Podcast
Questions and Answers
What is the main indicator that a patient may have ongoing occult hemorrhage after initial treatment?
What is the main indicator that a patient may have ongoing occult hemorrhage after initial treatment?
- Deterioration after initial response (correct)
- Improvement in hypotension
- Decrease in heart rate
- Increased blood pressure immediately
Which of the following symptoms is NOT associated with clinical manifestations of severe fluid deficit?
Which of the following symptoms is NOT associated with clinical manifestations of severe fluid deficit?
- Cold extremities
- Increased urination (correct)
- Palpitations
- Fainting
When should blood transfusion be considered in a patient with suspected hemorrhage?
When should blood transfusion be considered in a patient with suspected hemorrhage?
- When there is significant tachycardia only
- If hemorrhage exceeds 25% of total blood volume (correct)
- When hypotension is evident
- If hemorrhage is more than 15% of total blood volume
What should be done if the patient's blood pressure begins to rise after starting fluid therapy?
What should be done if the patient's blood pressure begins to rise after starting fluid therapy?
Which of the following describes cardiogenic shock?
Which of the following describes cardiogenic shock?
What condition is characterized by decreased perfusion of the tissues in the body?
What condition is characterized by decreased perfusion of the tissues in the body?
Rheumatic heart disease typically arises from which initial condition?
Rheumatic heart disease typically arises from which initial condition?
Which type of shock results from excessive hemorrhage and fluid loss?
Which type of shock results from excessive hemorrhage and fluid loss?
What is a potential complication of shock?
What is a potential complication of shock?
Which type of shock is NOT classified under the distributive category?
Which type of shock is NOT classified under the distributive category?
What is one of the causes of hypovolemic shock?
What is one of the causes of hypovolemic shock?
Which factor increases the risk for rheumatic heart disease?
Which factor increases the risk for rheumatic heart disease?
Which of the following is NOT a type of distributive shock?
Which of the following is NOT a type of distributive shock?
What initial action should be taken in the management of an allergic reaction?
What initial action should be taken in the management of an allergic reaction?
What is the correct dosage for Adrenaline when managing severe allergic reactions?
What is the correct dosage for Adrenaline when managing severe allergic reactions?
Which of the following statements is true about the complications of severe allergic reactions?
Which of the following statements is true about the complications of severe allergic reactions?
What is a common clinical manifestation associated with latex allergy?
What is a common clinical manifestation associated with latex allergy?
Which symptom indicates the most severe possible reaction from latex allergy?
Which symptom indicates the most severe possible reaction from latex allergy?
What factors influence the choice of antibiotics?
What factors influence the choice of antibiotics?
Which medication is used for the prevention of stress gastric ulcers in critically ill patients?
Which medication is used for the prevention of stress gastric ulcers in critically ill patients?
What is the primary reason for referring a patient if urinary output starts failing?
What is the primary reason for referring a patient if urinary output starts failing?
Which of the following is NOT a complication listed?
Which of the following is NOT a complication listed?
Which of the following is a common cause of anaphylactic shock?
Which of the following is a common cause of anaphylactic shock?
Which class of medications is known to potentially cause anaphylactic reactions?
Which class of medications is known to potentially cause anaphylactic reactions?
What is a major characteristic of anaphylactic shock?
What is a major characteristic of anaphylactic shock?
What is crucial to monitor in critically ill patients to prevent complications?
What is crucial to monitor in critically ill patients to prevent complications?
What is the primary characteristic of 'warm hypotension' in patients?
What is the primary characteristic of 'warm hypotension' in patients?
Which laboratory investigation is commonly used to evaluate kidney function?
Which laboratory investigation is commonly used to evaluate kidney function?
What is the recommended empirical antibiotic therapy for septic patients after cultures have been obtained?
What is the recommended empirical antibiotic therapy for septic patients after cultures have been obtained?
Which vasopressor is commonly recommended as a first-line treatment for hypotension?
