Podcast
Questions and Answers
What is the primary purpose of using an Esmarch bandage during lower limb surgery?
What is the primary purpose of using an Esmarch bandage during lower limb surgery?
- To prevent blood from flowing back into the limb (correct)
- To improve visibility of the surgical site
- To facilitate immediate wound closure
- To enhance blood circulation in the limb
What is a significant cause of delayed postoperative hemorrhage?
What is a significant cause of delayed postoperative hemorrhage?
- Inadequate preoperative assessment of the patient
- Excessive fluid administration during surgery
- Improper wound dressing techniques
- Ineffective management of blood pressure during the procedure (correct)
Why should care be taken when using pressure bandages for haemoabdomen?
Why should care be taken when using pressure bandages for haemoabdomen?
- They may cause excessive bleeding
- They promote rapid fluid absorption
- They reduce ventilation and perfusion to abdominal organs (correct)
- They can impair the patient's ability to move
Which factor can contribute to poor secondary haemostatic plug formation?
Which factor can contribute to poor secondary haemostatic plug formation?
What can result from slipped ligatures during a surgical procedure?
What can result from slipped ligatures during a surgical procedure?
Which knot is characterized by a double loop on the first throw to improve security?
Which knot is characterized by a double loop on the first throw to improve security?
What is a primary advantage of the one-hand tie technique?
What is a primary advantage of the one-hand tie technique?
In electrosurgery, which statement is true regarding the method of electrical current application?
In electrosurgery, which statement is true regarding the method of electrical current application?
Which ligature technique involves looping around the pedicle and not overlapping the loops?
Which ligature technique involves looping around the pedicle and not overlapping the loops?
What is the primary purpose of using two opposing mirror-image simple knots in a square knot?
What is the primary purpose of using two opposing mirror-image simple knots in a square knot?
Which technique is best suited for deep ligature placement?
Which technique is best suited for deep ligature placement?
When applying metal clips (Hemoclips), the diameter of the blood vessel should measure what proportion of the clip length?
When applying metal clips (Hemoclips), the diameter of the blood vessel should measure what proportion of the clip length?
Which technique uses a 'three clamp technique' before tying a ligature?
Which technique uses a 'three clamp technique' before tying a ligature?
Which knot requires pulling free ends in opposite directions to secure?
Which knot requires pulling free ends in opposite directions to secure?
To prevent the first throw from unwrapping before the second is placed, which knot should be used?
To prevent the first throw from unwrapping before the second is placed, which knot should be used?
What is the primary aim of using direct pressure (tamponade) during a surgical bleed?
What is the primary aim of using direct pressure (tamponade) during a surgical bleed?
Which method is considered the traditional and most secure for achieving haemostasis in larger vessels?
Which method is considered the traditional and most secure for achieving haemostasis in larger vessels?
What is a key caution when applying direct pressure to bleeding tissue?
What is a key caution when applying direct pressure to bleeding tissue?
When using haemostatic forceps, what is essential to achieve effective haemostasis?
When using haemostatic forceps, what is essential to achieve effective haemostasis?
Which of the following statements about ligation techniques is NOT true?
Which of the following statements about ligation techniques is NOT true?
What type of bleeds are vascular clips most suitable for?
What type of bleeds are vascular clips most suitable for?
What is the purpose of using a Pringle manoeuvre during surgery?
What is the purpose of using a Pringle manoeuvre during surgery?
Which statement about topical haemostatic agents is correct?
Which statement about topical haemostatic agents is correct?
Which of the following factors is crucial when dealing with coagulopathic patients during a surgical bleed?
Which of the following factors is crucial when dealing with coagulopathic patients during a surgical bleed?
What is a primary benefit of maintaining haemostasis during surgery?
What is a primary benefit of maintaining haemostasis during surgery?
Which method is used to estimate blood loss during surgery?
Which method is used to estimate blood loss during surgery?
What critical factor often influences the extent of haemorrhage during surgery?
