Podcast
Questions and Answers
What is the basic underlying cause of autoimmune diseases?
What is the basic underlying cause of autoimmune diseases?
- Increased aging factor
- Excessive immune responses
- Environmental toxins
- Failure of self-tolerance (correct)
What can promote T-cell death by apoptosis?
What can promote T-cell death by apoptosis?
- Increased production of antibodies
- Recognition of foreign antigens
- Signals that recognize self-antigens (correct)
- Exposure to viral infections
Which of the following is a type of autoimmune disorder mediated by antibodies?
Which of the following is a type of autoimmune disorder mediated by antibodies?
- Rheumatoid arthritis
- Multiple sclerosis
- Lupus (correct)
- Type 1 diabetes
What are susceptibility genes related to in the context of autoimmunity?
What are susceptibility genes related to in the context of autoimmunity?
Which of the following is considered a systemic autoimmune disorder?
Which of the following is considered a systemic autoimmune disorder?
What kind of autoimmune disorder is autoimmune hemolytic anemia?
What kind of autoimmune disorder is autoimmune hemolytic anemia?
Which factor is NOT typically considered a predisposing factor for autoimmunity?
Which factor is NOT typically considered a predisposing factor for autoimmunity?
What is a common clinical presentation of autoimmune disorders?
What is a common clinical presentation of autoimmune disorders?
What percentage of patients experience parotid gland enlargement?
What percentage of patients experience parotid gland enlargement?
Which of the following extraglandular diseases is not listed as a complication?
Which of the following extraglandular diseases is not listed as a complication?
What is a common defect observed in patients related to renal function?
What is a common defect observed in patients related to renal function?
Which autoimmune disorder is most commonly associated with this condition?
Which autoimmune disorder is most commonly associated with this condition?
What is the outcome associated with high titers of anti-SS-A antibodies?
What is the outcome associated with high titers of anti-SS-A antibodies?
What condition arises from the inflammatory destruction of the exocrine glands producing keratoconjunctivitis?
What condition arises from the inflammatory destruction of the exocrine glands producing keratoconjunctivitis?
Which symptom is specifically associated with xerostomia?
Which symptom is specifically associated with xerostomia?
What are potential consequences of keratoconjunctivitis?
What are potential consequences of keratoconjunctivitis?
Which organ system can be affected by the same process that causes symptoms like keratoconjunctivitis and xerostomia?
Which organ system can be affected by the same process that causes symptoms like keratoconjunctivitis and xerostomia?
What is a common symptom indicating keratoconjunctivitis?
What is a common symptom indicating keratoconjunctivitis?
Which statement best describes xerostomia?
Which statement best describes xerostomia?
Which of the following symptoms results from keratoconjunctivitis?
Which of the following symptoms results from keratoconjunctivitis?
What complication can result from the lack of tears due to keratoconjunctivitis?
What complication can result from the lack of tears due to keratoconjunctivitis?
Which of the following is a true statement regarding the systemic effects of gland dysfunction related to these conditions?
Which of the following is a true statement regarding the systemic effects of gland dysfunction related to these conditions?
What accumulation occurs in the conjunctival sac due to keratoconjunctivitis?
What accumulation occurs in the conjunctival sac due to keratoconjunctivitis?
What is a common histologic finding in the kidneys of patients with systemic lupus erythematosus (SLE)?
What is a common histologic finding in the kidneys of patients with systemic lupus erythematosus (SLE)?
What type of microscopy reveals deposition of immunoglobulin and complement in SLE?
What type of microscopy reveals deposition of immunoglobulin and complement in SLE?
Which cellular component is often involved in the perivascular inflammation seen in SLE?
Which cellular component is often involved in the perivascular inflammation seen in SLE?
What histological change occurs in the epidermis due to SLE skin involvement?
What histological change occurs in the epidermis due to SLE skin involvement?
What finding is NOT specific for systemic lupus erythematosus (SLE) but can occur in other autoimmune diseases?
What finding is NOT specific for systemic lupus erythematosus (SLE) but can occur in other autoimmune diseases?
