Podcast
Questions and Answers
Which condition involves bleeding into a joint space?
Which condition involves bleeding into a joint space?
- Hemarthrosis (correct)
- Ganglion
- Bursitis
- Contusion
A ballooning of the wall of a joint capsule or tendon sheath is characteristic of which of the following conditions?
A ballooning of the wall of a joint capsule or tendon sheath is characteristic of which of the following conditions?
- Bursitis
- Contusion
- Ganglion (correct)
- Adhesion
What is the primary characteristic of a Grade 1 tissue injury?
What is the primary characteristic of a Grade 1 tissue injury?
- Joint dysfunction due to loss of mobility
- Mild pain at the time of injury with mild swelling (correct)
- Moderate pain requiring stopping the activity
- Severe pain with immediate cessation of activity
Which of the following describes an adaptive shortening of soft tissues that restricts normal movement?
Which of the following describes an adaptive shortening of soft tissues that restricts normal movement?
What occurs when collagen fibers abnormally bind to surrounding tissues?
What occurs when collagen fibers abnormally bind to surrounding tissues?
Increased pressure in a closed, nonexpanding compartment that compromises the function of blood vessels, muscles, and nerves is known as:
Increased pressure in a closed, nonexpanding compartment that compromises the function of blood vessels, muscles, and nerves is known as:
Which of these describes a prolonged muscle contraction due to local circulatory and metabolic changes?
Which of these describes a prolonged muscle contraction due to local circulatory and metabolic changes?
What is the defining characteristic of a Grade 2 tissue injury in terms of pain and activity?
What is the defining characteristic of a Grade 2 tissue injury in terms of pain and activity?
During the initial stages of muscular endurance exercises, what type of range of motion should be used?
During the initial stages of muscular endurance exercises, what type of range of motion should be used?
What is a common cause of restricted motion during the repair process?
What is a common cause of restricted motion during the repair process?
Which of the following is NOT a typical intervention for restricted motion?
Which of the following is NOT a typical intervention for restricted motion?
What is a critical aspect of the therapist's role during the stage of healing where low-intensity activities are being resumed?
What is a critical aspect of the therapist's role during the stage of healing where low-intensity activities are being resumed?
Which of these is a characteristic of the chronic stage of healing?
Which of these is a characteristic of the chronic stage of healing?
What may be felt when testing tight structures at the end of their available range during the chronic stage?
What may be felt when testing tight structures at the end of their available range during the chronic stage?
Which factor does NOT directly influence the remodeling time of tissue?
Which factor does NOT directly influence the remodeling time of tissue?
What happens to collagen fibers during the maturation of tissue?
What happens to collagen fibers during the maturation of tissue?
At what point is scar tissue generally considered unresponsive to remodeling?
At what point is scar tissue generally considered unresponsive to remodeling?
Which of the following best describes the progression of exercises, in terms of intensity, in rehabilitation?
Which of the following best describes the progression of exercises, in terms of intensity, in rehabilitation?
What is the primary focus when progressing stretching during the remodeling phase?
What is the primary focus when progressing stretching during the remodeling phase?
During the progression of strengthening exercises, what should be simulated to progress the patient appropriately?
During the progression of strengthening exercises, what should be simulated to progress the patient appropriately?
In the context of returning to high-demand activities, how should exercises be progressed?
In the context of returning to high-demand activities, how should exercises be progressed?
What are important aspects of patient education during the chronic phase of healing?
What are important aspects of patient education during the chronic phase of healing?
Which of the following is essential to consider when progressing exercises?
Which of the following is essential to consider when progressing exercises?
What is a key component of exercises designed when returning a patient to high demand activities?
What is a key component of exercises designed when returning a patient to high demand activities?
What is a primary characteristic of muscle setting during low-dosage joint mobilization?
What is a primary characteristic of muscle setting during low-dosage joint mobilization?
How does massage potentially assist in preventing adhesions when cautiously applied to injured tissue?
How does massage potentially assist in preventing adhesions when cautiously applied to injured tissue?
Which exercise may be applied at an appropriate dosage to muscles not directly related to the injured tissue?
Which exercise may be applied at an appropriate dosage to muscles not directly related to the injured tissue?
When do signs of inflammation start to progressively decrease during the subacute stage of healing?
