Podcast
Questions and Answers
Which of the following is NOT a dynamic stabilizer of the glenohumeral joint?
Which of the following is NOT a dynamic stabilizer of the glenohumeral joint?
- Rotator cuff muscles
- Glenoid labrum (correct)
- GH joint movers
- Scapular stabilizers
What type of impingement is typically associated with structural variations in the acromion?
What type of impingement is typically associated with structural variations in the acromion?
- Dynamic impingement
- Primary impingement (correct)
- Internal impingement
- Secondary impingement
Which rotator cuff muscle is primarily responsible for internal rotation?
Which rotator cuff muscle is primarily responsible for internal rotation?
- Infraspinatus
- Subscapularis (correct)
- Teres minor
- Supraspinatus
What is a common factor contributing to rotator cuff injury?
What is a common factor contributing to rotator cuff injury?
Which of the following tests is used to assess a rotator cuff tear?
Which of the following tests is used to assess a rotator cuff tear?
What is a characteristic symptom of rotator cuff pain that distinguishes it from other shoulder conditions?
What is a characteristic symptom of rotator cuff pain that distinguishes it from other shoulder conditions?
Which condition is indicated by visible atrophy of the supraspinatus and infraspinatus muscles?
Which condition is indicated by visible atrophy of the supraspinatus and infraspinatus muscles?
During rehabilitation, what is the recommended frequency for performing strengthening exercises for shoulder recovery?
During rehabilitation, what is the recommended frequency for performing strengthening exercises for shoulder recovery?
In the management of rotator cuff injuries, which exercise should be prioritized in the early rehabilitation stages?
In the management of rotator cuff injuries, which exercise should be prioritized in the early rehabilitation stages?
In a patient with rotator cuff pathology, which action typically leads to increased pain during shoulder range of motion activities?
In a patient with rotator cuff pathology, which action typically leads to increased pain during shoulder range of motion activities?
What is the maximum duration of an unsuccessful nonoperative treatment program for rotator cuff issues?
What is the maximum duration of an unsuccessful nonoperative treatment program for rotator cuff issues?
What classification of rotator cuff tears primarily focuses on the mechanism of injury?
What classification of rotator cuff tears primarily focuses on the mechanism of injury?
Which symptom is NOT typical for Neer’s classification stage II / III?
Which symptom is NOT typical for Neer’s classification stage II / III?
Which factor does NOT influence the progression of rehabilitation after rotator cuff repair?
Which factor does NOT influence the progression of rehabilitation after rotator cuff repair?
In which population is chronic rotator cuff tearing most commonly observed?
In which population is chronic rotator cuff tearing most commonly observed?
What is a noted advantage of early surgical repair for acute rotator cuff tears?
What is a noted advantage of early surgical repair for acute rotator cuff tears?
What is typically assessed in addition to the shoulder girdle during pain management?
What is typically assessed in addition to the shoulder girdle during pain management?
What is the typical treatment approach for chronic rotator cuff tears?
What is the typical treatment approach for chronic rotator cuff tears?
What type of rotator cuff tear indicates complete involvement of the tendon?
What type of rotator cuff tear indicates complete involvement of the tendon?
Which symptom is often associated with chronic cases and may indicate adhesive capsulitis?
Which symptom is often associated with chronic cases and may indicate adhesive capsulitis?
Flashcards
What are Dynamic Stabilizers?
What are Dynamic Stabilizers?
Dynamic stabilizers are muscles that play a crucial role in providing stability to the shoulder joint. These muscles include the rotator cuff muscles, scapular stabilizers, and GH joint movers.
What are Static Stabilizers?
What are Static Stabilizers?
Static stabilizers are structures that provide passive stability to the shoulder joint. They include bony anatomy, the glenoid labrum, the capsule, and ligaments.
Rotator Cuff Injuries: Causes
Rotator Cuff Injuries: Causes
Rotator cuff injuries often occur due to impingement syndromes, repetitive microtrauma (such as overuse), direct blows, or excessive tensile forces.
What is Primary Impingement?
What is Primary Impingement?
Signup and view all the flashcards
What is Secondary Impingement?
What is Secondary Impingement?
