Podcast
Questions and Answers
What is the primary reason for performing induction in the lateral position during a Caesarian Section?
What is the primary reason for performing induction in the lateral position during a Caesarian Section?
- To avoid compression of the inferior vena cava (correct)
- To facilitate easier intubation
- To increase the absorption of anesthetic agents
- To maintain a higher heart rate
Which of the following is essential for avoiding aspiration during induction for a Caesarian Section?
Which of the following is essential for avoiding aspiration during induction for a Caesarian Section?
- Use of cricoid pressure (correct)
- Intubating before sedating
- Administering antiemetics
- Rapid sequence induction
What type of medications might be administered during a Caesarian Section to promote uterine contraction?
What type of medications might be administered during a Caesarian Section to promote uterine contraction?
- Ergot or oxytocin (correct)
- Nitrous oxide
- Opioids
- Antibiotics
Which surgical position is typically used for performing a hysterectomy?
Which surgical position is typically used for performing a hysterectomy?
In a hysterectomy, what is the key consideration for abdominal surgery as opposed to vaginal surgery?
In a hysterectomy, what is the key consideration for abdominal surgery as opposed to vaginal surgery?
What determines the need for compatible blood units during a hysterectomy?
What determines the need for compatible blood units during a hysterectomy?
Which of the following describes the types of Caesarian sections?
Which of the following describes the types of Caesarian sections?
What is a potential complication of respiratory impairment during dilatation and curettage (D&C)?
What is a potential complication of respiratory impairment during dilatation and curettage (D&C)?
Flashcards
Caesarian Section
Caesarian Section
A surgical delivery of a baby through an incision in the mother's abdomen.
Elective C-Section
Elective C-Section
A type of C-section performed when there are no immediate risks to the mother or baby.
Emergency C-Section
Emergency C-Section
A type of C-section performed when there are unforeseen complications during labor.
Dilatation of Cervix
Dilatation of Cervix
Signup and view all the flashcards
Curettage
Curettage
Signup and view all the flashcards
Hysterectomy
Hysterectomy
Signup and view all the flashcards
Abdominal Hysterectomy
Abdominal Hysterectomy
Signup and view all the flashcards
Vaginal Hysterectomy
Vaginal Hysterectomy
Signup and view all the flashcards
Study Notes
Cesarean Section (Under General Anesthesia)
- Preparation: Rapid preparation is needed, including adequate blood supplies and appropriate sized endotracheal tubes (ETT) and laryngoscopes (multiple sizes).
- Pre-oxygenation: Pre-oxygenate with 100% FIO2 for at least three minutes to remove nitrogen from the lungs.
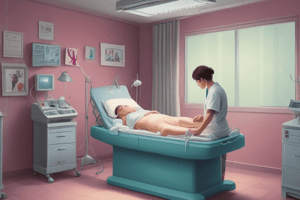
- Induction: Induction should be performed in a lateral tilt position to avoid hypotension caused by compression of the inferior vena cava and aorta by the gravid uterus (hypotensive syndrome). Supine position and relaxed abdominal wall can worsen this risk.
- Gastric content: To prevent aspiration pneumonia, crush the stomach content before giving any anesthetic induced by supine position and abdominal wall relaxation, or use the (cricoid pressure), which is better known as Mendelson's syndrome
- Post-delivery: After delivery, clamp the umbilical cord and return the patient to a suitable position,
Hysterectomy (Abdominal/Vaginal)
- Prolong surgery: Abdominal hysterectomy generally requires more extensive preparation and procedure time
- Relaxation: Good relaxation of the abdominal wall is crucial, especially during abdominal hysterectomy.
- No N/G tube: Unlike typical laparotomies, a nasogastric tube is not typically required in hysterectomies.
- Blood supply: Compatible blood units may be required
- Medical control: Controlling other medical conditions (anemia, diabetes, hypertension, hyperthyroidism) is essential before the procedure.