Which vasopressor is commonly recommended as a first-line treatment for hypotension?
What is the initial step in managing a patient showing signs of septic shock?
What is the initial step in managing a patient showing signs of septic shock?
When is it recommended to administer Hydrocortisone in cases of septic shock?
When is it recommended to administer Hydrocortisone in cases of septic shock?
What is the target mean arterial pressure (MAP) for patients requiring vasopressors?
What is the target mean arterial pressure (MAP) for patients requiring vasopressors?
What type of mechanical ventilation strategy is suggested for patients with ARDS?
What type of mechanical ventilation strategy is suggested for patients with ARDS?
Flashcards are hidden until you start studying
Study Notes
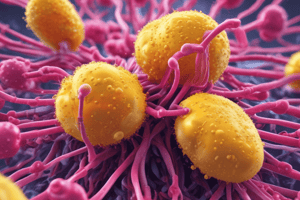
Shock
- Syndrome characterized by decreased tissue perfusion
- If prolonged, leads to multi-organ failure
- Types:
- Hypovolemic: Due to loss of intravascular fluid volume (blood and/ or fluid loss)
- Cardiogenic: Advanced cardiac failure with inadequate peripheral tissue perfusion
- Distributive:
- Obstructive
- Anaphylactic
- Neurogenic
- Septic
- Respiratory shock
Hypovolemic Shock
- Caused by excessive haemorrhage, fluid loss, or intestinal obstruction
- Symptoms:
- Fainting
- Palpitations
- Sweating
- Restlessness, clouding of consciousness
- Signs:
- Pallor
- Cold extremities
- Tachycardia
- Hypotension: Systolic BP < 30ml/hr
- Fluid bolus should be given with close monitoring of BP, pulse, and urine output, blood transfusions may be required
Rheumatic Heart Disease
- Occurs when heart valves are permanently damaged by rheumatic fever
- Rheumatic fever is an inflammatory disease affecting connective tissues, especially the heart
- Untreated or under-treated Strep infections increase risk
Septic Shock
- Clinical Manifestation:
- Low blood pressure but warm skin (“warm hypotension”)
- General malaise, chills
- Fatigue, weakness, pain
- Nausea and vomiting
- Skin signs: petechiae, haematoma
- Confusion
- Unexplained worsening of underlying illness
- Investigations:
- CBC, Urea, Creatinine, Electrolytes, Blood sugar, Blood and body fluid culture, Liver function tests, Coagulation tests, Chest X-ray, ABG
- Management:
- Commence resuscitation measures
- Start broad-spectrum antibiotics within 1 hour
- Fluid replacement, monitor urea, creatinine, electrolytes
- Consider hydrocortisone for septic shock patients
- Vasopressors for hypotension
- Oxygenotherapy and mechanical ventilation if needed
- Manage disseminated intravascular coagulopathy, stress gastric ulcers, DVT
Anaphylactic Shock
- Life-threatening allergic reaction with respiratory difficulties and circulatory failure
- Causes:
- Foods: nuts, fish, seafood, etc.
- Drugs: antibiotics, analgesics, ACE inhibitors
- Vaccines and serum
- Insect stings
- Radiographic contrast media, blood products, allergenic products
- Natural rubber (latex allergy)
- Physical exercise (rarely)
- Clinical Manifestation:
- Erythema
- Angioedema
- Rash
- Urticaria
- Bronchospasm
- Cardiovascular collapse
- severe hypotension
- Management:
- Stop administration of potential trigger
- Maintain airway, give O2 100%
- Elevate the legs
- Give Adrenaline
- Give IV fluid (Crystalloid)
- Complications:
- Circulatory and respiratory arrest
Complications of Shock (General)
- Renal Failure
- Hepatic Failure
- Metabolic Acidosis
- Coma, Death - ARDS
- Acute Kidney Disease
- DIC
- Liver Failure
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.