Podcast
Questions and Answers
What is the primary role of skeletal muscle?
What is the primary role of skeletal muscle?
- Maintains blood flow
- Produces involuntary movements
- Controls heart rate
- Produces voluntary movements (correct)
Which type of muscle is not under voluntary control?
Which type of muscle is not under voluntary control?
- Both B and C (correct)
- Skeletal Muscle
- Cardiac Muscle
- Smooth Muscle
During muscle contraction, which filament interacts with myosin?
During muscle contraction, which filament interacts with myosin?
- Fascicles
- Tropomyosin
- Actin (correct)
- Calcium
What initiates the signal for muscle contraction?
What initiates the signal for muscle contraction?
What happens after calcium binds with troponin during muscle contraction?
What happens after calcium binds with troponin during muscle contraction?
How long does ATP typically fuel muscle activity before replenishment is needed?
How long does ATP typically fuel muscle activity before replenishment is needed?
What role do synergistic muscles play during movement?
What role do synergistic muscles play during movement?
What occurs during muscle relaxation?
What occurs during muscle relaxation?
What causes the deeper voices in males after puberty?
What causes the deeper voices in males after puberty?
Which of the following statements about laryngitis is true?
Which of the following statements about laryngitis is true?
What is the major factor contributing to emphysema?
What is the major factor contributing to emphysema?
What role does the diaphragm play during inhalation?
What role does the diaphragm play during inhalation?
How does smoking affect the respiratory tract?
How does smoking affect the respiratory tract?
What triggers asthma attacks?
What triggers asthma attacks?
What is the primary function of alveoli in the lungs?
What is the primary function of alveoli in the lungs?
Which of the following is NOT a role of the smooth muscle in the bronchioles?
Which of the following is NOT a role of the smooth muscle in the bronchioles?
Which part of the nervous system regulates the basic breathing pattern?
Which part of the nervous system regulates the basic breathing pattern?
What is a common symptom of pneumonia?
What is a common symptom of pneumonia?
What is the primary risk associated with Rh-negative women pregnant with an Rh-positive baby?
What is the primary risk associated with Rh-negative women pregnant with an Rh-positive baby?
Which form of anemia is characterized by the bone marrow's inability to produce enough red blood cells?
Which form of anemia is characterized by the bone marrow's inability to produce enough red blood cells?
What is the function of the pulmonary veins in the circulatory system?
What is the function of the pulmonary veins in the circulatory system?
How do veins maintain blood return against gravity?
How do veins maintain blood return against gravity?
What is the primary function of creatine phosphate in muscle energy?
What is the primary function of creatine phosphate in muscle energy?
Which condition occurs due to high blood pressure and can lead to serious cardiovascular issues?
Which condition occurs due to high blood pressure and can lead to serious cardiovascular issues?
What is the main function of baroreceptors in the body?
What is the main function of baroreceptors in the body?
What main characteristic distinguishes fast-twitch muscle fibers from slow-twitch fibers?
What main characteristic distinguishes fast-twitch muscle fibers from slow-twitch fibers?
Which of the following statements about blood functions is incorrect?
Which of the following statements about blood functions is incorrect?
How does exercise benefit cardiovascular health?
How does exercise benefit cardiovascular health?
Which heart chamber is primarily responsible for pumping blood to the entire body?
Which heart chamber is primarily responsible for pumping blood to the entire body?
What is the primary role of erythropoietin in the body?
What is the primary role of erythropoietin in the body?
How does hemoglobin release oxygen effectively in active tissues?
How does hemoglobin release oxygen effectively in active tissues?
What is the primary cause of carbon monoxide poisoning?
What is the primary cause of carbon monoxide poisoning?
Which of the following best describes anemia?
Which of the following best describes anemia?
What is a characteristic feature of smooth muscle cells?
What is a characteristic feature of smooth muscle cells?
What leads to muscle fatigue during intense activity?
What leads to muscle fatigue during intense activity?