What critical factor often influences the extent of haemorrhage during surgery?
Which condition may lead to increased surgical bleeding?
Which condition may lead to increased surgical bleeding?
What should be monitored to ensure effective haemostasis during surgery?
What should be monitored to ensure effective haemostasis during surgery?
Which technique is recommended to limit blood loss during dissection?
Which technique is recommended to limit blood loss during dissection?
Why is it important to address shock during surgery?
Why is it important to address shock during surgery?
What is one advantage of pre-emptive measures like ligation prior to transecting vessels?
What is one advantage of pre-emptive measures like ligation prior to transecting vessels?
Which parameter may indicate hypothermia during surgery?
Which parameter may indicate hypothermia during surgery?
What is a potential consequence of improper haemostasis during surgery?
What is a potential consequence of improper haemostasis during surgery?
What is a primary advantage of using bipolar diathermy as compared to unipolar diathermy?
What is a primary advantage of using bipolar diathermy as compared to unipolar diathermy?
Which of the following correctly describes radiosurgery?
Which of the following correctly describes radiosurgery?
What is a risk associated with poor contact during electrosurgery?
What is a risk associated with poor contact during electrosurgery?
What feature distinguishes the Ligasure device from other bipolar vessel sealers?
What feature distinguishes the Ligasure device from other bipolar vessel sealers?
What is a notable characteristic of the Harmonic Scalpel?
What is a notable characteristic of the Harmonic Scalpel?
Which function does adrenaline serve in small superficial wounds?
Which function does adrenaline serve in small superficial wounds?
What is a significant drawback of topical hemostatic agents?
What is a significant drawback of topical hemostatic agents?
What is the mechanism of action of tranexamic acid (TXA)?
What is the mechanism of action of tranexamic acid (TXA)?
What is the desired time limit for applying a tourniquet during surgical procedures?
What is the desired time limit for applying a tourniquet during surgical procedures?
Which of the following is true about active topical hemostatic agents?
Which of the following is true about active topical hemostatic agents?
What is the role of bone wax in surgery?
What is the role of bone wax in surgery?
Which of the following describes the application of lasers in surgical procedures?
Which of the following describes the application of lasers in surgical procedures?
What does desmopressin do in the context of von Willebrand's disease (vWD)?
What does desmopressin do in the context of von Willebrand's disease (vWD)?
Flashcards
Surgical Haemostasis
Surgical Haemostasis
A surgical procedure that prevents blood loss.
Surgical Site Infection (SSI)
Surgical Site Infection (SSI)
Infection that happens after surgery.
Haematoma
Haematoma
Collection of blood within tissues after surgery.
Seroma
Seroma
Signup and view all the flashcards
Shock
Shock
Signup and view all the flashcards
Preventative Haemostasis
Preventative Haemostasis
Signup and view all the flashcards
Postoperative Haemorrhage
Postoperative Haemorrhage
Signup and view all the flashcards
Quantifying Blood Loss
Quantifying Blood Loss
Signup and view all the flashcards
Finger and Blunt Dissection
Finger and Blunt Dissection
Signup and view all the flashcards
Meticulous Surgical Haemostasis
Meticulous Surgical Haemostasis
Signup and view all the flashcards
Direct Pressure (Tamponade)
Direct Pressure (Tamponade)
Signup and view all the flashcards
Haemostatic Forceps
Haemostatic Forceps
Signup and view all the flashcards
Ligation
Ligation
Signup and view all the flashcards
Vascular Clips
Vascular Clips
Signup and view all the flashcards
Electrosurgery
Electrosurgery
Signup and view all the flashcards
Radiosurgery
Radiosurgery
Signup and view all the flashcards
