease is characterized by the presence of monosodium urate crystals in connective tissues throughout the body?
What is the primary pathogenesis in Osteoarthritis?
What is the primary pathogenesis in Osteoarthritis?
What is the leading cause of disability in middle-aged and older populations in the US?
What is the leading cause of disability in middle-aged and older populations in the US?
Which of the following is a characteristic of Osteoarthritis?
Which of the following is a characteristic of Osteoarthritis?
What is the effect of the loss of proteoglycans from articular cartilage in Osteoarthritis?
What is the effect of the loss of proteoglycans from articular cartilage in Osteoarthritis?
What is the clinical manifestation of Gout in the great toe metatarsophalangeal joint?
What is the clinical manifestation of Gout in the great toe metatarsophalangeal joint?
What is the effect of increased water content in cartilage with normal aging?
What is the effect of increased water content in cartilage with normal aging?
What is the composition of the matrix in cartilage?
What is the composition of the matrix in cartilage?
What is the primary function of Chondrocytes in the articular cartilage?
What is the primary function of Chondrocytes in the articular cartilage?
Flashcards are hidden until you start studying
Study Notes
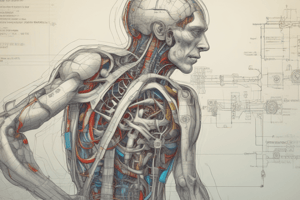
The Spinal Cord
- Lies within the vertebral column and is covered by the meninges
- Originates in the medulla oblongata and carries two types of information: efferent motor neuron outputs from the brain and afferent sensory neural inputs to the brain from the body
- In the adult, the spinal cord extends to the lower border of L1, with the conus medullaris located at L1/L2 and the cauda equina consisting of nerve fibers projecting from the end of the spinal cord to S5
Gray Matter Horns
- Dorsal horn: contains axons and interneurons of sensory (afferent) neurons, with sensory fibers traveling through the dorsal roots to the posterior horn of the gray matter
- Ventral horn: contains cell bodies for motor (efferent) pathways leaving the spinal cord, with motor fibers traveling out through the ventral roots from the anterior horn of the gray matter
Upper and Lower Motor Neurons
- Upper motor neurons: cell bodies located in the motor cortex of the brain, with axons reaching down to a certain vertebral level in the corticospinal tract, crossing from one side of the body to the other at the level of the brain stem, and using glutamate as their neurotransmitter
- Lower motor neurons: cell bodies located in the ventral horn of the spinal cord, with axons reaching out into the peripheral nervous system (PNS) and using acetylcholine as their neurotransmitter at the neuromuscular junction
Spinal Reflexes
- Definition: involuntary, near-instant response to a stimulus that does not involve input from the brain
- Types of reflex arcs:
- Autonomic - visceral organs
- Somatic
- Stretch - plays a major role in maintaining posture, including the deep tendon reflex (e.g., patellar tendon reflex) and the Golgi tendon reflex
- Crossed extensor - helps the body compensate for a stimulus on one side of the body
- Flexor/Withdrawal - withdrawal in response to a noxious stimulus
Stretch Reflex Arc
- Four processes:
- Monosynaptic response: information only goes through one synapse, involving the stretch of a muscle, sending an afferent message to the spinal cord, and receiving an efferent message to contract the muscle
- Reciprocal innervation: opposing muscle groups receive an efferent message to relax
- Synergistic muscle recruitment: accessory muscle groups receive an efferent message to help with the extension of the leg
- Ascending information: afferent fibers travel from the spinal cord up to the brain to process the event
Clinical Correlation - Stretch Reflex
- Operates as a protective mechanism to prevent strain or tear of muscles and tendons
- Clinically, reflexes can provide information about the spinal cord, peripheral nerves, and muscle tone/strength
Spinal Cord Organization
- Dermatomes and myotomes:
- Sensory: dermatomes
- Motor: myotomes
- We can predict deficits someone will have from an injury using dermatomes and myotomes
- Ascending and descending tracts:
- Ascending tracts: afferent/sensory
- Descending tracts: efferent/motor
Ascending and Descending Tracts
- Afferent pathways (ascending):
- Spinothalamic: vague touch, pain, temperature, with fibers decussating immediately at their level of entry into the spinal cord
- Dorsal columns: basic perception of touch, proprioception, vibration, with fibers crossing at the medulla
- Efferent pathways (descending):
- Corticospinal tracts: efferent/motor control below the head, containing upper motor neurons, with some fibers staying ipsilateral and traveling in the anterior corticospinal tract, and most fibers crossing at the medulla to travel down the lateral corticospinal tract