What type of valve prevents backflow from the arteries to the ventricles in the heart?
What type of valve prevents backflow from the arteries to the ventricles in the heart?
What is a common characteristic of leukemia?
What is a common characteristic of leukemia?
What happens during platelet plug formation?
What happens during platelet plug formation?
What is one potential consequence of untreated hemophilia?
What is one potential consequence of untreated hemophilia?
Which is true about the lifespan of red blood cells (RBCs)?
Which is true about the lifespan of red blood cells (RBCs)?
Which of the following is a viral pathogen?
Which of the following is a viral pathogen?
What is one consequence of receiving incompatible blood types?
What is one consequence of receiving incompatible blood types?
What is the characteristic structure of red blood cells?
What is the characteristic structure of red blood cells?
What triggers the release of fibrin during coagulation?
What triggers the release of fibrin during coagulation?
How do aerobic respiration processes primarily differ from anaerobic processes?
How do aerobic respiration processes primarily differ from anaerobic processes?
What defines the Rh factor in blood typing?
What defines the Rh factor in blood typing?
Which of the following diseases is caused by a protist?
Which of the following diseases is caused by a protist?
What type of immunity involves the body recognizing specific pathogens it has encountered before?
What type of immunity involves the body recognizing specific pathogens it has encountered before?
Which type of white blood cells make up about two-thirds of the total white blood cell count and are crucial for fighting infections?
Which type of white blood cells make up about two-thirds of the total white blood cell count and are crucial for fighting infections?
What is the role of memory B cells in the immune system?
What is the role of memory B cells in the immune system?
Which of these is a characteristic of innate immunity?
Which of these is a characteristic of innate immunity?
What is the function of eosinophils in the immune response?
What is the function of eosinophils in the immune response?
Which organ filters infections from the blood and breaks down old red blood cells?
Which organ filters infections from the blood and breaks down old red blood cells?
What results from the action of complement proteins in immunity?
What results from the action of complement proteins in immunity?
What is a major consequence of high sustained fevers in the body?
What is a major consequence of high sustained fevers in the body?
Which of the following accurately describes passive immunization?
Which of the following accurately describes passive immunization?
Which structure prevents food from entering the trachea during swallowing?
Which structure prevents food from entering the trachea during swallowing?
How does the body obtain oxygen during respiration?
How does the body obtain oxygen during respiration?
What immune disorder occurs when the body attacks its own cells?
What immune disorder occurs when the body attacks its own cells?
What protects the skin from pathogens?
What protects the skin from pathogens?
Flashcards are hidden until you start studying
Study Notes
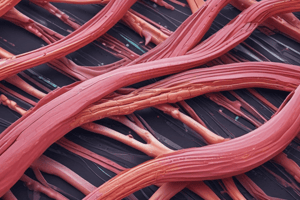
### Muscle Tissue Composition
- Muscle makes up 40% of body weight in males and 32% in females.
- There are three types of muscle:
- Skeletal Muscle: Produces movement and is generally under voluntary control.
- Cardiac Muscle: Found in the heart, responsible for pumping blood.
- Smooth Muscle: Involuntary control, found in organs like the digestive tract, blood vessels, bladder, and uterus.
- Muscles function by contracting, shortening the distance between bones, and then relaxing.
### Muscle Groups
- Synergistic Muscles: Different muscles work together for a movement, for example, turning your head.
- Antagonistic Muscles: Opposing muscles produce opposite motions. These muscle groups don't contract at the same time because of reciprocal innervation.
### Muscle Structure
- Muscle cells share the same origin and insertion.
- Fascicles: Bundles of cells surrounded by connective tissue that form tendons.
- Myofibrils: Bundles within each muscle cell that are composed of sarcomeres laid out end-to-end.
- Skeletal muscle cells are multinucleate, formed from fused cells.
- A muscle contains many fascicles, which contain many cells, which contain many myofibrils, which contain many sarcomeres laid out end-to-end.