Vessel Sealing Devices
Vessel Sealing Devices
Signup and view all the flashcards
Adrenaline
Adrenaline
Signup and view all the flashcards
Topical Haemostatic Agents
Topical Haemostatic Agents
Signup and view all the flashcards
Tourniquet/Esmarch
Tourniquet/Esmarch
Signup and view all the flashcards
Square Knot
Square Knot
Signup and view all the flashcards
Surgeon's Knot
Surgeon's Knot
Signup and view all the flashcards
Miller's Knot
Miller's Knot
Signup and view all the flashcards
Modified Miller's Knot (Strangle)
Modified Miller's Knot (Strangle)
Signup and view all the flashcards
Vascular Clips (Hemoclips)
Vascular Clips (Hemoclips)
Signup and view all the flashcards
Electrosurgery (Electrocoagulation)
Electrosurgery (Electrocoagulation)
Signup and view all the flashcards
Monopolar Electrosurgery
Monopolar Electrosurgery
Signup and view all the flashcards
Bipolar Electrosurgery
Bipolar Electrosurgery
Signup and view all the flashcards
Stick Ties
Stick Ties
Signup and view all the flashcards
Figure of Eight Ligature
Figure of Eight Ligature
Signup and view all the flashcards
Esmarch Bandage
Esmarch Bandage
Signup and view all the flashcards
Postoperative Haemorrhage (Delayed Haemorrhage)
Postoperative Haemorrhage (Delayed Haemorrhage)
Signup and view all the flashcards
Abdominal Wraps/Pressure Bandage
Abdominal Wraps/Pressure Bandage
Signup and view all the flashcards
What is radiosurgery?
What is radiosurgery?
Signup and view all the flashcards
What is bipolar electrosurgery?
What is bipolar electrosurgery?
Signup and view all the flashcards
What is a bipolar diathermic sealing device?
What is a bipolar diathermic sealing device?
Signup and view all the flashcards
What is a Hotblade?
What is a Hotblade?
Signup and view all the flashcards
What is a harmonic scalpel?
What is a harmonic scalpel?
Signup and view all the flashcards
What are lasers in surgery?
What are lasers in surgery?
Signup and view all the flashcards
How does adrenaline help control bleeding?
How does adrenaline help control bleeding?
Signup and view all the flashcards
What is the mechanism of topical haemostatic agents?
What is the mechanism of topical haemostatic agents?
Signup and view all the flashcards
What is Gelfoam-Spongostan?
What is Gelfoam-Spongostan?
Signup and view all the flashcards
What is Lyostypt?
What is Lyostypt?
Signup and view all the flashcards
What is Surgicell?
What is Surgicell?
Signup and view all the flashcards
What is Surgiflo?
What is Surgiflo?
Signup and view all the flashcards
What is bone wax?
What is bone wax?
Signup and view all the flashcards
What are active topical haemostatic agents?
What are active topical haemostatic agents?
Signup and view all the flashcards
What is Tranexamic acid?
What is Tranexamic acid?
Signup and view all the flashcards
What is Desmopressin?
What is Desmopressin?
Signup and view all the flashcards
What is a tourniquet used for?
What is a tourniquet used for?
Signup and view all the flashcards
Study Notes
Surgical Haemostasis
-
Surgical haemostasis aims to stop bleeding during surgery.
-
Understanding and managing surgical blood loss is essential for successful procedures, patient safety, and preventing complications.
-
Proper technique minimizes blood loss, preserves tissue, and facilitates a clear surgical field.
-
Recognizing the signs and importance of surgical blood loss is critical.
-
Methods for measuring surgical blood loss include weighing surgical swabs, comparing dry and saturated swabs, and recording suctioned blood.
-
Limiting intraoperative haemorrhage is key, involving planning, ligation, coagulation of vessels before cutting, and gentle tissue handling.
-
Materials promote clotting, though their benefits and drawbacks should be considered.
-
Dressings can help control bleeding post-operation.
-
Haemostasis is the process of stopping bleeding.
-
It allows good visualisation and decreases surgical time.
-
Prevents post-operative infections (SSIs).
-
Good tissue apposition is vital for post-operative healing.
