Podcast
Questions and Answers
Which structure has the highest permeability for ion absorption?
Which structure has the highest permeability for ion absorption?
- Colon
- Proximal large intestine
- Jejunum (correct)
- Ileum
What is the role of Intrinsic Factor in the absorption of Vitamin B12?
What is the role of Intrinsic Factor in the absorption of Vitamin B12?
- It releases calcium from food.
- It facilitates magnesium absorption.
- It binds to Vitamin B12 for absorption in the ileum. (correct)
- It transports water across intestinal cells.
Which ion's absorption occurs predominantly through the paracellular pathway in the small intestine?
Which ion's absorption occurs predominantly through the paracellular pathway in the small intestine?
- Sodium (Na+)
- Potassium (K+) (correct)
- Calcium (Ca++)
- Magnesium (Mg++)
Which factor is essential for the conversion of ferric iron to ferrous iron for absorption?
Which factor is essential for the conversion of ferric iron to ferrous iron for absorption?
What primarily stimulates the absorption of calcium in the small intestine?
What primarily stimulates the absorption of calcium in the small intestine?
In which phase of energy metabolism does insulin get released?
In which phase of energy metabolism does insulin get released?
What is the main function of Brunner's glands in the small intestine?
What is the main function of Brunner's glands in the small intestine?
Which cell type within the small intestinal crypts is primarily responsible for the secretion of antimicrobial enzymes?
Which cell type within the small intestinal crypts is primarily responsible for the secretion of antimicrobial enzymes?
What component of the immune system is particularly important in the intestinal surveillance within the small intestine?
What component of the immune system is particularly important in the intestinal surveillance within the small intestine?
What is the primary role of absorptive cells (enterocytes) in the small intestine?
What is the primary role of absorptive cells (enterocytes) in the small intestine?
Which of the following statements about the composition of bile is true?
Which of the following statements about the composition of bile is true?
What distinguishes phase I and phase II reactions in biotransformation?
What distinguishes phase I and phase II reactions in biotransformation?
Which of the following best describes the role of enteroendocrine cells in the small intestine?
Which of the following best describes the role of enteroendocrine cells in the small intestine?
Which structure contributes to the large surface area of the small intestine?
Which structure contributes to the large surface area of the small intestine?
Which aspect of the regeneration of the intestinal epithelium is accurate?
Which aspect of the regeneration of the intestinal epithelium is accurate?
Which statement accurately describes the liver's role in carbohydrate metabolism?
Which statement accurately describes the liver's role in carbohydrate metabolism?
Which of the following plasma proteins is primarily synthesized by the liver?
Which of the following plasma proteins is primarily synthesized by the liver?
What is the primary function of cytochrome P450 in the liver?
What is the primary function of cytochrome P450 in the liver?
Phase II of drug metabolism mainly involves what type of chemical reaction?
Phase II of drug metabolism mainly involves what type of chemical reaction?
Which statement is true regarding bile acids and their synthesis?
Which statement is true regarding bile acids and their synthesis?
What consequences can arise due to a lack of certain enzymes in cats during drug metabolism?
What consequences can arise due to a lack of certain enzymes in cats during drug metabolism?
How do bile salts influence cholesterol metabolism?
How do bile salts influence cholesterol metabolism?
Which of the following is not a typical outcome of phase I drug metabolism?
Which of the following is not a typical outcome of phase I drug metabolism?
What is the primary role of bile in digestion?
What is the primary role of bile in digestion?
Which factor can significantly impact drug metabolism variations among species?
Which factor can significantly impact drug metabolism variations among species?
What is the primary role of bile acids in the small intestine?
What is the primary role of bile acids in the small intestine?
Which of the following statements correctly describes the function of the gallbladder?
Which of the following statements correctly describes the function of the gallbladder?
What initiates pancreatic secretion of digestive enzymes?
What initiates pancreatic secretion of digestive enzymes?
Which enzyme is responsible for the initial breakdown of carbohydrates in the mouth?
Which enzyme is responsible for the initial breakdown of carbohydrates in the mouth?
What occurs during the process of emulsification in the duodenum?
What occurs during the process of emulsification in the duodenum?
What happens to short-chain fatty acids during lipid absorption?
What happens to short-chain fatty acids during lipid absorption?
What is the clinical manifestation of pancreatic insufficiency?
What is the clinical manifestation of pancreatic insufficiency?