Sarcomere
- The basic muscle contractile unit.
- Made up of thick (myosin) and thin (actin) filaments.
- Contraction: Cross-bridges are formed between myosin and actin, resulting in muscle contraction.
- Relaxation: Cross-bridges are broken, and the filaments slide back into place, leading to muscle relaxation.
### Sliding Filament Mechanism
- Sarcomeres shorten during muscle contraction.
- Z-Lines: Points where actin filaments are attached.
### Muscle Contraction Steps
- Signal for muscle contraction originates in the cerebral cortex.
- Neurons carry this message from the brain, down the spinal cord, to the muscles.
- Motor neurons release acetylcholine (a neurotransmitter), which binds to muscle cell receptors.
- This generates an electrical impulse in the muscle.
- The impulse causes the release of calcium ions from the sarcoplasmic reticulum into the cytoplasm.
- Calcium binds to troponin, causing tropomyosin to expose actin binding sites.
- Energized myosin heads create cross-bridges with actin, leading to muscle contraction.
### Muscle Relaxation
- Nervous stimulation stops, and calcium is pumped back into the sarcoplasmic reticulum.
- Tropomyosin covers the actin binding sites, and the sarcomere relaxes.
### Energy Sources for Muscle Activity
- ATP: The first energy source for muscle activity, lasting up to 10 seconds.
- Creatine Phosphate: Replenishes ATP for an additional 25 seconds.
- Stored Glycogen: Provides energy for 5-10 minutes.
- Aerobic Respiration: Provides energy for longer periods by using glucose, triglycerides, and proteins.
### Muscle Fatigue
- Muscles are unable to contract due to insufficient ATP supply and a buildup of lactic acid.
- Deep breaths and rest help break down lactic acid and replenish ATP levels.
### Motor Unit
- A single motor neuron stimulates multiple muscle cells.
- One motor neuron and the muscle cells it stimulates constitute a motor unit.
- Fine Control: Fewer muscle cells per neuron (e.g., eyes).
- Brute Strength: More muscle cells per neuron (e.g., legs).
### Skeletal Muscle Types
- Slow-Twitch Fibers: Contract slowly and are suited for endurance activities.
- Fast-Twitch Fibers: Contract quickly and are suited for short bursts of power.
- Muscles contain a mixture of both types of fibers, with varying proportions due to genetics and training.
### Exercise and Muscles
- Strength Training: Builds fast-twitch muscle fibers and increases glycogen and creatine phosphate stores.
- Endurance Training: Builds slow-twitch muscle fibers, increases blood vessel supply, mitochondria, and myoglobin.
### Comparison of Muscle Types
- Skeletal Muscle: Voluntary control, long, cylindrical, multinucleated cells.
- Cardiac Muscle: Involuntary control, short cells connected by gap junctions.
- Smooth Muscle: Involuntary control, small, spindle-shaped cells joined by gap junctions.
### Muscle Disorders
- Tetanus: A bacterial toxin causes constant muscle contraction.
- Duchenne Muscular Dystrophy: A genetic disease leading to muscle degeneration.
- Pulled Muscles: Muscle fibers tear from overstretching.
- Muscle Cramps: Uncontrolled muscle contraction due to factors like ATP depletion, dehydration, and ion imbalances.
- Anabolic Steroids: Mimic testosterone, increasing muscle mass but can cause side effects such as liver and kidney tumors, baldness, and infertility.
Functions of Blood
- Transportation: Blood transports various substances throughout the body.
- Homeostasis:
- Regulating Body Temperature: Heat in blood is transported near the skin's surface when we are hot.
- pH of Body Fluids: Blood contains a buffering system, including ion buffers and hemoglobin, that binds to excess hydrogen ions.
- Defense: Various white blood cells and antibodies defend against infections.
- Clotting: Platelets and fibrinogen proteins prevent excessive blood loss.