In patients with SLE, what type of renal pathology is primarily observed in the glomeruli?
In patients with SLE, what type of renal pathology is primarily observed in the glomeruli?
What skin condition is most closely associated with SLE and characterized by a distinct appearance?
What skin condition is most closely associated with SLE and characterized by a distinct appearance?
What type of necrosis may be prominent in the vasculitis seen in SLE?
What type of necrosis may be prominent in the vasculitis seen in SLE?
What percentage of SLE patients have clinically significant renal involvement?
What percentage of SLE patients have clinically significant renal involvement?
Which characteristic change in the dermis is associated with SLE skin lesions?
Which characteristic change in the dermis is associated with SLE skin lesions?
What is one primary result of xerostomia?
What is one primary result of xerostomia?
What might happen to the oral mucosa in patients with xerostomia?
What might happen to the oral mucosa in patients with xerostomia?
What type of skin involvement is observed in the limited form of xerostomia?
What type of skin involvement is observed in the limited form of xerostomia?
How does the clinical course of limited xerostomia compare to diffuse xerostomia?
How does the clinical course of limited xerostomia compare to diffuse xerostomia?
What is not a symptom associated with xerostomia?
What is not a symptom associated with xerostomia?
In what way does xerostomia impact the ability to taste?
In what way does xerostomia impact the ability to taste?
Which of the following is a potential feature of xerostomia?
Which of the following is a potential feature of xerostomia?
What do cracks and fissures in the mouth indicate in relation to xerostomia?
What do cracks and fissures in the mouth indicate in relation to xerostomia?
Which statement about the symptoms of xerostomia is accurate?
Which statement about the symptoms of xerostomia is accurate?
What could be a long-term complication of untreated xerostomia?
What could be a long-term complication of untreated xerostomia?
What disorder is most commonly caused by antiplatelet autoantibodies in SLE patients?
What disorder is most commonly caused by antiplatelet autoantibodies in SLE patients?
What percentage of lupus patients may present with antiphopholipid antibodies?
What percentage of lupus patients may present with antiphopholipid antibodies?
Which clinical condition is referred to as the secondary antiphospholipid antibody syndrome (APAS)?
Which clinical condition is referred to as the secondary antiphospholipid antibody syndrome (APAS)?
Antinuclear antibodies (ANAs) are primarily directed against which of the following?
Antinuclear antibodies (ANAs) are primarily directed against which of the following?
Which pattern of glomerular disease is categorized as minimal mesangial lupus nephritis?
Which pattern of glomerular disease is categorized as minimal mesangial lupus nephritis?
Which statement is true regarding antiphospholipid antibodies in the context of SLE?
Which statement is true regarding antiphospholipid antibodies in the context of SLE?
What autoimmune response is classified under Type IIa autoantibodies?
What autoimmune response is classified under Type IIa autoantibodies?
What is a potential clinical outcome associated with the presence of antiphospholipid antibodies?
What is a potential clinical outcome associated with the presence of antiphospholipid antibodies?
Which area is NOT mentioned as being affected by scleroderma?
Which area is NOT mentioned as being affected by scleroderma?
What type of autoantibody is specifically anti-Scl 70?
What type of autoantibody is specifically anti-Scl 70?
Which of the following is a condition that may result from severe scleroderma?
Which of the following is a condition that may result from severe scleroderma?
What describes the specific skin changes associated with advanced stage scleroderma?
What describes the specific skin changes associated with advanced stage scleroderma?
What is a potential consequence of loss of blood supply to the phalanges in scleroderma?
What is a potential consequence of loss of blood supply to the phalanges in scleroderma?
Which role do autoantibodies play in the pathology of scleroderma?
Which role do autoantibodies play in the pathology of scleroderma?
What type of antibodies are present in virtually all scleroderma patients?
What type of antibodies are present in virtually all scleroderma patients?
What is the specificity of anti-Scl 70 antibodies?
What is the specificity of anti-Scl 70 antibodies?
What might indicate the presence of auto-amputation in scleroderma patients?
What might indicate the presence of auto-amputation in scleroderma patients?