What occurs to triacylglycerols inside enterocytes after absorption?
What occurs to triacylglycerols inside enterocytes after absorption?
Which factor influences the secretion of secretin in the digestive process?
Which factor influences the secretion of secretin in the digestive process?
Which of the following describes the role of chylomicrons in the body?
Which of the following describes the role of chylomicrons in the body?
What primarily influences the length of the villi in the small intestine?
What primarily influences the length of the villi in the small intestine?
Which cells migrate downward into the crypts of the small intestine?
Which cells migrate downward into the crypts of the small intestine?
What is the primary mechanism through which water is secreted in the intestines?
What is the primary mechanism through which water is secreted in the intestines?
How does most water reabsorption occur in the small intestine?
How does most water reabsorption occur in the small intestine?
Which statement best describes the structure of the large intestine's mucosa?
Which statement best describes the structure of the large intestine's mucosa?
Where do absorbed nutrients enter after moving through the interstitial space?
Where do absorbed nutrients enter after moving through the interstitial space?
Which components are included in the portal triad found in the liver lobule?
Which components are included in the portal triad found in the liver lobule?
What role do hepatocytes play within the liver lobule structure?
What role do hepatocytes play within the liver lobule structure?
What occurs to venous blood from the gastrointestinal tract before it returns to the heart?
What occurs to venous blood from the gastrointestinal tract before it returns to the heart?
What function does the large intestine serve in relation to vitamins?
What function does the large intestine serve in relation to vitamins?
Flashcards
Large Intestine Structure
Large Intestine Structure
Single layer of cylindrical epithelium, no villi.
Large Intestine Function
Large Intestine Function
Minimal water absorption (14%), vitamin absorption, mucus secretion.
Small Intestine Surface Area
Small Intestine Surface Area
Large surface area for nutrient absorption.
Plicae Circulares
Plicae Circulares
Signup and view all the flashcards
Villi
Villi
Signup and view all the flashcards
Microvilli
Microvilli
Signup and view all the flashcards
Crypts of Lieberkuhn
Crypts of Lieberkuhn
Signup and view all the flashcards
Paneth Cells
Paneth Cells
Signup and view all the flashcards
Enterocytes
Enterocytes
Signup and view all the flashcards
Goblet Cells
Goblet Cells
Signup and view all the flashcards
Brunner's Glands
Brunner's Glands
Signup and view all the flashcards
Peyer's Patches
Peyer's Patches
Signup and view all the flashcards
Enteroendocrine Cells
Enteroendocrine Cells
Signup and view all the flashcards
Liver Lobule
Liver Lobule
Signup and view all the flashcards
Hepatocytes
Hepatocytes
Signup and view all the flashcards
Portal Triad
Portal Triad
Signup and view all the flashcards
Bile Canaliculi
Bile Canaliculi
Signup and view all the flashcards
Exocrine Pancreas
Exocrine Pancreas
Signup and view all the flashcards
Pancreatic Juice
Pancreatic Juice
Signup and view all the flashcards
Secretin
Secretin
Signup and view all the flashcards
CCK
CCK
Signup and view all the flashcards
Carbohydrates
Carbohydrates
Signup and view all the flashcards
Protein Digestion
Protein Digestion
Signup and view all the flashcards
Lipid Digestion
Lipid Digestion
Signup and view all the flashcards
Chylomicrons
Chylomicrons
Signup and view all the flashcards
Study Notes
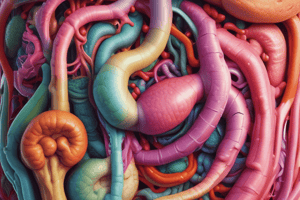
Small Intestine
- Large Surface Area: The small intestine has a large surface area to allow for reabsorption of nutrients.
- Three Levels of Surface Convolutions:
- Plicae Circulares: Spiral or circular folds lined by villi and microvilli.
- Villi: Finger-like epithelial projections.
- Microvilli: Small projections on the surface of villi.
- Structure of Small Intestine:
- Crypts of Lieberkuhn: Gland-like structures found at the base of villi.
- Crypts Cell Types:
- Paneth cells: Secrete antimicrobial enzymes and peptides.
- Endocrine cells: Produce hormones.
- Stem cells: Responsible for regeneration of intestinal epithelium.
- Goblet cells: Secrete mucus.