### Components of Blood
- Cellular Portion (45% of volume):
- Red Blood Cells (RBCs): Transport oxygen and some carbon dioxide.
- White Blood Cells (WBCs): Defend against viral, bacterial, protist, and animal invaders, as well as virus-infected cells and cancerous cells.
- Platelets: Critical for blood clotting.
- Plasma (55% of volume):
- Water: The primary constituent (90%) and biological solvent.
- Ions: pH buffers for cell function and volume regulation, essential for excitable cells like muscles and nerves.
- Hormones: Messages released by endocrine glands into the blood.
- Gases: Oxygen (small amounts) and carbon dioxide (majority) dissolved in plasma.
- Nutrients: Such as amino acids, glucose, and lipids. Lipids are bound to special globulin transport proteins because they do not dissolve in blood plasma.
- Wastes: Ammonia, urea, and uric acid, removed from the blood at the kidneys.
### Plasma Proteins
- Albumins: Produced by the liver to maintain osmotic balance between blood and extracellular fluid, helping to maintain fluid volume.
- Antibodies: Produced by WBCs, they bind to foreign substances like bacteria and viruses.
- Fibrinogen: Produced by the liver and converted to fibrin, forming a network for blood clotting.
### Red Blood Cells (RBCs)
- Structure: No nucleus, no organelles, and flattened disks which allow flexibility.
- Lifespan: RBCs live for 120 days on average.
- Old cells are broken down in the liver and spleen: Iron is recycled to the red bone marrow, amino acids are reused, and heme groups become part of bile.
### Control of RBC Production
- The hormone erythropoietin controls the production of RBCs.
### Homeostasis of Oxygen Carrying Capacity
- Kidney cells detect a decrease in oxygen levels and secrete erythropoietin to increase RBC production by stem cells in the red bone marrow.
- Increased oxygen levels lead to reduced erythropoietin secretion.
### Hemoglobin
- Each RBC contains 300 million hemoglobin molecules, each capable of carrying 1.2 billion oxygen molecules.
- Structure: Composed of four polypeptide chains (two alpha and two beta), each with a heme group containing iron that binds to oxygen. Each hemoglobin molecule binds to 4 oxygen molecules.
### Hemoglobin and Oxygen Binding
- Hemoglobin binds to oxygen: Higher pH (less acidic), high oxygen concentration, and lower temperature (like in the lungs).
- Hemoglobin releases oxygen: Lower pH (more acidic), low oxygen concentration, and higher temperatures (like in active tissues such as exercising muscles).
### Stopping Loss of Blood
- Vascular Spasm: Smooth muscle constricts blood vessels, reducing or stopping blood flow.
- Platelet Plug Formation: Platelets change shape, become stickier, and form a plug.
- Coagulation: Chemical signals convert soluble fibrinogen into insoluble fibrin, forming a clot with trapped RBCs and platelets.
### Blood Types and Antibodies
- Antigens: Proteins/glycoproteins in cell membranes.
- B Lymphocytes: Produce protein antibodies that bind to foreign antigens.
- Wrong blood type: Agglutination occurs, causing clumps of RBCs and antibodies to get stuck in small blood vessels. This damages organs due to lack of blood supply, potentially leading to death.
### Rh Factor
- Rh Antigen: If present, an individual is Rh positive; if absent, they are Rh negative.
- Rh-negative individuals: Can receive Rh-positive blood once, but antibodies are produced that will cause agglutination if Rh-positive blood is received a second time.
### Rh Factor and Pregnancy
- First Pregnancy: Rh-negative women pregnant with an Rh-positive baby are usually fine, but antibodies form in the mother.
- Second Pregnancy: These antibodies can cross the placenta, potentially causing hemolytic disease of the newborn (severe anemia, jaundice, and possibly death).
- Treatment: RhoGam is administered before the first birth to prevent the mother’s immune response.
### Blood Disorders
- Carbon Monoxide Poisoning: CO competes with oxygen, binding to hemoglobin and staying bound for a long time, preventing oxygen from binding.