Signup and view all the flashcards
Pain Pattern in Rotator Cuff Impingement
Pain Pattern in Rotator Cuff Impingement
Signup and view all the flashcards
Painful Arc of Abduction
Painful Arc of Abduction
Signup and view all the flashcards
Stage II: Tendenitis and Fibrosis
Stage II: Tendenitis and Fibrosis
Signup and view all the flashcards
Positive Drop Arm Test
Positive Drop Arm Test
Signup and view all the flashcards
Early Stage Exercise for Rotator Cuff Impingement
Early Stage Exercise for Rotator Cuff Impingement
Signup and view all the flashcards
Chronic Rotator Cuff Tear
Chronic Rotator Cuff Tear
Signup and view all the flashcards
Acute Rotator Cuff Tear
Acute Rotator Cuff Tear
Signup and view all the flashcards
Full-Thickness Rotator Cuff Tear
Full-Thickness Rotator Cuff Tear
Signup and view all the flashcards
Partial-Thickness Rotator Cuff Tear
Partial-Thickness Rotator Cuff Tear
Signup and view all the flashcards
Nonoperative Treatment for Rotator Cuff Tears
Nonoperative Treatment for Rotator Cuff Tears
Signup and view all the flashcards
Treatment Options for Rotator Cuff Tears
Treatment Options for Rotator Cuff Tears
Signup and view all the flashcards
Range of Motion Assessment for Rotator Cuff Tears
Range of Motion Assessment for Rotator Cuff Tears
Signup and view all the flashcards
Surgical Repair for Acute Rotator Cuff Tears
Surgical Repair for Acute Rotator Cuff Tears
Signup and view all the flashcards
Advantages of Early Surgical Repair
Advantages of Early Surgical Repair
Signup and view all the flashcards
Factors Influencing Rehabilitation After Rotator Cuff Repair
Factors Influencing Rehabilitation After Rotator Cuff Repair
Signup and view all the flashcards
Study Notes
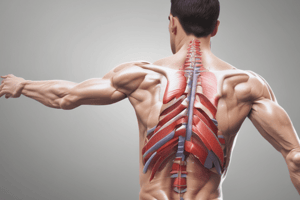
Shoulder Joint Injuries
- The glenohumeral joint is a common injury site in competitive sports.
- Dynamic stabilizers include the rotator cuff muscles, scapular stabilizers, and glenohumeral joint movers.
- Static stabilizers include bony anatomy, glenoid labrum, capsule, and ligaments.
Rotator Cuff Injuries
- Four muscles comprise the rotator cuff: supraspinatus, infraspinatus, teres minor, and subscapularis.
- These muscles dynamically stabilize the shoulder throughout its range of motion (ROM).
- The infraspinatus, teres minor, and subscapularis depress the humeral head, countering the upward pull of the deltoid.
- Infraspinatus and teres minor perform external rotation, while the subscapularis performs internal rotation.
Scapular Dysfunction
- Improper positioning of the scapula relative to the humerus can lead to rotator cuff tears due to instability and impingement.
Factors of Rotator Cuff Injury
- Impingement syndromes
- Repetitive microtrauma
- Direct blows
- Excessive tensile forces
Impingement Syndrome
- Classified as intrinsic or extrinsic.
- Intrinsic causes involve acromion derangement, damaging or irritating the supraspinatus tendon.
- Extrinsic causes can be primary or secondary.
- Primary impingement results from chronic overhead movements (baseball, swimming).
- Secondary impingement is caused by muscular imbalance, particularly in overhead athletes.
Clinical Presentation
- Impingement syndrome typically presents with anterior superior lateral shoulder pain, exacerbated by overhead movements.
- Pain often has a gradual onset, associated with increased training activity or changes to sporting equipment use.
- Sleep disturbance is a potential symptom.
- Painful arc often felt between 45 and 120 degrees of abduction.
- Clinical evaluation involves checking for pain in particular ranges of motion.
Primary Impingement
- Crowding of the subacromial space
- Hypertrophic degenerative changes of the AC joint.
- Thickening or calcification of the coracoacromial ligament
- Subacromial bursa thickening and fibrosis
- Increased thoracic kyphosis
- Structural acromion variations
- Trauma (macrotrauma or microtrauma)
Secondary Impingement
- Commonly stems from glenohumeral or scapulothoracic instability.
- Instability at the glenohumeral joint can arise from excessive demands on the capsule, ligaments, and labrum.
- Factors such as fatigue and tendon injury contribute to anterior glenohumeral instability.
Internal Impingement
- 90° abduction and 90° external rotation position causes posterior and superior rotation of the rotator cuff tendons
- Tendons may get pinched or compressed between the humeral head and the glenoid rim.
Diagnosis
- Diagnosis is generally made clinically via range of motion tests.
- Painful arc, typically between 45 and 120 degrees of abduction, suggests impingement.
- Manual strength testing assesses potential weakness, particularly in abduction, internal, and external rotations.
Special Tests
- Neer test, full/empty can tests(supraspinatus), drop arm test, and Hawkins impingement test are used to assess for impingement.
Neer's Classification
- Stage I: Edema and hemorrhage (usually in patients <25 years)
- Stage II: Tendinitis/bursitis and fibrosis (typically in patients 25-40 years)
- Stage III: Bone spurs and tendon rupture (common in patients >40 years old)
Early clinical stages & symptom notes
- Aching after use only
- Painful arch during abduction (60° to 120°)
- Pain-free passive movements
- Clinicians rarely see patients during this stage
Activity Modification
- Avoid impingement positions during activities of daily living (ADLs) and training.
- Avoid poor postures.
- Ice therapy after workouts
- Ensure scapular dynamic stability
- Maintain correct exercise positions
- Regular evaluation of pain, muscle strength, and range of motion (ROM)
Later Stage Interventions
- Regular ROM and stretching exercises.
- Strengthening exercises (3 times weekly).
- Modalities (heat or cold).
- Manual therapy.
- ROM exercises (e.g., shrugs, shoulder retractions, pendulum exercises).
- Scapular retraction specific exercises.
