Podcast
Questions and Answers
A child presents with right torticollis. Which of the following is the MOST likely resting posture of their neck?
A child presents with right torticollis. Which of the following is the MOST likely resting posture of their neck?
- Left lateral flexion and left rotation
- Left lateral flexion and right rotation
- Right lateral flexion and right rotation
- Right lateral flexion and left rotation (correct)
Which of the following is a DIFFERENTIAL diagnosis for congenital muscular torticollis?
Which of the following is a DIFFERENTIAL diagnosis for congenital muscular torticollis?
- Plagiocephaly
- Klippel-Feil Syndrome (correct)
- Developmental dysplasia of the hip
- Brachycephaly
What is the MOST important aspect of physical therapy for an infant with torticollis?
What is the MOST important aspect of physical therapy for an infant with torticollis?
- Aggressive stretching of the affected SCM
- Strengthening exercises for the neck muscles
- Caregiver education (correct)
- Use of positioning devices
A physical therapist observes that an infant with torticollis consistently turns their head to the right during visual tracking activities. Which intervention is MOST appropriate to address this?
A physical therapist observes that an infant with torticollis consistently turns their head to the right during visual tracking activities. Which intervention is MOST appropriate to address this?
Which finding would be a RED FLAG, suggesting a cause OTHER than congenital muscular torticollis?
Which finding would be a RED FLAG, suggesting a cause OTHER than congenital muscular torticollis?
What would the expected finding with PROM be for an infant with right torticollis?
What would the expected finding with PROM be for an infant with right torticollis?
Which cranial deformation is characterized by ipsilateral occipital flattening and contralateral frontal bossing?
Which cranial deformation is characterized by ipsilateral occipital flattening and contralateral frontal bossing?
An infant with a history of torticollis presents with a flattened occiput, open sutures, and anteriorly displaced ear. Which type of cranial deformation is MOST likely?
An infant with a history of torticollis presents with a flattened occiput, open sutures, and anteriorly displaced ear. Which type of cranial deformation is MOST likely?
An infant who had torticollis is now 14 months old and walking. According to the guidelines, when should reassessment occur post-discharge from physical therapy?
An infant who had torticollis is now 14 months old and walking. According to the guidelines, when should reassessment occur post-discharge from physical therapy?
A 3-month-old infant is being treated for torticollis. Which Muscle Function Scale (MFS) score would be considered within the normal range for this age?
A 3-month-old infant is being treated for torticollis. Which Muscle Function Scale (MFS) score would be considered within the normal range for this age?
A parent reports that their infant with torticollis seems to have an increased head tilt when they are tired or sick. What is the BEST course of action?
A parent reports that their infant with torticollis seems to have an increased head tilt when they are tired or sick. What is the BEST course of action?
Which of the following is an example of an environmental modification to encourage cervical rotation to the left for an infant with right torticollis?
Which of the following is an example of an environmental modification to encourage cervical rotation to the left for an infant with right torticollis?
A 5-month-old infant presents with torticollis and has not yet achieved the ability to roll from prone to supine. Which intervention is MOST appropriate?
A 5-month-old infant presents with torticollis and has not yet achieved the ability to roll from prone to supine. Which intervention is MOST appropriate?
What is the MOST likely reason for an increased incidence of cranial deformation since 1994?
What is the MOST likely reason for an increased incidence of cranial deformation since 1994?
A physical therapist is examining an infant with torticollis and notices asymmetrical skin folds in the infant's groin area. What condition should the physical therapist screen for?
A physical therapist is examining an infant with torticollis and notices asymmetrical skin folds in the infant's groin area. What condition should the physical therapist screen for?
Why are children diagnosed with CMT at risk for motor developmental delays?
Why are children diagnosed with CMT at risk for motor developmental delays?
What is the MOST appropriate initial intervention for an infant diagnosed with postural torticollis?
What is the MOST appropriate initial intervention for an infant diagnosed with postural torticollis?