When do signs of inflammation start to progressively decrease during the subacute stage of healing?
What might a patient experience when encountering tissue resistance at the end of their available ROM during the subacute stage?
What might a patient experience when encountering tissue resistance at the end of their available ROM during the subacute stage?
During the subacute stage, what is a key characteristic of the newly formed collagen?
During the subacute stage, what is a key characteristic of the newly formed collagen?
Why is it important to be mindful of tensile loading force during the subacute stage?
Why is it important to be mindful of tensile loading force during the subacute stage?
How long does wound closure typically take in tendons and ligaments?
How long does wound closure typically take in tendons and ligaments?
Which of the following is the primary goal of exercises during the subacute phase of tissue healing?
Which of the following is the primary goal of exercises during the subacute phase of tissue healing?
What is the MOST important characteristic of pain that must be achieved before initiating active exercises and stretching?
What is the MOST important characteristic of pain that must be achieved before initiating active exercises and stretching?
During the subacute phase, what is the recommended placement of a joint during submaximal isometric exercises?
During the subacute phase, what is the recommended placement of a joint during submaximal isometric exercises?
Which of the following best characterizes the progression of exercises as they are introduced during the subacute phase?
Which of the following best characterizes the progression of exercises as they are introduced during the subacute phase?
What factor should be considered when progressing exercises in the subacute phase if symptoms increase?
What factor should be considered when progressing exercises in the subacute phase if symptoms increase?
What type of exercises are recommended to initiate active range of motion in the subacute phase?
What type of exercises are recommended to initiate active range of motion in the subacute phase?
What should be kept in mind regarding the range of motion and strength of muscles during active range of motion exercises?
What should be kept in mind regarding the range of motion and strength of muscles during active range of motion exercises?
Why is patient education important during the subacute phase of recovery and rehabilitation?
Why is patient education important during the subacute phase of recovery and rehabilitation?
What is a primary characteristic of cumulative trauma leading to chronic recurring pain?
What is a primary characteristic of cumulative trauma leading to chronic recurring pain?
Which of the following is a major cause of chronic inflammation related to cumulative trauma?
Which of the following is a major cause of chronic inflammation related to cumulative trauma?
Returning to high-demand activities too soon after an injury can cause what?
Returning to high-demand activities too soon after an injury can cause what?
Which factor is NOT identified as a contributing factor to cumulative trauma?
Which factor is NOT identified as a contributing factor to cumulative trauma?
During the acute phase of chronic inflammation due to cumulative trauma, what is a critical step in addition to rest and modalities?
During the acute phase of chronic inflammation due to cumulative trauma, what is a critical step in addition to rest and modalities?
In subacute and chronic stages of chronic inflammation, focusing on muscle endurance is important because of which reason?
In subacute and chronic stages of chronic inflammation, focusing on muscle endurance is important because of which reason?
What is the primary purpose of work-conditioning and work-hardening programs in relation to cumulative trauma and chronic pain?
What is the primary purpose of work-conditioning and work-hardening programs in relation to cumulative trauma and chronic pain?
What can muscle guarding indicate in the context of subacute and chronic inflammation?
What can muscle guarding indicate in the context of subacute and chronic inflammation?
Flashcards
Hemarthrosis
Hemarthrosis
Bleeding into a joint.
Ganglion
Ganglion
Ballooning of the wall of a joint capsule sheath.
Bursitis
Bursitis
Inflammation of a bursa.
Contusion
Contusion
Signup and view all the flashcards
Dysfunction
Dysfunction
Signup and view all the flashcards
Joint Dysfunction
Joint Dysfunction
Signup and view all the flashcards
Contracture
Contracture
Signup and view all the flashcards
Adhesions
Adhesions
Signup and view all the flashcards
Subacute Phase Exercises
Subacute Phase Exercises
Signup and view all the flashcards
Patient Education in Subacute Phase
Patient Education in Subacute Phase
Signup and view all the flashcards
Pain Management in Subacute Phase
Pain Management in Subacute Phase
Signup and view all the flashcards
Submaximal Isometric Exercises
Submaximal Isometric Exercises
Signup and view all the flashcards
Active ROM Exercises
Active ROM Exercises
Signup and view all the flashcards
Multiple-angle Exercises
Multiple-angle Exercises
Signup and view all the flashcards
Monitoring Exercise Response
Monitoring Exercise Response
Signup and view all the flashcards
Modifying Exercise Intensity
Modifying Exercise Intensity
Signup and view all the flashcards
What is Muscle Setting?
