Podcast
Questions and Answers
In the context of surgical pathology, what is the primary rationale for performing a frozen section examination during an ongoing surgical procedure?
In the context of surgical pathology, what is the primary rationale for performing a frozen section examination during an ongoing surgical procedure?
- To facilitate comprehensive genetic sequencing of the specimen, informing personalized treatment strategies.
- To conduct a thorough macroscopic examination, ensuring adherence to standardized organ system protocols.
- To definitively determine the patient's long-term prognosis, guiding subsequent adjuvant therapies.
- To offer immediate diagnostic insights that could potentially modify the surgical approach in real-time. (correct)
A pathologist is examining a resected colon specimen and identifies tumor cells at the inked surgical margin during microscopic examination. How should this finding be communicated and what is the typical next step in management?
A pathologist is examining a resected colon specimen and identifies tumor cells at the inked surgical margin during microscopic examination. How should this finding be communicated and what is the typical next step in management?
- Report the margins as 'suspicious for malignancy,' and schedule the patient for close surveillance with serial imaging studies.
- Report the margins as 'positive for malignancy,' indicating that additional tissue removal is necessary to achieve complete tumor excision. (correct)
- Report the margins as 'indeterminate,' and recommend immediate radiation therapy to address any residual microscopic disease.
- Report the margins as 'negative for malignancy,' and proceed with adjuvant chemotherapy, as the initial resection was curative.
A surgical pathology report indicates 'T2N1M0' for a breast cancer specimen. What is the most accurate interpretation of this staging information?
A surgical pathology report indicates 'T2N1M0' for a breast cancer specimen. What is the most accurate interpretation of this staging information?
- The tumor cannot be assessed, there is no involvement of regional lymph nodes, but distant metastases are present.
- The tumor is larger, there is involvement of regional lymph nodes, but there are no distant metastases. (correct)
- The tumor is small, there are no regional lymph node metastases, and there are distant metastases.
- The tumor size is not assessed, there is extensive involvement of distant lymph nodes, and there are no distant metastases.
In surgical pathology, what is the significance of clinical-pathological correlation, and why is it essential for accurate diagnosis?
In surgical pathology, what is the significance of clinical-pathological correlation, and why is it essential for accurate diagnosis?
During a surgical resection, a pathologist identifies reactive changes in the tissue surrounding a tumor. What is the most appropriate way to interpret and report these findings?
During a surgical resection, a pathologist identifies reactive changes in the tissue surrounding a tumor. What is the most appropriate way to interpret and report these findings?
A surgeon submits a specimen labeled 'prostate biopsy.' What key clinical information should the pathologist seek before examining the specimen?
A surgeon submits a specimen labeled 'prostate biopsy.' What key clinical information should the pathologist seek before examining the specimen?
Immunohistochemistry (IHC) is performed on a tumor sample, and the results show strong positive staining for a specific marker typically associated with a different tissue type. How should this unexpected result be interpreted?
Immunohistochemistry (IHC) is performed on a tumor sample, and the results show strong positive staining for a specific marker typically associated with a different tissue type. How should this unexpected result be interpreted?
What is the central objective of surgical pathology in patient care?
What is the central objective of surgical pathology in patient care?
Which of the following scenarios would MOST warrant the use of genetic sequencing in surgical pathology?
Which of the following scenarios would MOST warrant the use of genetic sequencing in surgical pathology?
Apart from surgical specimens, biopsies, and FNA's, which of the following items might a surgical pathologist be asked to examine?
Apart from surgical specimens, biopsies, and FNA's, which of the following items might a surgical pathologist be asked to examine?
Flashcards
Surgical Pathology
Surgical Pathology
Examination of surgical specimens to diagnose and guide surgical/clinical management.
Specimen Types
Specimen Types
Major surgeries, biopsies, FNAs, cell scrapings, stents, implants, or bullet fragments.
Surgical Pathology Team
Surgical Pathology Team
Surgeons, internal medicine specialists, radiologists, dermatologists, OR nurses, technicians, pathologist assistants.
Clinical-Pathological Correlation
Clinical-Pathological Correlation
Signup and view all the flashcards
Gross Examination
Gross Examination
Signup and view all the flashcards
Microscopic Examination
Microscopic Examination
Signup and view all the flashcards
Frozen Section Examination
Frozen Section Examination
Signup and view all the flashcards
TNM Staging
TNM Staging
Signup and view all the flashcards
Negative Margins
Negative Margins
Signup and view all the flashcards
Positive Margins
Positive Margins
Signup and view all the flashcards
Study Notes
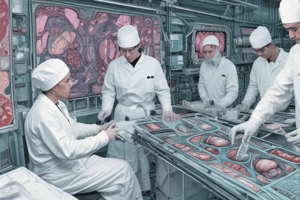
Surgical Pathology Overview
- Surgical pathology involves examining surgical specimens removed during medical procedures.
- The purpose is to diagnose conditions and guide surgical and clinical management.
- The general workflow includes specimen acquisition, examination, and diagnostic reporting for clinical decisions.
Specimen Types
- Specimens are usually obtained via a medical procedure.
- Surgical specimens include resections from major surgeries, biopsies, fine needle aspirates, cell brushings, and scrapings.
- Non-biological specimens like stents, orthopedic hardware, breast implants, and bullet fragments are also examined.
Team Involvement
- Surgeons, internal medicine specialists, interventional radiologists, dermatologists, and OB/GYN specialists may obtain specimens.
- Allied personnel like OR nurses, couriers, surgical pathology technicians, pathologist assistants, and histotechnologists are also involved.
Clinical-Pathological Correlation
- Pathologists must understand the clinical context of each case before examining specimens.
- Interpretation of diagnostic procedures, lab tests, and imaging should align with the clinical picture.
Specimen Examination
- Examination includes three major components.
- These examinations follow standardization rules that makes the results interpretable.
Macroscopic Examination
- Gross examination involves assessing anatomical origin, size, weight, color, and any visible anomalies following standardized protocols.
Microscopic Examination
- Tissue sections are frozen, sliced, stained with hematoxylin and eosin (H&E), and examined by pathologists.
- Pathologists evaluate if the tissue is benign or malignant
- Additional tests may be used such as immunohistochemistry (IHC), special stains, genetic sequencing, or electron microscopy to confirm diagnoses or specify tumor subtypes.
Intraoperative Examination
- Frozen section examination occurs during surgery, with results communicated to the surgeon within 20 minutes.
- This examination determines immediate management such as whether a mass seen on X-ray is an abscess needing drainage or a tumor needing excision plus chemotherapy/radiation.
- TNM staging is very important for tumors, where T is tumor, N is lymph node involvement, and M is metastasis.
- Results may alter the course of surgery.
Adequacy of Excision
- An important consideration is whether the entire tumor has been removed with adequate margins of normal tissue.
- Negative margins mean no tumor cells are present at the surgical margin, indicating completion.
- Positive margins signify remaining tumor cells, requiring further tissue removal.
- Some tumor markers need more than the 20-minute intraoperative timeframe, which may require additional surgeries.
Pathology Training
- AP/CP combined residency, lasting four years, is chosen by 80% of residents
- AP-only or CP-only residencies last three years
- Fellowships are typically one year, neuropathology fellowships are two years
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.