- Surgical Position: Vaginal hysterectomy is an extra-peritoneal operation typically done in Lithotomy position, while abdominal hysterectomy is done in a spine position
- Surgery Type: Indicate if procedure is intra-abdominal or extra-peritoneal
Indications for Cesarean Section (LSCS)
- Failure to progress: Labor may stall or not progress as expected
- Fetal distress: Non-reassuring fetal heart rate patterns
- Cephalopelvic disproportion: Baby's head is too large relative to the mother's pelvis
- Malpresentation: Baby is not positioned for vaginal delivery
- Prematurity: Premature delivery status
- Previous uterine surgery: History of uterine surgery
- Previous surgeries: History of previous operations impacting childbirth
Goals of Cesarean Section Anesthesia
- Maternal safety: Ensuring the mother's safety during surgery
- Fetal safety: Ensuring the baby's safety throughout the entire process
- Maternal comfort: Providing comfort and minimizing pain perception to the mother
- Surgical ability: Ability to perform the surgery safely under the anesthesia technique
Regional vs. General Anesthesia
- Regional anesthesia: Preferred method for C-sections as it has lower maternal mortality rates compared to general anesthesia and less risk to the neonate.
- General anesthesia: Associated with higher maternal mortality and potential issues like: airway problems, aspiration pneumonia, and high neural blockade.
- Spinal anesthesia: Rapid onset with dense neural block and minimal fetal transfer of drugs. (but can cause hypotension)
Failed Intubation
- Pregnancy-related physical changes: Physical changes from pregnancy, including weight gain, enlarged breasts, edema, oropharyngeal edema, a short neck, protruding maxillary incisors, and mandibular recession can complicate endotracheal intubation.
- Complication: A complication of labor and childbirth that causes airway obstacles.
Pre-operative Preparations
- Prophylaxis: Prophylactic medications, like ranitidine and metoclopramide, are given to prevent aspiration pneumonia
- Fasting period: Important to note the consideration of patient's fasting period before induction to prevent aspiration.
- Medication: Oral Omeprazole is given to reduce lower esophageal sphincter tone to avoid aspiration complications
General Anesthesia Technique Suggestions
- Nonparticulate antacid: Initial administration of a nonparticulate antacid is required.
- Monitoring: Monitor the patient's physiological parameters (ECG, pulse oximetry, and capnography).
- Airway management: Maintain correct airway position by left uterine displacement.
- Oxygenation: De-nitrogenate the patient's lungs with high-flow oxygen for several minutes (3-5).
General Anesthesia Technique
- Rapid sequence induction: Rapid-sequence induction with thiopental and succinylcholine, followed by cricoid pressure until the correct placement of endotracheal tube.
- Muscle relaxation: Muscle relaxation as necessary using either a nondepolarizing or succinylcholine.
- Ventilatory support: Maintaining normocarbia (normal blood CO2 levels) using appropriate ventilation is required during surgery.
- Positioning + Airway: Positioning and maintaining optimal airway position are crucial.
- Emergencies: In emergencies, appropriate management of issues like fetal distress or abnormal haemorrhaging requires meticulous management.
- Post-delivery: Reduce nitrous oxide, discontinue volatile anesthetics, give opioid or benzodiazepine
- Other fluids: Add oxytocin to intravenous fluids, which facilitates uterine contraction after delivery.
- Intubation Failure: Address complications like failed intubation with appropriate measures like waking up the patient and changing or providing alternate methods.
Failed Intubation Drill
- Airway management: Maintain cricoid pressure, oxygenate with facemask and turn to left side with head down.
- Emergency response: Manage complications such as fetal distress or antepartum haemorrhage with the appropriate techniques and measures, such as re-establish spontaneous respiration after suxamethonlum.
- Alternative techniques: Use a regional technique if problems with the airway are encountered.
- Continuous oxygenation: Ensure continuous oxygenation for the patient.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.