-
Bleeding is a normal part of surgery.
-
The extent of haemorrhage is inversely proportional to the surgeon's skill.
-
Preventative haemostasis, proper planning, and accurate dissection are vital.
-
Significant bleeding can occur unexpectedly, during or after surgery.
-
Maintaining IV access and monitoring blood pressure (BP) are crucial for volume resuscitation.
Intra-operative Haemostasis
- Proper surgical technique is crucial
- Meticulous surgical haemostasis is needed, including gentle tissue handling and appropriate instruments.
- Excellent knowledge of relevant anatomy and surgical procedure is needed.
- Normal haemostatic mechanisms must be considered.
- Awareness of diseases impacting haemostasis, such as bleeding disorders, is essential.
Intra-operative Blood Loss
- Blood loss is normal part of surgery.
- The amount of blood loss depends on the surgeon's technical skill.
- Preventative haemostasis, planning, and accurate dissection reduces blood loss.
- Significant haemorrhage could happen unexpectedly.
- Maintaining IV access and monitoring blood pressure (BP) aid volume resuscitation.
Shock
- Reduced tissue perfusion leads to reduced oxygen delivery.
- Clinical signs include sinus tachycardia/bradycardia, hypotension, poor pulse quality, cold extremities, pallor, and biochemistry changes (renal, lactate?).
- Untreated shock can be fatal.
Approach to Intra-operative Haemorrhage
- Recognizing and addressing blood loss is paramount.
- Ruling out the source of bleeding, including examining for suture malfunction, concealed bleeding, and accidental damage, is necessary.
- Restoring haemostasis is essential.
- Reversing hypothermia, shock, and other complications related to the bleeding is also critical.
Quantifying Blood Loss
- Blood loss during surgery should be estimated or measured.
- Swabs are used for assessing blood loss, and their weights are recorded.
- Blood essentially has a density similar to water (1 gram=1 ml).
- Blood losses on the floor or drapes should be estimated.
- Recorded volumes of flush use are calculated to determine blood loss.
Avoiding Surgical Bleeds
- Knowledge of the anatomy is critical prior to procedures.
- Good surgical preparation and planning are important steps.
- Appropriate surgical instruments (such as clamps and a sufficient surgical kit) and lighting are needed.
- Assistance during surgery is helpful.
- Proper tissue dissection and avoiding unnecessary cutting are important.
- Finger and blunt dissection are preferred techniques where applicable.
Prevention of Surgical Bleeds
- Awareness of potential bleeding disorders is vital.
- Pre-treating conditions like greyhounds fibrinolytic syndrome with Tranexamic Acid can be helpful, as well as being aware of breeds (e.g. Doberman Pinscher) predisposed to von Willebrand's disease.
- Other conditions that may contribute to bleeding disorders include: liver disease, platelet disorders, and coagulopathy.
Surgical Bleed (during the operation)
- Remain calm during surgical bleeds.
- Return to basic principles to determine the source of the bleed.
- Increase exposure, adjusting clips or drapes to more efficiently access the bleed.
- Ensure an assistant or additional support is available when needed.
- Use resources such as retractors, swabs, and suction to identify and isolate the source of bleeding and contain it.
Surgical Methods of Haemostasis
- Pressure (tamponade) is useful for smaller vessels and as an initial control of larger bleeds.
- Haemostatic forceps temporarily contain haemorrhage.
- Ligation techniques control bleeding with sutures.
- Vascular clips and sealing devices provide effective and rapid hemostasis in many cases; they are more precise and prevent complications.
- Electrocautery, radiosurgery and Vessel sealing devices stop bleeding via heat-based techniques.
- Topical haemostatic agents and antifibrinolytics aid in clotting and prevent breakdown of the clot.
- Tourniquets temporarily reduce blood flow in certain procedures; their use needs to be managed cautiously.
Direct Pressure (Tamponade)
- Useful for minor bleeds, initially controlling larger bleeds.