If an infant has a posterior displaced ear, and a closed lambdoid suture, what is the MOST likely diagnosis?
If an infant has a posterior displaced ear, and a closed lambdoid suture, what is the MOST likely diagnosis?
Which of the following interventions has the WEAKEST evidence to support its use in the treatment of CMT?
Which of the following interventions has the WEAKEST evidence to support its use in the treatment of CMT?
An infant is diagnosed with Sandifer syndrome. This condition is MOST likely associated with:
An infant is diagnosed with Sandifer syndrome. This condition is MOST likely associated with:
A physical therapist is assessing an infant with torticollis. Which of the following findings would necessitate a referral to a pediatric ophthalmologist?
A physical therapist is assessing an infant with torticollis. Which of the following findings would necessitate a referral to a pediatric ophthalmologist?
What is MOST commonly associated with a SCM mass (fibrous tumor) that appears with CMT?
What is MOST commonly associated with a SCM mass (fibrous tumor) that appears with CMT?
A parent reports that their 6-month-old infant with torticollis strongly prefers looking to the right and consistently resists looking to the left. What AROM exercises would be MOST beneficial?
A parent reports that their 6-month-old infant with torticollis strongly prefers looking to the right and consistently resists looking to the left. What AROM exercises would be MOST beneficial?
A child with torticollis is being treated with a cranial molding helmet. What is the MINIMUM number of hours per day treatment that the helmet should be worn?
A child with torticollis is being treated with a cranial molding helmet. What is the MINIMUM number of hours per day treatment that the helmet should be worn?
Which of the following is a PRIMARY goal of trunk AROM exercises in the treatment of CMT?
Which of the following is a PRIMARY goal of trunk AROM exercises in the treatment of CMT?
A physical therapist is treating a 4 week old infant with torticollis. How often should the baby receive direct physical therapy?
A physical therapist is treating a 4 week old infant with torticollis. How often should the baby receive direct physical therapy?
Which of the following findings during a systems review would warrant further investigation for a gastrointestinal issue in an infant with torticollis?
Which of the following findings during a systems review would warrant further investigation for a gastrointestinal issue in an infant with torticollis?
When providing PROM to an infant with torticollis, what is the MOST important consideration to prevent complications?
When providing PROM to an infant with torticollis, what is the MOST important consideration to prevent complications?
Flashcards
SCM Origin
SCM Origin
Mastoid process of temporal bone and lateral half of superior nuchal line.
SCM Insertion
SCM Insertion
-Sternal head: manubrium of sternum. -Clavicular head: medial third of the clavicle
SCM Innervation
SCM Innervation
Spinal accessory nerve (motor) & C2,C3 (pain and proprioception)
SCM Action
SCM Action
Signup and view all the flashcards
Right SCM Contraction
Right SCM Contraction
Signup and view all the flashcards
Left SCM Contraction
Left SCM Contraction
Signup and view all the flashcards
Right Torticollis
Right Torticollis
Signup and view all the flashcards
Left Torticollis
Left Torticollis
Signup and view all the flashcards
Postural Torticollis
Postural Torticollis
Signup and view all the flashcards
Muscular Torticollis
Muscular Torticollis
Signup and view all the flashcards
Torticollis with SCM Mass
Torticollis with SCM Mass
Signup and view all the flashcards
CMT with SCM Mass
CMT with SCM Mass
Signup and view all the flashcards
Torticollis Risk Factors
Torticollis Risk Factors
Signup and view all the flashcards
Untreated Torticollis
Untreated Torticollis
Signup and view all the flashcards
Klippel-Feil Syndrome
Klippel-Feil Syndrome
Signup and view all the flashcards
Ocular Torticollis
Ocular Torticollis
Signup and view all the flashcards
Benign Paroxysmal Torticollis
Benign Paroxysmal Torticollis
Signup and view all the flashcards
Sandifer Syndrome
Sandifer Syndrome
Signup and view all the flashcards
Neurological Causes
Neurological Causes
Signup and view all the flashcards
Subjective History
Subjective History
Signup and view all the flashcards
Associated Conditions Screening
Associated Conditions Screening
Signup and view all the flashcards
Examination-systems review
Examination-systems review
Signup and view all the flashcards
Examination-systems review continued
Examination-systems review continued
Signup and view all the flashcards
DDH Signs/Symptoms
DDH Signs/Symptoms
Signup and view all the flashcards
Cervical ROM
Cervical ROM
Signup and view all the flashcards
Body Structure Examination
Body Structure Examination
Signup and view all the flashcards
Muscle Function Scale (MFS) 0
Muscle Function Scale (MFS) 0
Signup and view all the flashcards
Muscle Function Scale (MFS) 4
Muscle Function Scale (MFS) 4
Signup and view all the flashcards
Early PT Impact
Early PT Impact
Signup and view all the flashcards
1st Choice Interventions for CMT
1st Choice Interventions for CMT
Signup and view all the flashcards
Study Notes
- The content provided is a muscle guide for the Sternocleidomastoid (SCM) muscle, torticollis, cranial deformities, and associated interventions.