- Cell Types of Small Intestine:
- Absorptive cells (Enterocytes): Absorb nutrients.
- Secrete digestive enzymes, water, chloride ions (Cl-), and bicarbonate ions (HCO3-).
- Goblet cells: Secrete mucus.
- Enteroendocrine cells: Produce hormones like CCK, secretin, and GIP.
- Paneth cells: Secrete antimicrobial enzymes and peptides.
- Absorptive cells (Enterocytes): Absorb nutrients.
- Brunner's Glands:
- Located in the submucosa.
- Tubuloalveolar glands that produce mucus.
- Secrete glycoproteins and bicarbonate ions.
- Secretion has a pH of 8.1-9.3.
- Function: Protect small intestine mucosa by neutralizing acidic chyme from the stomach.
- Small Intestine Immune System:
- Peyer's Patches: Important in immune surveillance of the intestinal lumen.
- Facilitate the generation of immune responses within the mucosa.
- Peyer's Patches: Important in immune surveillance of the intestinal lumen.
- Cell Replacement in Small Intestine:
- Occurs within the intestinal crypts.
- Enterocytes divide and replicate.
- Crypt cells are among the most rapidly regenerating cells in the body.
- Enterocyte turnover time: 4 to 7 days.
- As cells multiply, they migrate upward along the villi (except Paneth cells).
- The length of villi is determined by the balance between cell loss at the tips and cell replacement.
- Cells of the Crypt and Regeneration:
- Progenitor cells differentiate into absorptive enterocytes, goblet cells, enteroendocrine cells, and Paneth cells.
- Water Absorption in Small Intestine:
- All water secretion in the intestine is mediated by osmosis.
- Food entering the intestine may be hyperosmotic, especially after digestion.
- Water moves via the paracellular pathway, following the movement of solutes.
- Most water reabsorption occurs in the small intestine due to:
- Larger solute reabsorption.
- Larger surface area (villi & microvilli).
- Larger openings in tight junctions.
- Extensive capillary network in the villi.
Large Intestine
- Structure:
- One layer of cylindrical epithelium.
- Crypts are present, but villi are absent.
- Functions:
- Minimal water absorption (about 14%).
- Vitamin absorption.
- Goblet cells produce mucus in small volumes, which is isotonic to plasma.
- Microbial metabolism is particularly significant in horses and rabbits.
Liver
- Liver Lobule:
- Hepatocytes: Liver cells arranged in a hexagonal pattern.
- Central vein: Located at the center of the hexagonal structure.
- Portal triad: Found at the vertices of the hexagon, containing:
- Portal venule.
- Arteriole of hepatic artery.
- Bile duct.
- Sinusoids: Low-pressure vascular channels that receive blood from the hepatic artery and portal vein.
- Bile canaliculi: Tiny tissue spaces between hepatocytes that form an intralobular network of channels.
- Drain bile produced by hepatocytes.
- Liver Functions:
- Carbohydrate metabolism: Gluconeogenesis, glycolysis.
- Amino acid and protein metabolism: Synthesis of plasma proteins.
- Lipid metabolism: Fatty acids oxidation, ketone bodies synthesis.
- Storage: Glycogen, lipids, vitamins, copper, iron.
- Synthesis and secretion of bile acids.
- Biotransformation of drugs, xenobiotics, and metabolic byproducts.
- Synthesis of hormones and mediators.
- Synthesis of components of the immune system
- Synthesis of Plasma Proteins:
- The liver produces most of the body's circulating plasma proteins, including:
- Albumins.
- Lipoproteins (VLDLs, LDLs, HDLs).
- Glycoproteins (haptoglobin, transferrin).
- Prothrombin and fibrinogen.
- Nonimmune alpha- and beta-globulins.
- The liver produces most of the body's circulating plasma proteins, including:
- Synthesis of Hormones by the Liver:
- Angiotensinogen: A prohormone.
- Thrombopoietin: A hormone (growth factor).
- Insulin-like growth factors (IGF1 and IGF2).
- Hepcidin: A small peptide hormone involved in iron homeostasis.
Biotransformation
- Definition: A group of reactions that convert toxic molecules into less toxic, less active, and water-soluble forms.
- Essential for drug metabolism, termination of drug action, and elimination.
- Cytochrome P450: Microsomal enzymes primarily located in the liver.