How might anti-nuclear antibodies contribute to the disease mechanism in scleroderma?
How might anti-nuclear antibodies contribute to the disease mechanism in scleroderma?
What is a common clinical feature of systemic sclerosis?
What is a common clinical feature of systemic sclerosis?
Which symptom often precedes other symptoms in systemic sclerosis?
Which symptom often precedes other symptoms in systemic sclerosis?
What is a known complication associated with myocardial fibrosis in systemic sclerosis?
What is a known complication associated with myocardial fibrosis in systemic sclerosis?
What age group has the peak incidence of systemic sclerosis?
What age group has the peak incidence of systemic sclerosis?
What gastrointestinal issue is commonly associated with systemic sclerosis?
What gastrointestinal issue is commonly associated with systemic sclerosis?
What are the potential symptoms of myocarditis?
What are the potential symptoms of myocarditis?
Which condition is characterized by the presence of fibrinous exudate on mesothelial surfaces?
Which condition is characterized by the presence of fibrinous exudate on mesothelial surfaces?
What is a potential complication of chronic inflammation in the cardiovascular system?
What is a potential complication of chronic inflammation in the cardiovascular system?
Which valves are primarily affected by valvular abnormalities?
Which valves are primarily affected by valvular abnormalities?
What happens to mesothelial surfaces as inflammation progresses into the chronic phase?
What happens to mesothelial surfaces as inflammation progresses into the chronic phase?
Which of the following statements is true regarding pericarditis?
Which of the following statements is true regarding pericarditis?
What types of effusions may accompany myocarditis?
What types of effusions may accompany myocarditis?
What is a typical electrocardiogram change seen in myocarditis?
What is a typical electrocardiogram change seen in myocarditis?
In which phase does the serosal cavity begin to present with shaggy fibrous tissue?
In which phase does the serosal cavity begin to present with shaggy fibrous tissue?
Which phase of inflammation includes covering of mesothelial surfaces with fibrinous exudate?
Which phase of inflammation includes covering of mesothelial surfaces with fibrinous exudate?
What is the potential consequence of malignant hypertension in patients with systemic sclerosis?
What is the potential consequence of malignant hypertension in patients with systemic sclerosis?
Which autoantibody is associated with diffuse systemic sclerosis?
Which autoantibody is associated with diffuse systemic sclerosis?
Which of the following findings is common in patients with CREST syndrome?
Which of the following findings is common in patients with CREST syndrome?
What type of vascular change is associated with hypertension in systemic sclerosis?
What type of vascular change is associated with hypertension in systemic sclerosis?
In systemic sclerosis, what percentage of patients has anti-centromere antibodies?
In systemic sclerosis, what percentage of patients has anti-centromere antibodies?
What is a characteristic feature of malignant hypertension as described in systemic sclerosis?
What is a characteristic feature of malignant hypertension as described in systemic sclerosis?
What factor increases the likelihood of pulmonary fibrosis in systemic sclerosis patients?
What factor increases the likelihood of pulmonary fibrosis in systemic sclerosis patients?
What histopathological change is NOT typical in patients with systemic sclerosis concerning renal health?
What histopathological change is NOT typical in patients with systemic sclerosis concerning renal health?
Which symptom is associated with hypertension leading to renal complications in systemic sclerosis?
Which symptom is associated with hypertension leading to renal complications in systemic sclerosis?
What is a common risk associated with the presence of autoantibodies in systemic sclerosis?
What is a common risk associated with the presence of autoantibodies in systemic sclerosis?
Flashcards are hidden until you start studying
Study Notes
Apoptosis and Autoimmunity
- T-cells that encounter self-antigens may receive signals for apoptosis, preventing autoimmune reactions.
Failure of Self-Tolerance
- Autoimmune diseases stem from the breakdown of self-tolerance, leading to immune responses against self-antigens.
Predisposing Factors of Autoimmunity
- Susceptibility Genes: Inherited genes can disrupt self-tolerance, increasing autoimmune disease risk.