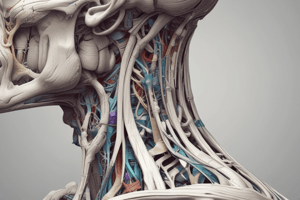
SCM Muscle
- Originates from the mastoid process of the temporal bone and the lateral half of the superior nuchal line.
- The sternal head inserts on the manubrium of the sternum.
- The clavicular head inserts on the medial third of the clavicle.
- Innervated by the spinal accessory nerve for motor function, and C2/C3 for pain and proprioception.
- Bilateral action causes cervical flexion and capital extension.
- Unilateral contraction results in ipsilateral sidebending/lateral flexion and contralateral rotation of the neck.
Unilateral SCM Contraction
- Right SCM contraction leads to right sidebending and left rotation.
- Left SCM contraction leads to left sidebending and right rotation.
Congenital Muscular Torticollis (CMT) Naming
- Right torticollis involves the right SCM, resulting in right lateral flexion and left rotation, with limited left lateral flexion and right rotation.
- Left torticollis involves the left SCM, resulting in left lateral flexion and right rotation, with limited right lateral flexion and left rotation.
Types of Torticollis
- Postural torticollis involves a postural preference of cervical lateral flexion and/or rotation, but muscle flexibility and ROM are normal.
- Muscular torticollis involves cervical lateral flexion and/or rotation with SCM tightness and ROM limitations.
- SCM mass involves cervical lateral flexion and/or rotation with fibrotic thickening of the SCM (palpable mass/bump) and ROM limitations.
- CMT with SCM mass is a congenital, benign, nontender fibrous tumor in the SCM, associated with breech presentation or forceps/vacuum delivery.
Torticollis Risk Factors
- Large baby
- Multiple babies
- Breech position
- Birth trauma
- Vacuum or forceps delivery
Untreated Torticollis Complications
- Craniofacial deformities
- Asymmetrical postures
- Developmental delay
- Plagiocephaly
- Asymmetrical ears (one anterior and one posterior)
- Uneven eyes
- Cervical &/or thoracic scoliosis
- Uneven shoulders
- Uneven weight bearing through pelvis
- Children diagnosed with CMT are at risk for motor developmental delays
Importance of Screening
- Up to 18% of children with asymmetrical head and neck posture may have a non-muscular cause.
- Establishing an accurate diagnosis is essential
Torticollis Differential Diagnosis
- Klippel-Feil Syndrome
- Ocular Torticollis
- Benign paroxysmal torticollis
- Sandifer syndrome
- Neurological causes
Klippel-Feil Syndrome
- Abnormal fusion of 2 or more cervical vertebrae (Red Flag).
- Associated with short neck, low hairline, cervical spine ROM limitations.