- Drug metabolism increases polarity, making drugs and their metabolites more water-soluble.
- Phase I: Oxidation reactions (hydroxylation, carboxylation).
- Phase II: Conjugation reactions (glucuronic acid, glycine, taurine).
Bile Acid Production
- Bile: Produced by hepatocytes, modified by gallbladder epithelial cells.
- Gallbladder: Stores and concentrates bile by resorption of electrolytes and water.
- Bile acids are synthesized from cholesterol.
- Bile salts are bile acids conjugated with amino acids (glycine, taurine).
- Bile salts inhibit cholesterol 7-alpha-hydroxylase, reducing the synthesis of bile acids.
- Bile acids are amphipathic molecules and the most important components of bile.
- Secretion:
- Secreted into bile canaliculi.
- Canaliculi merge into larger canals and ultimately the common bile duct.
- The sphincter of Oddi regulates bile flow into the duodenum.
- Enterohepatic Circulation: Continous recycling of bile acids between the liver, small intestine, and gallbladder.
Exocrine Pancreas
- Function: Secrete digestive enzymes and bicarbonate ions.
- Secretion:
- Pancreatic Juice: Containing digestive enzymes and bicarbonate ions.
- Zymogens: Inactive forms of digestive enzymes.
- Regulation of Pancreatic Secretion:
- Cephalic Phase: Stimulated by sight, smell, or thought of food.
- Gastric Phase: Stimulated by distention of the stomach.
- Intestinal Phase:
- ↓pH: Stimulates secretion of secretin.
- ↑ amino acids (AA), free fatty acids (FA): Stimulates secretion of CCK.
- Effects of Regulators:
- Secretin: Stimulates production of bicarbonate-rich pancreatic juice.
- Ach (acetylcholine) and CCK: Stimulate secretion of enzyme-rich and chloride-rich fluid.
- Pancreatic Enzymes: Released into acini via exocytosis.
- Pancreatic Insufficiency:
- Insufficient production of digestive enzymes by the exocrine pancreas.
- Leads to reduced digestion.
- Clinical signs: Greasy stools (steatorrhea), polyphagia, rapid weight loss.
- Pancreatitis:
- Inflammation of the pancreas.
- Commonly seen in older, obese dogs.
- Risk factors: High-fat diet, human food, garbage.
- Pathophysiology: Acini are destroyed and replaced by connective tissue due to auto-digestion.
Carbohydrates
- Functions:
- Energy source.
- Storage form of energy.
- Cell membrane component.
- Structural component.
- Monosaccharides: Simple sugars with the general formula (CH2O)n.
- Disaccharides: Two monosaccharides linked by glycosidic bonds.
- Oligosaccharides: 3-10 monosaccharides.
- Polysaccharides: More than 10 monosaccharides.
- Digestion:
- Begins in the mouth (salivary amylase, in species that produce it).
- Continues in the small intestine with pancreatic enzymes and intestinal mucosal enzymes.
- Absorption:
- Occurs in the duodenum and upper jejunum.
- Mediated by:
- Sodium-dependent glucose transporter 1 (SGLT1) at the apical membrane.
- Glucose transporters (GLUT5 and GLUT2) at both the apical and basolateral membranes.
Protein Digestion
- Begins in the stomach:
- Pepsin partially hydrolyzes proteins (12-15%).
- Denaturation of proteins.
- Continues in the small intestine:
- Pancreatic enzymes further digest polypeptides and oligopeptides.
- Brush border peptidases break down oligopeptides into tri- and dipeptides.
- Amino acids are transported into the cell and eventually to the liver via the portal vein.
Lipids
- Functions:
- Prostaglandins.
- Steroid hormones.
- Phospholipids.
- Platelet-activating factor (PAF).
- Sphingomyelin.
- Dietary Lipids:
- Cholesterol esters, phospholipids, triglycerides.
- Short-chain and medium-chain fatty acids (<12 carbons).
- Long-chain fatty acids (>12 carbons).
- Digestion and Utilization:
- Emulsification:
- Reduces droplet size.
- Increases surface area of hydrophobic lipid droplets.
- Bile acids: Emulsify fat droplets.
- Pancreatic lipases: Hydrolyze triglycerides into monoglycerides and free fatty acids (FFA) in the duodenum.
- Emulsification:
- Mixed Micelles:
- Formed by monoglycerides, FFA, cholesterol, and fat-soluble vitamins.