- CO is produced by burning fuel (e.g., motor exhaust), wood, charcoal, and tobacco.
- Anemia: Reduction in oxygen-carrying capacity:
- Iron Deficiency: Low iron = not enough heme groups formed.
- Aplastic Anemia: Bone marrow does not produce enough RBCs.
- Hemorrhagic Anemia: Extreme blood loss.
- Sickle Cell Anemia: RBCs are sickle-shaped and destroyed early (genetic).
- Thalassemia: Insufficient alpha or beta protein chains of hemoglobin produced, reducing oxygen-carrying capacity.
- Leukemia: Cancer of WBCs, leading to uncontrolled WBC division. Crowds out normal WBCs and RBCs, interfering with organ function.
- Hemophilia: Uncontrolled bleeding due to insufficient platelets, liver diseases, or Vitamin K deficiency.
Circulation Overview
- Arteries: Carry blood away from the heart.
- Veins: Carry blood towards the heart.
- Capillaries: Where most exchange of gases, nutrients, and wastes takes place.
- Pulmonary Circulation: Blood flow between the heart and lungs.
- Systemic Circulation: Blood flow between the heart and the rest of the body.
- Coronary Arteries: Supply blood to the heart muscles.
- Cardiac Veins: Return blood from the heart muscles.
Blood Flow Through Blood Vessels
- Pathway: Heart → Aorta → Arteries → Arterioles → Capillaries → Venules → Veins → Heart.
- Pulmonary Arteries: Carry deoxygenated blood to the lungs.
- Pulmonary Veins: Carry oxygenated blood back to the heart.
Blood Vessels
- Arteries: Highest blood pressure; thick middle and outer layers. Elastic recoil helps move blood forward.
- Arterioles: Small arteries that regulate blood flow to capillaries.
- Capillaries: Where exchange of gases, nutrients, and wastes occurs. Made of a single layer of endothelial cells.
- Venules: Small veins that collect blood from capillaries.
- Veins: Low blood pressure, large lumen, and thinner walls. Stores a large amount of blood and contain one-way valves to prevent backflow.
### Capillaries
- Proteins and red blood cells remain in capillaries during exchange, while fluids are reabsorbed by osmotic pressure, driven by albumin plasma protein.
- Edema: Swelling due to low albumin levels - common in malnourished children.
- The lymphatic system returns excess fluid to the veins.
### Venules and Veins
- Blood is stored in veins, and 50-60% of all blood in the body is in veins.
- Blood pressure is low in veins, so they don't need thick walls.
Mechanisms for Blood Return
- Gravity: Helps return blood from veins above the heart.
- Skeletal Muscle Contractions: Help pump blood back towards the heart.
- Smooth Muscle Contraction in Vein Walls: Helps move blood forward.
- Pressure Changes During Breathing: Inhaling causes low pressure in the thorax and high pressure in the abdomen, which helps move blood back to the heart.
Heart Structure
- Chambers: Four chambers: two atria and two ventricles. The left ventricle is the most muscular as it pumps blood to the entire body.
- Valves:
- Atrioventricular Valves: Prevent backflow from ventricles to atria.
- Semilunar Valves: Prevent backflow from arteries to ventricles.
### Cardiac Cycle
- Blood flows due to pressure differences, and valves prevent backflow.
### Heart Sounds and Valves
- Lub-DUB: Heart sounds are due to valve closures.
- "Lub": Atrioventricular valves closing.
- "DUB": Semilunar valves closing.
- Heart Murmurs: Unusual heart sounds due to backflow through valves.
### Heart Contractions
- Sinoatrial (SA) Node: Cardiac pacemaker generates an electrical signal.
- Gap Junctions: Electrical impulses travel between cardiac cells.
- Atrioventricular (AV) Node: Receives impulses, and the AV bundle carries impulses to the ventricles.