What is Muscle Setting?
Signup and view all the flashcards
What is the Subacute Stage of Inflammation?
What is the Subacute Stage of Inflammation?
Signup and view all the flashcards
What happens during Fibroblastic activity in the Subacute Stage?
What happens during Fibroblastic activity in the Subacute Stage?
Signup and view all the flashcards
What is the typical pain experience during the Subacute Stage?
What is the typical pain experience during the Subacute Stage?
Signup and view all the flashcards
What is Scar Shrinkage in the Subacute Stage?
What is Scar Shrinkage in the Subacute Stage?
Signup and view all the flashcards
What is Resistance Exercise and how is it used in the Subacute Stage?
What is Resistance Exercise and how is it used in the Subacute Stage?
Signup and view all the flashcards
What are Functional Activities in the Subacute Stage?
What are Functional Activities in the Subacute Stage?
Signup and view all the flashcards
What is Immature Connective Tissue in the Subacute Stage?
What is Immature Connective Tissue in the Subacute Stage?
Signup and view all the flashcards
Inflammation Phase of Healing
Inflammation Phase of Healing
Signup and view all the flashcards
Repair Phase of Healing
Repair Phase of Healing
Signup and view all the flashcards
Muscle Function Restoration
Muscle Function Restoration
Signup and view all the flashcards
Muscular Endurance Exercises
Muscular Endurance Exercises
Signup and view all the flashcards
Improving Flexibility
Improving Flexibility
Signup and view all the flashcards
Returning to Activities
Returning to Activities
Signup and view all the flashcards
Chronic Phase of Healing
Chronic Phase of Healing
Signup and view all the flashcards
Tissue Maturation in Chronic Phase
Tissue Maturation in Chronic Phase
Signup and view all the flashcards
Scar tissue remodeling: What factors influence it?
Scar tissue remodeling: What factors influence it?
Signup and view all the flashcards
Cumulative Trauma
Cumulative Trauma
Signup and view all the flashcards
Scar tissue remodeling: Limit?
Scar tissue remodeling: Limit?
Signup and view all the flashcards
Cumulative Trauma: Structural Weakening
Cumulative Trauma: Structural Weakening
Signup and view all the flashcards
Scar tissue remodeling: Unresponsive, what to do?
Scar tissue remodeling: Unresponsive, what to do?
Signup and view all the flashcards
Cumulative Trauma: Reinjury of an Old Scar
Cumulative Trauma: Reinjury of an Old Scar
Signup and view all the flashcards
Cumulative Trauma: Contributing Factors
Cumulative Trauma: Contributing Factors
Signup and view all the flashcards
Chronic phase of healing: Patient education?
Chronic phase of healing: Patient education?
Signup and view all the flashcards
Chronic Inflammation: Acute Stage
Chronic Inflammation: Acute Stage
Signup and view all the flashcards
Chronic phase of healing: Exercise progression focus?
Chronic phase of healing: Exercise progression focus?
Signup and view all the flashcards
Chronic Inflammation: Subacute and Chronic Stages
Chronic Inflammation: Subacute and Chronic Stages
Signup and view all the flashcards
Chronic phase of healing: Stretching progression?
Chronic phase of healing: Stretching progression?
Signup and view all the flashcards
Chronic phase of healing: Strength exercise progression?
Chronic phase of healing: Strength exercise progression?
Signup and view all the flashcards
Work-conditioning and Work-hardening Programs
Work-conditioning and Work-hardening Programs
Signup and view all the flashcards
Muscle Guarding
Muscle Guarding
Signup and view all the flashcards
Chronic phase of healing: Return to high-demand activities?
Chronic phase of healing: Return to high-demand activities?
Signup and view all the flashcards
Study Notes
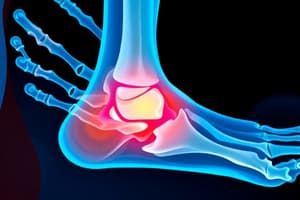
Chapter 10: Soft Tissue Injury, Repair, and Management
- Examination process is crucial to determine the stage of recovery (acute, subacute, or chronic) of involved tissues.