- Carry lipids to the brush border membrane for absorption.
- Absorption:
- Long-chain fatty acids (LCFA) are re-esterified into triglycerides in the endoplasmic reticulum.
- Chylomicrons (CMs): Triglyceride-rich lipoproteins that transport lipids, primarily through lymphatic vessels.
- Chylomicrons enter the bloodstream via the thoracic duct, bypassing the liver.
Intestinal Absorption of Ions and Water
- Sodium (Na+) Transport:
- Very efficient and drives most transport processes.
- Potassium (K+) and Chloride (Cl-) Absorption:
- Primarily occurs in the small intestine through the paracellular pathway.
- Water Absorption:
- 85% in the small intestine (duodenum and jejunum: 55%; ileum: 30%).
- 14% in the large intestine.
- Factors Influencing Absorption:
- Increased surface area.
- Mucosa uptake mechanisms.
- High blood perfusion.
- Permeability.
- Pore size and water permeability of tight junctions vary along the intestine.
Intestinal Absorption of Essential Nutrients
- Calcium (Ca++) Absorption:
- Parathyroid hormone (PTH): Stimulates vitamin D production in the kidney.
- Calcitriol (active vitamin D): Increases calcium absorption in the small intestine by:
- Increasing apical Ca++ channels.
- Increasing calbindin synthesis.
- Increasing Ca++ ATPase activity.
- Magnesium (Mg++) Absorption:
- Absorbed through Mg++ channels and paracellularly.
- Phosphate (PO4--) Absorption:
- Absorbed through the Na+/Phosphate symporter.
- Vitamin B12 Absorption:
- Haptocorrin (HC): Glycoprotein produced by salivary glands, binds to vitamin B12 in the stomach.
- Pancreatic enzymes (trypsin): Degrade HC in the duodenum.
- Intrinsic factor (IF): Produced by parietal cells in the stomach, binds to free vitamin B12.
- IF/vitamin B12 complex: Absorbed in the ileum.
- Transcobalamin: Transports vitamin B12 in the plasma.
- Iron Absorption:
- Primarily occurs in the duodenum and proximal jejunum.
- Iron must be in the ferrous (Fe2+) state for absorption.
- The low pH in the proximal duodenum facilitates the conversion of ferric (Fe3+) to ferrous iron.
- Once in the bloodstream, iron binds to transferrin.
Iron Transport
- Transferrin is a glycoprotein found in blood, which binds to iron and transports it throughout the body.
- Absorption of vitamins occurs mainly in the small intestine for water-soluble vitamins.
- Water-soluble vitamins are absorbed from the small intestine.
- Vitamins produced by microbes in the large intestine are absorbed in the large intestine.
- Specific carrier-mediated transport systems are responsible for the absorption of vitamins.
- These transporters can either be secondary active transporters relying on the Na-K-ATPase or independent of sodium.
- Fat-soluble vitamins (A, D, E, K) are absorbed through mixed micelles and enter the enterocyte by diffusion.
Catabolic Pathways
- Generate energy (ATP, NADH) through the breakdown of energy-rich molecules.
Anabolic Pathways
- Combine small molecules (e.g. amino acids) to form complex molecules (e.g. proteins).
- Require energy (ATP→ADP) and often chemical reductions (NADH).
Phases of Energy Metabolism
- Energy metabolism can be divided into three phases:
Absorptive Phase
- During active digestion and absorption of nutrients from the gut. - Insulin is released. - Glucose is taken up by the liver and converted to glycogen and fatty acids. - Fatty acids are sent out of the liver as VLDL to adipose tissue or muscle. - Amino acids are used for protein synthesis or deaminated for gluconeogenesis.Post-Absorptive Phase
- Between meals when nutrients are mobilized from storage pools to tissues. - Glucagon is released. - Glycogenolysis and gluconeogenesis are stimulated - Amino acids are mobilized from muscle.Prolonged Energy Deficiency or Food Deprivation
- Glucose and amino acids are conserved. - Fatty acids are mobilized in the form of non-esterified fatty acids (NEFAs). - Formation of ketone bodies in the liver (mitochondria).
Definitions
- Glycogen: The primary form of carbohydrate storage in the liver and muscle.
- Glycogenolysis: The breakdown of glycogen to glucose
- Gluconeogenesis: The generation of glucose.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.