### Controlling Heart Rate
- At Rest: The medulla oblongata dampens the SA node to slow the heart rate.
- During Stress or Exercise: The heart rate increases as the medulla stimulates the heart.
### Blood Pressure and Homeostasis
- Baroreceptors: Monitor blood pressure and send messages to the medulla.
- The medulla controls heart rate and arteriole width, affecting blood pressure.
- Increased heart rate + vasoconstriction = higher blood pressure.
- Decreased heart rate + vasodilation = lower blood pressure.
### Cardiovascular Disorders
- Hypertension: Blood pressure >140/90. High blood pressure damages arteries, causing arteriosclerosis and increasing heart attack and stroke risk.
- Atherosclerosis: Cholesterol plaques form, narrowing arteries.
- Embolism: Blood clot blocks a blood vessel, potentially leading to heart attacks or strokes.
- Angina Pectoris: Chest pain due to restricted blood flow to the heart.
- Heart Attack: Blockage of coronary arteries causes heart muscle death.
- Ventricle Fibrillation: Irregular heartbeats can cause sudden unconsciousness.
- Stroke: Blockage of blood flow to the brain or vessel rupture leads to permanent brain damage.
- Aneurysm: Weakening of arterial walls, potentially leading to fatal ruptures.
### Preventing Cardiovascular Disease
- Reduce salt and saturated fats in your diet.
- Exercise regularly to strengthen the heart and improve circulation.
- Avoid smoking and limit alcohol intake.
- Control stress and maintain a healthy weight.
### Exercise Benefits
- Lowers blood pressure and cholesterol.
- Increases red blood cell count and blood vessel supply to the heart.
- Strengthens the heart, reducing the need for it to work hard over time.
Examples of Pathogens
- Viral: Influenza, common cold, chickenpox, HIV/AIDS, COVID-19.
- Bacterial: Tuberculosis, salmonella, cholera, urinary tract infections, gonorrhea.
- Protist: Malaria, amoebic dysentery.
- Fungal: Athlete’s foot, yeast infection.
- Animal: Intestinal fluke, whipworm.
Whipworm
- Burrows into the tissue surrounding the large intestine.
- Can cause rectal bleeding, anemia, diarrhea, and dehydration.
Defenses Against Invaders
- Physical/Chemical Surface Barriers (1st Line of Defense): Prevent pathogens from entering the body.
- Nonspecific Defenses "Innate Immunity" (2nd Line): Attack pathogens that enter the body but do not recognize specific pathogens. Not important for long-term immunity.
- Specific Defenses "Adaptive Immunity" (3rd Line): Recognize specific pathogens previously encountered and responsible for long-term immunity.
### Physical/Chemical Barriers
- Skin: Multiple layers of tightly-packed cells provide a physical barrier to pathogens. Skin pH is 5-6, which is too acidic for many microorganisms.
- Resident Harmless Bacteria: Out-compete pathogens on the skin's surface.
### Other Physical/Chemical Barriers
- Tears, Saliva, Mucus: Contain lysozymes that kill bacteria.
- Earwax
- Digestive Acids
- Urination, Vomiting, Defecation
### Innate Immunity (Neutrophils)
- Neutrophils: 2/3 of WBCs are neutrophils. They leave capillaries, phagocytize bacteria, and digest them using lysosomes. Dead neutrophils contribute to pus.
### Innate Immunity (Macrophages)
- Monocyte WBCs: Become macrophages. They leave capillaries, engulf bacteria, and digest dead cells. Macrophages release cytokines, which trigger fevers.
### Fever
- Raising body temperature can create an unfavorable environment for bacteria and increase WBC activity.
- High sustained fevers can be dangerous due to protein denaturation.
### Innate Immunity (Eosinophils)
- Attack large invaders like parasites (e.g., worms) by surrounding them and releasing digestive enzymes.
### Innate Immunity (Natural Killer Cells)
- Natural Killer Cells: Recognize and kill infected or cancerous cells.