Progress to Active Assisted Motion
- Cane, suspended pulleys or uninvolved arm support, progressing to active motion as comfort dictates.
- Scapular plane exercises (flexion and abduction), initially separate.
- Stretching of anterior and posterior shoulder muscles (30s holds, 10s rest, 5-10 repetitions).
Strengthening Exercises
- Focus on rotator cuff and scapular stabilizing muscles.
- Exercises include TheraBand and weight-based exercises,
- Scapula stabilizing exercises involve upper, middle, and lower trapezius, serratus anterior, anterior, middle deltoid, supraspinatus, infraspinatus, and teres minor strength training using exercises like chair press, push-up plus, and press-ups.
Chronic Tears, other factors, and classifications
- Common in individuals >50 years with no prior shoulder trauma.
- Characterized by intermittent shoulder pain.
- Conservative rehabilitation may result in a successful outcome for chronic tears.
- If the injuries are caused by acute injuries, surgical repair is required or considered.
- Factors impacting successful rehabilitation include injury onset and location, associated pathologies (glenohumeral instability or fracture), preoperative strength and mobility, general health, patient age, approach type, repair type, patient mobility, and compliance.
Pain Management
- Assess all shoulder joint areas, including cervical and thoracic spine segments, in addition to evaluating symptoms associated with the upper cross syndrome or scapular control.
Postoperative Management
- Phase I: Immediate post-surgical phase.
- Precautions include avoiding shoulder movements, lifting, and reaching behind the back.
- Encourage continuous use of a shoulder splint.
Goals of management
- Diminish pain and inflammation through cold therapy or electrical stimulation.
- Preserve & protect the repair area integrity.
- Maintain abduction orthosis or pillow position.
- Maintain scapular plane and shoulder/elbow position
- Duration of immobilization depends on tear size.
Preventing Mobility & Strength Loss and other issues
- Maintain active ROM of the elbow, wrist, hand and cervical spine.
- Pendulum exercises are implemented on the first postoperative day.
- Removal of the immobilizer allows for exercise and passive ROM.
- Maintain a supine position during initial phases to sustain scapular stability against the thorax.
Prevent or Correct Postural Deviations
- Posture training and exercises are done to address and correct excessive thoracic kyphosis.
- Low-intensity muscle-setting and isometric exercises in the healing period.
- Exercises should be initiated as early as 1–3 weeks post-surgery, dependent on the extent of the tear and the quality of the repair.
Develop Control of Rotator Cuff and Scapulothoracic Stabilizers
- Active movements of the scapula.
- Submaximal isometrics of scapular muscles (side-lying).
- Scapular isometric protraction, retraction, and elevation/depression.
- Rotator cuff submaximal isometrics at the end of the phase
Phase II: Protection and Protected Active Motion
- Precautions: no lifting (>5lb), no excessive behind-the-back movements, no sudden movements, and no body weight support on the hands.
- Goals: allow soft tissue healing, continued progress towards full pain-free ROM, and decrease pain and inflammation.
- Restore near-complete, non-painful, passive mobility.
- Active assisted range of motion (ROM) for shoulder, initially in supine position with elbow flexed.
Phase III: Early Strengthening
- Precautions: no lifting (>5lb), no sudden movements, and exercise should not be painful.
- Continue with stretching, joint mobilization, and passive range of motion (PROM) exercises.
- Increase shoulder strength, endurance, and dynamic stability.
- Isometric and dynamic strengthening exercises focusing on the rotator cuff and other glenohumeral muscles.
- Isotonic strengthening exercises tailored for pain-free ranges and light resistance.
- Initiate light functional activities gradually.
Phase VI: Advanced Strengthening
- Continue ROM exercises.
- Continue progressive isotonic strengthening exercises.
- Implement advanced proprioceptive and neuromuscular activities (PNF).
Proximal Biceps Tendonitis
- Repeated use of the biceps, or problems in the shoulder area, can irritate the proximal biceps tendon.
- Symptoms include pain in the shoulder and proximal biceps area.
Bicipital Tendonitis
- More prevalent in overhead athletes, such as baseball pitchers, swimmers, and tennis players.
- Direct injury or trauma to the tendon from excessive abduction or external rotations can lead to this condition.
Bicipital Tendonitis: Clinical Presentation
- Athletes typically report pain with overhead activities or lifting weights.
- Pain is usually located in the anterior part of the shoulder.
- Pain typically manifests as an aching sensation exacerbated by overhead movements, pushing, or pulling.
- Pain may diminish with rest.
Bicipital Tendonitis: Diagnosis
- Physical examination reveals localized tenderness over the bicipital groove with pain during elbow flexion against resistance.
- Diagnostic tests include speed test and Yergason test.
Bicipital Tendonitis: Treatment
- Initially, treatment involves 3-4 weeks of NSAIDs for reducing inflammation and pain, supplemented by rest and ice.
- Patients should avoid painful movements and activities like lifting or reaching.
- Physical therapy is often recommended to achieve and maintain full and pain-free range of motion (ROM), bolster strength, and enhance endurance.
Return to Play
- Athletes can usually return to play within approximately 3 weeks from treatment commencement, pending complete pain relief.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.