- This helps determine the appropriate type and intensity of exercises to facilitate healing without interfering with recovery.
- Preventing further problems and maximizing return of function are key goals.
Musculoskeletal Disorders and Tissue Response to Injury
- Soft Tissue Lesions:
- Strain: Overstretching, overexertion, or overuse of soft tissue (muscle/tendon).
- Sprain: Overstretching, overexertion, or overuse of soft tissue (ligament).
- Dislocation: Displacement of a part (usually bony partners in a joint).
- Subluxation: Incomplete or partial dislocation of bony partners in a joint.
Muscle Tendon Rupture or Tear
- Partial Tear: Pain during muscle stretches or contractions.
- Complete Tear: Muscle does not pull against the injury; stretching or contraction does not cause pain.
- Tendinopathy: Tendon injury affected by mechanical loading.
- Tenosynovitis: Inflammation of the synovial membrane covering a tendon.
- Tendinitis: Inflammation of a tendon.
- Tendinosis: Degeneration of a tendon due to repetitive microtrauma.
- Synovitis: Inflammation of a synovial membrane (joint or tendon sheath).
Musculoskeletal Disorders and Tissue Response to Injury
- Hemarthrosis: Bleeding into a joint.
- Ganglion: Ballooning of the wall of a joint capsule or sheath.
- Bursitis: Inflammation of a bursa.
- Contusion: Bruising from a direct blow, resulting in capillary rupture, bleeding, edema, and an inflammatory response.
- Overuse syndromes, cumulative trauma disorders, repetitive strain injuries: Conditions involving repetitive stress and strain on muscles and tendons.
Musculoskeletal Disorders and Tissue Response to Injury
- Primary pathology: Determining the primary pathology can be difficult, especially when tissue healing has limitations or secondary losses of function due to trauma or pathology.
- Dysfunction: Loss of normal function in a tissue or region.
- Joint Dysfunction: Mechanical loss of normal joint play in synovial joints.
- Contracture: Adaptive shortening of skin, fascia, muscle, or joint capsule preventing normal mobility or flexibility of a structure.
- Adhesions: Abnormal adherence of collagen fibers to surrounding structures.
Musculoskeletal Disorders and Tissue Response to Injury
- Reflex Muscle Guarding: Prolonged contraction of a muscle in response to painful stimuli.
- Intrinsic Muscle Spasm: Prolonged muscle contraction due to local circulatory and metabolic changes.
- Muscle Weakness: Decrease in the strength of muscle contractions.
- Myofascial Compartment Syndrome: Increased pressure in a closed, non-expanding myofascial compartment compromising blood vessels, muscles, and nerves.
Severity of Tissue Injury
- Grade I (first-degree): Mild pain within 24 hours of injury, mild swelling and tenderness, pain when stressed.
- Grade II (second-degree): Moderate pain requiring activity cessation, significant increase in pain with stress and palpation, some laxity.
- Grade III (third-degree): Complete or near-complete tear or avulsion of tissue, usually painless with palpation revealing a defect.
Grades of Sprain and Strain
- Grade I: Stretching, small tears.
- Grade II: Larger, but incomplete tear.
- Grade III: Complete tear.
Cardinal Signs of Inflammation
- Redness: Caused by dilation of arterioles/increased blood flow.
- Heat: Increased chemical activity and increased blood flow to the skin surface.
- Swelling: Caused by accumulation of blood and damaged tissue cells.
- Pain: Direct injury to nerve fibers, pressure of hematoma on nerve endings, chemical irritants (bradykinin, histamine, prostaglandin).
- Loss of Function: Increased pain/swelling.
Stages of Inflammation and Repair
- Acute Stage: The first phase of healing (4-6 days). Characterized by swelling, redness, heat, pain at rest, and loss of function. Painful range of motion and muscle guarding.
- Tissue responses: Early phases include vascular changes, cellular exudation, edema formation, and phagocytosis.
- Acute Phase Management Guidelines: Focus on maximum protection to help heal tissue through POLICE guidelines.
- Subacute Stage: The second phase of healing (10-17 days). Signs of inflammation decrease and eventually disappear. Pain may occur with ROM and when tissues are stressed.