### Innate Immunity (Complement Proteins)
- Complement Proteins: Present in blood and tissue fluids. Complement proteins attach to pathogens, attract neutrophils and macrophages, and help phagocytize pathogens.
- Membrane Attack Complexes: Punch holes in bacterial cell membranes, leading to rupture.
### Innate Immunity (Inflammatory Response)
- Basophils and Mast Cells: Release histamines, causing inflammation.
- Signs of inflammation: Redness, warmth, swelling, and pain.
### Adaptive Immunity (Lymphocytes)
- B Cells: Produce antibodies that bind to foreign antigens.
- Cytotoxic T Cells: "Touch-kill" foreign cells or infected cells.
- Helper T Cells: Coordinate the immune response and stimulate cell division of B and T lymphocytes.
### Key Features of Adaptive Immunity
- Specificity: Targets specific antigens the body has been exposed to.
- Diversity: Over 1 billion B and T lymphocytes target different antigens.
- Memory: Memory B and T cells provide long-term immunity.
### B Cells and Antibodies
- Effector B Cells: Secrete antibodies into lymph and blood, binding to pathogens.
- Memory B Cells: Remain in the body for quick responses to future infections.
### T Cells
- Helper T Cells: Stimulate the division of B and cytotoxic T cells.
- Cytotoxic T Cells: Recognize and kill cells infected with specific antigens using perforin proteins.
### First Exposure to Pathogens
- Primary Immune Response: Slow and peaks at 10-12 days. Memory B and T cells are created.
### Second Exposure to Pathogens
- Secondary Immune Response: Rapid and results in greater antibody production.
### Why the Flu Recurs
- The flu virus mutates, leading to new antigens.
### Lymphatic System
- Lymphatic System: Transports bacteria and other pathogens to lymph nodes, where macrophages engulf them.
- Lymph Nodes: Also house B and T lymphocytes.
Lymphatic Organs
- Lymph Nodes: Contain macrophages and lymphocytes.
- Spleen: Filters infections in the blood and breaks down old RBCs.
- Thymus Gland: Matures T lymphocytes.
### Breastfeeding and Immunity
- Antibodies and immune cells are transferred through breast milk.
### Immunization (Vaccination)
- Exposure to dead or weakened pathogens results in the formation of memory B and T cells, providing immunity without sickness.
### Passive Immunization
- Injected antibodies fight infections but do not provide long-term immunity.
### Antibiotics
- Only effective against bacteria, not viruses
### Organ Donation
- Transplanted organs have foreign antigens that can trigger immune rejection.
### Allergies
- Harmless substances cause an immune response, leading to inflammation.
### Autoimmune Disorders
- The immune system mistakenly attacks the body's own cells.
- Multiple Sclerosis: Inflammation damages cells protecting neurons.
- Type 1 Diabetes: Immune cells destroy insulin-producing cells.
- Rheumatoid Arthritis: Inflamed joints due to autoimmune attacks on the synovial membrane.
### Functions of the Respiratory System
- Exchanging carbon dioxide and oxygen.
- Producing noises (language)
### The Path of Oxygen
- Oxygen inhaled through the mouth or nose → pharynx → trachea → bronchi → bronchioles → alveoli in lungs → diffuses into blood plasma in capillaries surrounding alveoli → binds with hemoglobin → transported in blood vessels → diffuses into blood plasma in capillaries of the body → diffuses into cells → diffuses to mitochondria for aerobic cellular respiration.
- Carbon dioxide moves in the opposite direction.
- Note: Gas exchange between the respiratory and circulatory systems occurs only at the alveoli.
Upper Respiratory Tract
- Passageway for respiration.
- Contains receptors for smell (important for taste).
- Catches foreign materials (dirt, bacteria) in mucus; cilia move it back to the pharynx to be coughed out or swallowed.
Upper Respiratory Tract
- Moistens and warms air: Mucus and blood vessels play a crucial role in preparing air for the lungs.