Spinal Cord Injuries
- Complete vs incomplete spinal cord injury:
- Complete spinal cord transection: interrupting all three tracts with complete loss of motor/sensory function below the level of injury
- Incomplete spinal cord injury: variable degree of dysfunction due to only part of the spinal cord being affected, with some tracts still intact and others disrupted
- Types of spinal cord injuries:
- Cord concussion: transient dysfunction of the spinal cord with or without vertebral damage and no pathologic changes, resolving within 48 hours
- Cord contusion: bruise caused by crushing of the spinal cord, leading to bleeding, edema, and tissue death, with severity depending on the integrity of remaining nerve fibers
- Cord compression: pressure on the spinal cord from an external source, such as bone, ruptured/herniated vertebral disks, hematoma, abscess, or tumor
- Cord transection: tear within the spinal cord itself due to traumatic injury, compromising blood supply and CSF, with clinically complete loss of motor/sensory function below the level of injury (if complete transection)
- Hemorrhage: typically due to trauma or vascular malformation, most commonly seen in the central gray matter at the point of impact, leading to further injury due to edema and cord infarction
- Infarct: blockage of vertebral arteries due to atherosclerosis, inflammation, or blood clots, leading to tissue death
- Evolution of spinal cord injury: primary cord injury (the actual trauma/compression/transaction) and secondary cord injury (a cascade of events leading to swelling and tissue destruction)
Autoimmune Reaction and Autoimmune Diseases
- Autoimmune reaction causes inflammation in areas of the body where it is not needed, leading to pain, swelling, and organ damage
- Autoimmune diseases originate from an initiating event in a genetically predisposed individual, leading to an autoimmune mechanism that affects specific target tissues or cells
Systemic Lupus Erythematosus (SLE)
- More common in women (10:1) and in people aged 20-40
- Characterized by frequent remissions and exacerbations
- A chronic, multisystem, inflammatory disease
- Pathophysiology involves production of a large variety of autoantibodies, including ANA, anti-DS DNA, anti-Smith, and APLA
- Autoantibodies are against nucleic acids, histones, ribonucleoproteins, and other nuclear materials
- Most common clinical manifestations:
- Arthralgias or arthritis (90%)
- Vasculitis and rash (malar and discoid)
- Renal disease (40% to 50%)
- Hematologic abnormalities (50% with anemia being the most common complication)
- Cardiovascular diseases (30% to 50%)
- Diagnosis is difficult due to intermittent and widespread symptoms
- serial or simultaneous presence of at least four of 11 common clinical findings indicates SLE
Arthropathies
- Joint diseases
- Types:
- Non-inflammatory arthropathy (Osteoarthritis)
- Inflammatory Arthropathies (Rheumatoid Arthritis, Gout, Ankylosing Spondylitis)
Osteoarthritis
- Most common joint disease
- Leading cause of disability in middle-aged and older populations in the US
- Most often affects knees, hip, neck, hands, and lower back
- Characterized by:
- Local areas of loss and damage of articular cartilage
- Bone spurs (osteophytes)
- Subchondral bone changes
- Variable degrees of mild synovitis
- Thickening of the joint capsule
- Susceptibility factors:
- Joint Vulnerability: systemic factors (Age, Female, Genetics, Nutritional factors)
- Joint Vulnerability: Intrinsic Factors (Previous damage, muscle weakness, malalignment, proprioception deficiency)
- Joint load factors (Obesity, Physical activities prone to injury)
- Pathogenesis:
- Primary pathogenesis is degeneration, loss, and disordered repair of articular cartilage
- Higher levels of pro-inflammatory markers and cascade of cytokine, biochemical, and growth factor pathways
- Chondrocytes of the articular cartilage become damaged
- Loss of proteoglycans from articular cartilage is a hallmark of the osteoarthritic process
- Cartilage composition:
- Water + Matrix
- Matrix: Collagen + Proteoglycans
- Clinical manifestations:
- Joint pain and stiffness
- Stiffness in morning and usually brief
Gout
- Clinical manifestations:
- Increase in serum urate concentration
- Recurrent attacks of monoarticular arthritis
- Severe pain, swelling, tenderness, erythema
- 50% of initial attacks are in great toe metatarsophalangeal joint
- Tophi: Deposits of monosodium urate in and around the joints
- Renal disease involving glomerular, tubular, and interstitial tissues and blood vessels
- Formation of renal stones
- 3 Clinical Stages:
- Asymptomatic Hyperuricemia
- Acute Gouty Arthritis
- Tophaceous Gout
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.