- Subacute Tissue Responses: Fibroblast activity, collagen formation, and granulation tissue development increase. Myofibroblastic activity begins around day 5, and scar shrinkage starts.
- Subacute Phase Management Guidelines: Initial and progressive non-destructive exercise and activities and patient education.
- Chronic Stage: The third phase of healing (6 months-1 year). No inflammation is present. Pain may be present when testing tight structures and may be limited by contractures, adhesions, weakness etc.
Davis Law
- Ligaments and soft tissues, when under persistent tension, will elongate by producing new material.
- Conversely, soft tissues that aren't under tension will gradually shorten.
Wolff's Law of Bone
- Bone growth and remodeling respond to the forces acting on it.
- After an injury, stresses in specific directions help bone remodel to a healthy state.
Specific Interventions and Dosages for the Acute Phase
- Passive ROM: Used to maintain mobility within pain limits.
- Low-Dosage Joint Mobilization Techniques: Gentle isometric muscle contractions at low intensity to prevent pain or compression.
- Massage: Gently applied to injured tissues to move fluid and prevent adhesions.
Stages of Inflammation and Repair
- **Range of Motion (ROM):** Active or passive movements to maintain joint mobility, guided by the affected area.
- **Resistance Exercises:** Should be applied to muscles not directly related to injuries.
- **Functional Activities:** Use of supportive devices as needed, based on injury area and activities.
Specific Interventions and Dosages for the Subacute Phase
- Important to initiate and progress non-destructive exercises that are within the tolerance of healing tissues. Key to initiating and progressing non-destructive exercises and activities.
- Implement patient education on expected symptoms and consistent home exercise programs
- Monitoring pain levels and managing inflammation are key.
Multiple-angle, Submaximal Isometric Exercises
- Shortened, relaxed position to avoid pulling the new scar.
- Contractions kept below the perception of pain.
- Active range of motion exercises with light resistance to reinforce proper joint mechanics.
Muscular Endurance Exercises
- Begin with active range of motion (ROM).
- Progress to low intensity, high repetition exercises with light resistance.
- Implement protected weight bearing for exercises to reinforce appropriate muscle contractions and to promote development of control.
- Warm tissues, using relaxation and stretching techniques if needed, and promote new range of motion using massage to create a functional range of motion.
Initiation and Progression of Stretching
- Avoid complete or continuous immobilization.
- Gentle, but appropriate stretching is essential to maintain tissue flexibility.
- Exercise and activities should not cause pain or further injure affected areas.
Chronic Stage: Maturation and Remodeling
- The third phase of healing (6 months-1 year), characterized by no signs of inflammation, and potential for contractures or adhesions.
- Limited range of motion and muscle weakness or endurance may be present along with potential for pain to be felt when testing tight structures at the available range.
Tissue response in the Chronic Phase
- Collagen fibers become thicker and reorient in response to stresses on the connective tissue, and scar tissue development.
- Remodeling takes time depending on the size and location of the injury, along with the amount of tissue damage.
- Adaptive lengthening is supported by surgical interventions as needed.
Specific Interventions and Dosages for the Chronic Phase
- Provide patient education on biomechanically safe progressions of resistance and self-stretching.
- Re-evaluate patient progress to adapt and modify interventions as needed.
Progression of Stretching and Exercises
- Gradually increase the intensity and duration of stretching, avoiding increased pain, which typically lasts only 24 hrs after training.
- Progress strengthening exercises to better simulate muscle demands as is needed for sport specific activities
- Implement activities that mirror work and daily life activities.
Cumulative Trauma: Chronic Recurring Pain
- Repetitive stress exceeding the body's ability to repair tissue leads to chronic inflammation.
- Overuse, cumulative trauma, repetitive strain are common causes, potentially originating from injuries that have not fully healed or injuries to old scar tissue.
- Contributing factors include muscular imbalance, overuse, structural weaknesses or problems etc.
Chronic Pain Disorder (Chronic Pain Syndrome)
- A chronic condition lasting >6 months without a clear cause, leading to limitations in activity and function.
- Important to educate patients; emphasizing they are not causing continued injury, and that movement and activity may be beneficial.
- Use time-contingent approaches to physical activity and exercise, and focusing on non-destructive exercises.
Ankle Mobility & Strengthening Exercises
- A progression of exercises, from easiest to hardest, for ankle mobility and strengthening.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.