- May also involve kidney, rib & heart abnormalities, hearing problems, congenital scoliosis.
Ocular Torticollis
- Compensatory abnormal head/neck posture used to improve vision &/or maintain binocular vision.
- Onset is later than CMT
- Neck ROM is not limited
- Usually associated w/ nystagmus or strabismus
- Screen by checking oculomotor function (visual tracking, smooth pursuit)
Benign Paroxysmal Torticollis
- Recurrent episodes of head tilt to the same or opposite side.
- Accompanied by nausea, vomiting, crying and migraines later in life.
Sandifer Syndrome
- Recurrent episodes of dystonia of the neck (R cervical rotation) with back arching, especially after eating.
- Occurs secondary to GERD, a position of comfort for infants with reflux.
Neurological Causes of Torticollis
- Screen for brachial plexus injury (head turned away from affected UE), CNS lesions (tumors in brain, brainstem, cerebellum).
- Pain with movement (CMT is not painful).
- Atypical or asymmetrical muscle tone and retained primitive reflexes.
- Signs of brachial plexus injury (decreased movement &/or posturing of one UE, decreased sensation in an UE).
Torticollis Subjective History
- Chronological age (corrected if premature) and age of symptom onset.
- Pregnancy and birth history (fetal movement, multiple pregnancies, cephalic or breech, forceps or vacuum, low birth weight).
- Head posture/preference & head or facial asymmetry.
- Other known/suspected congenital, developmental, or medical conditions.
- Developmental milestones.
Torticollis Associated Conditions Screening
- Cranial deformities
- Developmental dysplasia of the hip
- Brachial plexus injury
- Foot deformities
- Early motor delays
- TMJ dysfunction
Torticollis Examination-Systems Review
- Musculoskeletal (symmetrical face, skull, spine, shoulders, hips, symmetrical ROM, SCM palpation).
- Neurological (tone, BPI, temperament, visual tracking).
- Integumentary (skin folds of hip and neck symmetry, color, condition).
- Cardiopulmonary (rib cage expansion, clavicle movement).
- Communication (facial expression, cry).
- Movement (symmetrical and full AROM in all positions).
- G-I (Hx of GERD or difficulty feeding from one side).
Developmental Dysplasia of Hip Risk Factors
- Breech birth
- Large babies
- Cultures that swaddle
- Signs/Sx: asymmetrical skin folds, hip popping/clicking, limited hip ABD ROM, leg length discrepancy
Torticollis Examination-Body Structures
- Bilateral cervical AROM of lateral flexion and rotation.
- Bilateral cervical PROM of lateral flexion (110°) and rotation (70°).
- Posture in and tolerance to supine, prone, sitting, and standing.
- PROM/AROM of trunk, UEs, LEs.
- Pain or discomfort.
- Skin integrity, SCM mass.
- Craniofacial asymmetry & head/skull shape.
Muscle Strength of Lateral Flexors measured by Muscle Function Scale (MFS)
- 0: Below the horizontal line (0° to 15° to >45°).
- 4: High above the horizontal line, more than 45° (>45° to 75°).
Norms for Muscle Function Strength/Endurance at Ages
- 2 months: Mean 1.0, Range 0-2.
- 4 months: Mean 2.6, Range 1-4.
- 6 months: Mean 3.0, Range 2-4.
- 10 months: Mean 3.4, Range 3-4.
Torticollis Examination-Participation
- Positioning when awake & asleep.
- Time in prone when awake.
- Ability to alternate sides when breastfeeding or bottle feeding.
- Time spent in equipment/positioning devices.
Torticollis Prognosis
- PT starts before 1 month, often 1x/wk.
- Most important aspect of PT=>caregiver education.