- Not suitable for major bleeds.
- Not suitable for patients who have coagulopathies.
- Compression should utilize swabs for pressure, and avoiding excessive pressure to prevent platelet migration is important.
Haemostatic Forceps
- Used to crush tissues and temporarily stop bleeding.
- Ratchets allow for proper positioning during clamping..
- Damage to surrounding vessels (vascular damage) can aid in clotting.
- Used for smaller blood vessels requiring time for normal clotting.
Using Haemostatic Forceps
- Use smallest forceps suitable for vessel size.
- Avoid unnecessary tissue grasp during use of forceps.
- Use curved forceps to maintain a clear view of the surgical site.
- Use a wide-based grip to immobilize tissues and identify bleed sources.
- Palming multiple forceps aids in management of numerous areas.
- Smaller vessels are managed using forceps tips.
- For larger vessels, forceps jaws are used.
Ligation
- Traditional and secure method of haemostasis.
- Not dependent on clot not dislodging.
- Reduces post-operative bruising.
- Maintains clear surgical field.
- Techniques include two-hand tie, one-hand tie, and instrument tie, surgeon knot, square knot, simple knot, and transfixing knot methods.
Ligating and Temporarily Occluding Vessels
- Pringle maneuver, utilizing clamps for temporary vessel occlusion is a surgical technique for preventing blood flow in the vessels, often utilized for easier surgical access or to reduce bleeding from a region.
- Clamps, bulldog clamps, and tourniquets can be used, optionally using red tubing or Penrose drains.
Different Techniques and Knots
- Two-hand: Produces good square knots, but is time-consuming and challenging for deep ligatures.
- One-hand: Creates square knots quickly but is less tactile, often used for deep ligatures.
- Knots are susceptible to loosening, which requires meticulous technique.
- Instrument tie: Easier, better-maintained knot quality, but with less tactile feel.
- Utilizes less suture material suitable for deep ligature placement.
Knots
- Square knot utilizes two opposing, similar knots.
- Reverses direction during knot tying for each knot throw.
- Maintain even tension throughout.
- Surgeon's knot loops first throw to improve security.
- Often useful in elastic or under-tension tissues.
- Bulky vascular pedicles have a reduced risk of unwrapping.
Knots (continued)
- Miller's knot loops over first layer twice with second overlap, using free end to loop and over first loop before pulling opposite directions and finish with square knots.
- Modified Miller's loops without overlaps.
- Pass free end to ensure both sides overlap before pulling in opposite directions.
Ligature Techniques
- Simple encircling creates a circular knot around the vessel.
- Modified transfixing uses a double-looping knot.
- Halsted transfixing is effective for deep-seated vessels.
- Figure-of-eight secures and holds the vessel to prevent future bleeding.
- Clamp technique often combines tightening multiple vessels, and releasing clamping for further action.
- Divide and Conquer involves dividing tissues, then tying these sutures.
- Stick ties provide an effective method for securing tissues.
Vascular Clips
- Metal clips, like Hemoclips, are used for hemostasis.
- Tissues are dissected, and vessels are clipped after determining diameter.
Electrosurgery
- Electrocautery (non-electrosurgery) is a technique for heating tissue and disrupting blood vessel walls.
- Electrosurgery/electrocoagulation uses electrical currents from the metal tip to the blood vessel.
- Heat is generated in the tissue to seal the vessel, allowing better hemostasis.
- May be better for smaller vessels, less than 2 millimeters in diameter.
Electrosurgery (diathermy)
- Monopolar operates with a ground plate under the patient.
- A current flows through the electrode and to the ground plate.
- If not properly grounded, current may cause burns.
- Requires a dry surgical field for optimal performance.
- Bipolar provides more precision for hemostasis
Radiosurgery
- Similar to electrosurgery, but uses high-frequency radio waves.
- Patient is not part of the circuit.
- No ground plate is necessary, so it does not require contact with skin.