- Voice production: The upper respiratory tract acts as a resonating chamber for sound production
Lower Respiratory Tract
- Epiglottis: A flap of cartilage that covers the trachea during swallowing, preventing food from entering the airway.
- Glottis: The opening to the trachea, responsible for sound production. The glottis is open when not talking and mostly closed during speech.
- Larynx: The "voice box." It transports air to and from the lungs and allows for speech production by vibrating vocal cords. Men have deeper voices due to larger larynxes and longer vocal cords after puberty. Laryngitis is inflammation of the larynx that affects vocal cord vibration.
- Trachea (windpipe): A rigid tube lined with mucus-secreting cells and cilia, helping to clean and filter the air. Smoking damages these cells, leading to "smoker's cough" and increased susceptibility to infections.
- Bronchi and Bronchioles: Branching airways from the trachea, lined with cartilage, cilia, and mucus. Bronchioles are smaller than bronchi and lack cartilage but still have smooth muscle, cilia, and mucus.
- Asthma: A condition where allergens, pollution, stress, exercise, or infections can trigger bronchiole constriction and excess mucus production, leading to difficulty breathing. Asthma attacks can be fatal but treated with inhalers.
Alveoli and Gas Exchange
- Alveoli: Tiny air sacs at the ends of bronchioles responsible for gas exchange. The lungs contain about 300 million alveoli, offering a large surface area for oxygen and carbon dioxide exchange.
- Emphysema: A chronic lung disease causing deterioration of alveoli over time. This leads to reduced gas exchange, difficulty breathing, and increased heart workload. Smoking is the primary cause, although genetic factors and infections can also contribute.
Breathing Process
- Inhalation (breathing in): Contraction of the diaphragm and external intercostal muscles expands the lungs, decreasing pressure and drawing air inward.
- Exhalation (breathing out): Relaxation of muscles causes the chest cavity to recoil, compressing the lungs and expelling air.
- Active exhalation: Abdominal muscles contract to push the diaphragm up, and internal intercostal muscles pull ribs inward, aiding in forced exhalation.
Lungs and Pleural Membranes
- Lungs: Contain bronchi, bronchioles, blood vessels, and alveoli.
- Pleural Membranes: Two layers surrounding the lungs and lining the chest cavity. These membranes contain lubricating fluid, allowing the lungs to expand and contract smoothly during breathing.
Gas transport:
- Oxygen: Mostly transported in the blood bound to hemoglobin with a small portion dissolved in plasma.
- Carbon Dioxide: Transported in the blood by binding to hemoglobin, dissolving in plasma, or as bicarbonate ions.
Nervous System and Breathing
- Respiratory Center: Located in the medulla oblongata, this brain region controls the basic breathing pattern. It stimulates the diaphragm and intercostal muscles every 4-5 seconds for inhalation. Stretch receptors in the lungs signal the brain to stop muscle contractions, leading to exhalation.
Chemical Regulation of Breathing
- Medulla Oblongata: Monitors hydrogen ions (CO₂) levels in cerebrospinal fluid. Increased CO₂ leads to faster and deeper breathing.
- Carotid and Aortic Bodies: These chemoreceptors sense oxygen levels in the blood. Decreased oxygen triggers increased breathing rate.
Respiratory Disorders:
- Pneumonia: Inflammation and fluid build-up in the alveoli due to bacterial or viral infection, hindering gas exchange. Pneumonia can be life-threatening.
- Tuberculosis: Bacterial infection causing lung damage and scarring. While 25% of the world's population has TB, only 5-15% exhibit symptoms. Without treatment, TB is fatal.
- Cystic Fibrosis: A genetic disorder leading to thick mucus buildup in the airways, impeding gas exchange and increasing infection risk. Regular lung drainage is necessary for management.
- Lung Cancer: Uncontrolled growth of lung cells leading to tumors. Over 90% of lung cancer cases are linked to cigarette smoking.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.