First Choice Interventions for CMT
- Neck PROM when PROM is limited
- Neck & trunk AROM
- Developmental of symmetrical movements
- Environmental adaptations
- Caregiver education
Neck PROM
- Should be performed frequently throughout the day
- Slow, gentle, pain-free stretches
- Stabilize head & shoulders to prevent compensations
- Can be performed in a variety of positions
- Contraindications to PROM: c-spine bony abnormalities, clavicle fracture, tumors, Arnold-chiari malformation
Neck & Trunk AROM
- Goal: strengthen neck and trunk muscles
- Activities: positioning, carrying, eating & play
- Cervical Rotation: Visual tracking to non-preferred side, feeding from non-preferred side
- Cervical lateral flexion: practice righting reactions to non-preferred side
- Minimize time in positioning devices & encourage prone play
Development of Symmetrical Movements
- Facilities symmetrical age-appropriate motor skills
- Prevent asymmetry with prone, sitting, crawling & walking
- Transition to the right and left b/w all developmental positions
Environmental Modifications
- Alternate infant’s position in crib & changing tables
- Minimize time in positioning devices
- When used, positioning devices must be used with attention to infant symmetry & encourage cervical rotation to the non-preferred side
- Maximize awake time in prone (goal=at least 1 cumulative hour of tummy time per day)
Caregiver Education
- Educate about:
- CMT
- Tummy time when awake
- Minimize time in infant positioning equipment
- Alternate sides when feeding
- Create individualized home program with family structure & schedule in mind
Torticollis Outcomes & PT Discontinuation Criteria
- Cervical PROM is within 5° of the unaffected side.
- Symmetrical movement patterns are present.
- Age-appropriate gross motor skills are present.
- No visible head tilt.
- Caregivers demonstrate understanding of how to monitor their child as they grow.
Reassessment After Torticollis Treatment
- Re-assess 3-12 months after discontinuation or when the child starts walking.
- Assess postural symmetry, functional abilities, caregiver understanding of home exercises/monitoring, and caregiver satisfaction.
- If all criteria met, discharge from PT; if not, restart direct PT services.
Notes on Intermittent Head Tilt
- May return with illness, fatigue, or when learning a new motor skill.
Cranial Deformation
- Distortion of head shape due to mechanical forces prenatally or postnatally.
- Associated with CMT, prematurity, multiple births, firstborn children.
- Increased incidence after 1994 "Back to Sleep" campaign.
- Decreased time in prone and increased time in supine
- 80% of brain/skull growth occurs before 12 mos of age.
- Skull is most malleable prior to 3 mos of age and brain growth slows at 5-6 mos.
Types of Cranial Deformation
- Plagiocephaly: Ipsilateral occipital flattening & contralateral occipital bossing
- Brachycephaly: Central occipital flattening
- Dolichocephaly: Long & narrow skull
Positional/Deformational Plagiocephaly
- Asymmetrical head shape and facial asymmetry-parallelogram shape.
- Jaw, ears & eye mal-alignment (ear on posterior flat side moves anterior).
- Associated with CMT, prematurity, multiple births.
Craniosynostosis (Red Flag)
- Premature closure of one or more cranial sutures causing cranial asymmetry.
- Sx: slow or no head growth.
- Raised ridge on skull along suture and abnormal skull shape.
- Positional Molding: frontal protuberance, ear displaced anteriorly, flattened occiput, all sutures open, posterior protuberance
- Lambdoid Synostosis: frontal protuberance, ear displaced posteriorly, mastoid protuberance, closed lambdoid suture, posterior protuberance
Craniofacial Assessment
- Palpate anterior and posterior fontanelles (size, shape, position, fullness).
- Palpate cranial sutures (look for ridging).
- Visual assessment of craniofacial symmetry (take photos of 6 views) or use standardized assessment.
- Reassess monthly.
Cranial Deformation Evidence Based Recommendations
- Decrease pressure on flat spots by encouraging more tummy time and less time in positioning equipment.
- Treat CMT, if present.
- Cranial molding helmets initiated when skull is rapidly growing (4-6 months), worn 20-23 hours per day.
- Poorer outcomes associated with older age, greater severity, and poor adherence.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.