Bipolar Diathermic Sealing Devices
- Sealing vessels up to 7mm using heat energy.
- Seals, signals with a beep, then cuts.
- Reduces risk of suture/ligature slippage.
- No foreign material left in tissues.
- Quicker surgical times than other methods, but tends to be more costly.
Hotblade
- Plugs into standard diathermy units but lacks automatic adjustment and cutting.
- Surgeon determines adequacy of coagulation visually.
- Knife uses ethylene oxide for sterilization.
- Is a cheaper option.
Other
- Harmonic scalpel uses ultrasonic energy for precise tissue cutting and coagulation.
- Lasers for surgery, provide better health and safety protocols, but are sometimes impractical.
Adrenaline
- Used to constrict small superficial wounds, or where diffusion of local bleeding is needed.
- Reduces blood flow to help clots form.
- Dilute solutions between 1:1,000 to 1:10,000. solutions are often used.
Topical Haemostatic agents
- Mechanical devices to provide pressure or tamponade to create a scaffold for clot formation are used.
- Can cause granuloma formation if used incorrectly.
- Thoroughly removed before closing the site is essential.
Topical Haemostatic Agents (continued)
- Biocompatible materials such as Gelfoam-Spongostan and Lyostypt are absorbed by the body in 3 weeks.
- Used in numerous surgical procedures like haemorrhoidectomy, and are absorbed in approximately 3 weeks.
- Bone wax temporarily blocks vascular channels
Active Topical Haemostatic Agents
- Autogenous muscle tissues are useful where tamponade, scaffold, and coagulation are required.
- Thrombin-gelatin aids blood clotting.
- Topical fibrin sealants (Evicel, Tisseel) immediately initiate clotting.
- Polyethylene glycol helps speed up coagulation
Antifibrinolytic
- Tranexamic acid (TXA) is a synthetic analogue of lysine.
- It inhibits plasminogen and prevents fibrin degradation, thus extending the duration of blood clots.
- Used primarily in greyhounds for surgery.
Coagulation Pathway Reminder
- The intrinsic and extrinsic pathways lead to the common pathway in the coagulation cascade.
- The main factors involved include Tissue factor, X, Xa, APPT, Plasminogen, Plasmin, etc.
Other
- Desmopressin increases the expression of von Willebrand's factor and Factor VIII.
- Decreases bleeding time in some breeds (e.g., some Dobermanns with vWD) and should be administered about 30 minutes before surgery.
Tourniquet
- Reduce arterial blood flow to the distal limb.
- Excessive use can cause ischemic damage (reduced blood flow leading to anaerobic respiration).
- In dogs, tourniquet time should not exceed 5 hours to avoid cardiac abnormalities or harmful potassium buildup.
- Should only be used for procedures lasting ~ 1 hour or less.
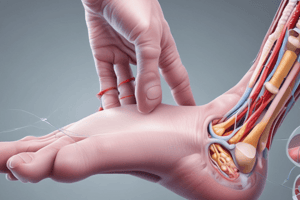
Esmarch Bandage
- Useful in lower limb surgery and digital amputation in various species, as well as in surgery of the horse.
- Exsanguination of the limb before surgery aids in efficient use.
- Bandage tightly wraps around the limb to prevent reperfusion.
Postoperative Haemorrhage (Delayed Haemorrhage)
- Ineffective haemostasis during surgery or post-surgery can lead to bleeding.
- Slipped ligatures, necrosis of the vessel and infections increase the possibility of delayed bleeding complications.
- Hypotension can mask injury in early post-operative stages, leading to delayed haemorrhage recognition.
- Inadequate secondary clot formations are common when there are blood clotting deficiencies.
Pressure
- Abdominal wraps/pressure bandages are used temporarily to control abdominal bleeding.
- They are used in haemoabdomen during surgery.
- Care must be taken to avoid impeding ventilation.
- They can reduce perfusion to abdominal organs and prevent movement; so they should have a clear purpose.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.