Podcast
Questions and Answers
What is the maximum percentage of abnormal sperm forms permissible in semen?
What is the maximum percentage of abnormal sperm forms permissible in semen?
- 50%
- 20% (correct)
- 30%
- 10%
What condition is characterized by the complete absence of sperm in semen?
What condition is characterized by the complete absence of sperm in semen?
- Spermatogenesis
- Necrospermia
- Azospermia (correct)
- Oligospermia
Which stage of oogenesis takes place in the ovary after birth?
Which stage of oogenesis takes place in the ovary after birth?
- First meiotic division
- Post-natal maturation (correct)
- Proliferation
- Growth
At what point does the primary oocyte complete prophase of the first meiotic division?
At what point does the primary oocyte complete prophase of the first meiotic division?
How many primary oocytes are present in each ovary at birth?
How many primary oocytes are present in each ovary at birth?
What is the main hormone secreted by the theca interna?
What is the main hormone secreted by the theca interna?
What term describes the fluid-filled cavity that separates granulosa cells in a growing follicle?
What term describes the fluid-filled cavity that separates granulosa cells in a growing follicle?
During which phase does the corpus luteum secrete progesterone?
During which phase does the corpus luteum secrete progesterone?
What happens to most of the follicles during an ovarian cycle?
What happens to most of the follicles during an ovarian cycle?
What does the secretory stage of the uterine cycle primarily depend on?
What does the secretory stage of the uterine cycle primarily depend on?
Flashcards
Spermatogenesis lifespan
Spermatogenesis lifespan
Sperm viability (ability to fertilize) lasts for 48 hours after ejaculation.
Abnormal sperm percentage
Abnormal sperm percentage
Abnormal sperm forms (giant, dwarf, bicephalic) should constitute no more than 20% of the total sperm count.
Oogenesis definition
Oogenesis definition
Oogenesis is the process of transforming oogonia (primitive female germ cells) into secondary oocytes (capable of fertilization) within the ovaries.
Oogenesis starting point
Oogenesis starting point
Signup and view all the flashcards
Primary oocyte formation in fetal oogenesis.
Primary oocyte formation in fetal oogenesis.
Signup and view all the flashcards
What are granulosa cells?
What are granulosa cells?
Signup and view all the flashcards
What is the function of the theca interna?
What is the function of the theca interna?
Signup and view all the flashcards
What is the corpus luteum?
What is the corpus luteum?
Signup and view all the flashcards
What is the stage of menstruation?
What is the stage of menstruation?
Signup and view all the flashcards
What is the uterine cycle?
What is the uterine cycle?
Signup and view all the flashcards
Study Notes
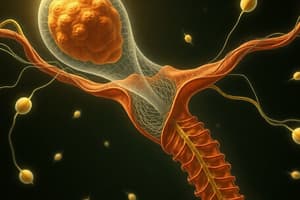
Spermatogenesis
- A process producing motile spermatozoa from primordial male germ cells (spermatogonia).
- Includes stages transforming spermatogonia to sperm in the testis.
- Begins after puberty and continues into old age.
- Duration: approximately 60-64 days (including spermiogenesis).
- Location: seminiferous tubules of the testis.
- Four stages: proliferation, growth, maturation, transformation
Stage of Proliferation
- Spermatogonium divides by mitosis to form two daughter spermatogonia.
- Each contains 23 pairs of chromosomes (2n).
Stage of Growth
- Daughter spermatogonia enlarge to form primary spermatocytes (2n).
- Largest germ cells in the seminiferous tubules.
Stage of Maturation
- Two stages of division;
- First meiotic division: primary spermatocyte divides into two secondary spermatocytes (each with 23 chromosomes).
- Second meiotic division: each secondary spermatocyte divides to form two spermatids (each with 23 chromosomes).
Stage of Transformation (Spermiogenesis)
- Spermatids change shape to form motile sperms:
- Nucleus condenses to form head.
- Golgi complex aggregates forming acrosome (enzyme-containing vesicle).
- Centrioles form axial filament (for tail).
- Mitochondria form helical sheath in midpiece.
- Cytoplasm shed.
Structure of Sperm
- Head: acrosome and nucleus.
- Neck: centrioles.
- Body: mitochondria (middle piece).
- Tail: axial filament (end piece).
Seminal Fluid
- Composed of spermatozoa and fluid secretions from accessory sex glands (seminal vesicles, prostate, bulbourethral glands).
- Alkaline fluid containing fructose and vitamin C.
- Normal ejaculate: 3-5 cc, containing ~100 million sperm/cc.
Anomalies of Spermatogenesis
- Abnormal sperm forms (giant, dwarf, bicephalic): not exceeding 20% of total sperm count.
- Necrospermia: dead sperm in the ejaculate.
- Oligospermia: low sperm count.
- Azoospermia: complete absence of sperm.
Oogenesis
- A process of differentiating oogonia cells (primordial female germ cells) into oocytes (ready for fertilization) in the ovary.
- Begins during fetal life (3rd month).
- Continues after puberty during the ovarian cycle.
- Ends at menopause.
- Takes place in the ovary
Ovarian Cycle (General)
- Regulated by FSH and LH hormones from the pituitary gland, with estrogen and progesterone secreted by the ovary.
- Consists of follicular and luteal phases (about 28 days in total).
Ovarian Cycle Phases
- Follicular phase (14 days): development of a follicle.
- Ovulation: release of the secondary oocyte.
- Luteal phase (14 days): formation of the corpus luteum
Ovulation
- Rupture of the Graafian follicle releasing the secondary oocyte.
- Usually occurs on day 14 of the menstrual cycle.
- Some women experience pain (middle pain).
- Basal body temperature rises (37.5°C).
Implantation
- Process of the blastocyst embedding into the uterine wall's posterior wall—usually.
- Occurs typically 6-7 days after fertilization.
- Trophoblast cells adhere to uterine wall, eroding endometrium, and progressively penetrating it.
The Decidua
- Modified endometrium of the pregnant uterus (gravid endometrium).
- Consists of three layers: capsularis, basalis, and parietalis.
- Supports and nourishes the developing embryo.
- Formed in response to implantation.
Cleavage of the Zygote
- Repeated mitotic divisions of a zygote into blastomeres.
- Blastomeres become smaller with each division.
- Zona pellucida maintains blastomeres together.
- The process begins ~30 hours after fertilization.
Formation of Bilaminar Embryonic Disc
- The embryoblast differentiates into two layers: epiblast and hypoblast, creating a bilaminar embryonic disk structure.
- Amniotic cavity and yolk sac cavities form.
- Extraembryonic membranes (amnion, yolk sac, chorion) form and surround the embryo.
Development of chorionic villi
- Extensions of the chorion projecting into the uterine lining.
- The villi are responsible for nutrient exchange.
- Develop from the syncytiotrophoblast and cytotrophoblast layers.
Development of the Placenta
- Formed from the chorion frondosum (fetal part) and decidua basalis (maternal part) components
Placental Circulation
- Oxygenated and nutrient-rich fetal blood circulates to the placenta through umbilical arteries.
- Gaseous exchange occurs in the intervillous space between maternal and fetal blood.
- Oxygenated blood returns to the fetus via the umbilical vein.
Anomalies of the Placenta
- Abnormal placental attachment (placenta previa).
- Abnormal distribution of chorionic villi (diffuse or divided placenta).
- Abnormal cord attachment (velamentous or battledore).
- Chorion epithelioma (rare malignant tumor).
Twins
- Two or more offspring developing from a single or multiple ovum/s and sperm/s.
- Can be identical (monozygotic) or fraternal (dizygotic), depending on the origin.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.