- Examples of Organ-Specific Autoimmune Disorders:
- Autoimmune hemolytic anemia
- Autoimmune thrombocytopenia
- Autoimmune atrophic gastritis
Systemic Lupus Erythematosus (SLE)
- Kidney Involvement: About 50% of SLE patients experience significant renal issues, primarily glomerulonephritis and tubulointerstitial nephritis.
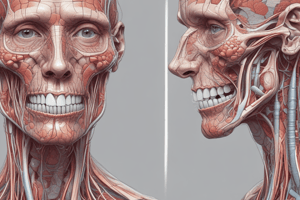
Histologic Findings of SLE
-
Light Microscopy:
- Glomerular lesions: immune complex deposition on glomerular membrane.
- Epidermis shows vacuolar degeneration; dermis may exhibit variable edema.
- Perivascular inflammation with lymphocytic infiltrates may be observed.
-
Immunofluorescence Microscopy:
- Deposition of immunoglobulin and complement at dermoepidermal junction, not exclusive to SLE.
Salivary Gland Involvement
- Symptoms of Inflammation:
- Keratoconjunctivitis: Leads to blurred vision, burning, and itching due to dry eyes.
- Xerostomia: Results in swallowing difficulties, loss of taste, oral fissures, and buccal mucosa dryness.
Other Symptoms in Autoimmunity
- Parotid gland enlargement occurs in 50% of cases.
- Nasal mucosa dryness, leading to epistaxis; recurrent bronchitis and pneumonitis are common.
- Extraglandular manifestations affect about one-third of patients and may include synovitis and peripheral neuropathy.
Major Categories of Autoimmune Conditions
- Diffuse vs. Limited:
- Diffuse: Widespread skin involvement; more aggressive clinical course.
- Limited: Skin involvement primarily on fingers, forearms, face; typically, a more benign course.
CREST Syndrome
- Observed in some patients with limited disease:
- Characterized by Calcinosis, Raynaud's phenomenon, Esophageal dysmotility, Sclerodactyly, and Telangiectasia.
- Patients usually live longer with less visceral organ involvement compared to diffuse forms.
Autoantibody Types in Systemic Lupus Erythematosus (SLE)
- Antinuclear antibodies (ANAs) target nuclear antigens, found in 30-40% of lupus patients.
- Autoantibodies can cause immune thrombocytopenic purpura in up to 10% of SLE cases.
- Antiphospholipid antibodies are linked to venous and arterial thrombosis; may lead to secondary antiphospholipid antibody syndrome (APAS).
- Recurrent miscarriages and focal cerebral or ocular ischemia can also occur.
Glomerular Disease Patterns in SLE
- Six distinct patterns of glomerular disease observed in SLE patients.
Cardiovascular System Involvement
- Cardiovascular issues may arise, affecting various heart layers.
- Pericarditis occurs in up to 50% of patients, can be symptomatic or asymptomatic.
- Myocarditis may present with tachycardia, ECG abnormalities, though uncommon.
- Valvular abnormalities primarily affect the mitral and aortic valves.
Scleroderma Overview
- Scleroderma is characterized as systemic sclerosis, leading to progressive fibrosis in various organs.
- Female predilection with a 3:1 ratio of women to men affected, particularly in the 50-60 age group.
- Autoantibodies including Anti-Scl-70 present in 10-20% of diffuse cases, associated with pulmonary fibrosis.
- Anti-centromere antibodies occur in 20-30% of cases, indicative of CREST syndrome (limited type).
Skin and Vascular Changes in Scleroderma
- Skin changes signify striking cutaneous fibrosis; may lead to atrophic alterations and ulcers.
- Hypertension is common, with a subset experiencing malignant hypertension potentially resulting in renal failure.
- Raynaud’s Phenomenon often precedes other symptoms in approximately 70% of patients, serving as an early indicator.
Clinical Features of Systemic Sclerosis
- Distinctive skin features and organ fibrosis are notable clinical signs.
- Difficulty swallowing (dysphagia) is common, linked to esophageal involvement.
- Endothelial injury, microvascular disease, and chronic ischemia contribute to disease progression and fibrosis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.