Podcast
Questions and Answers
What imaging techniques are typically used to confirm partial rotator cuff tears?
What imaging techniques are typically used to confirm partial rotator cuff tears?
- Fluoroscopy and PET scan
- Ultrasound and MRI (correct)
- X-ray and CT scan
- Bone scan and radiography
Which of the following conditions is NOT associated with degenerative tendinopathy?
Which of the following conditions is NOT associated with degenerative tendinopathy?
- Acute inflammation (correct)
- Chondral metaplasia
- Complete tendon rupture
- Mucoid degeneration
Which statement accurately describes the treatment approach for partial rotator cuff tears?
Which statement accurately describes the treatment approach for partial rotator cuff tears?
- Full-thickness tears are always treated conservatively.
- Conservative measures are typically first-line therapy for tears smaller than 50%. (correct)
- All partial tears must undergo MRI before any intervention.
- Surgical treatment is immediately recommended for all partial tears.
What percentage of individuals in the study had full-thickness rotator cuff tears?
What percentage of individuals in the study had full-thickness rotator cuff tears?
Which histological change is an early sign of reactive tendinopathy?
Which histological change is an early sign of reactive tendinopathy?
Which structural change occurs as a tendon progresses from reactive tendinopathy to degeneration?
Which structural change occurs as a tendon progresses from reactive tendinopathy to degeneration?
What clinical test is frequently associated with a complete tear of the rotator cuff?
What clinical test is frequently associated with a complete tear of the rotator cuff?
What is a common non-surgical intervention for patients with partial rotator cuff tears?
What is a common non-surgical intervention for patients with partial rotator cuff tears?
What might make the diagnosis of a complete rotator cuff tear challenging?
What might make the diagnosis of a complete rotator cuff tear challenging?
Which factor is considered a negative prognostic indicator for surgical treatment of full-thickness rotator cuff tears?
Which factor is considered a negative prognostic indicator for surgical treatment of full-thickness rotator cuff tears?
What percentage of partial thickness rotator cuff tears progresses to full thickness within two years?
What percentage of partial thickness rotator cuff tears progresses to full thickness within two years?
Which condition should be included in the differential diagnosis of rotator cuff pathology?
Which condition should be included in the differential diagnosis of rotator cuff pathology?
What type of rotator cuff tear is most often indicated for surgical repair?
What type of rotator cuff tear is most often indicated for surgical repair?
What is a likely outcome for chronic rotator cuff tears treated with physical therapy?
What is a likely outcome for chronic rotator cuff tears treated with physical therapy?
Which imaging technique is most commonly used to evaluate rotator cuff tears?
Which imaging technique is most commonly used to evaluate rotator cuff tears?
What impact does fatty infiltration have on rotator cuff treatment outcomes?
What impact does fatty infiltration have on rotator cuff treatment outcomes?
Which imaging modality is primarily utilized for assessing soft tissues of the shoulder, including the rotator cuff?
Which imaging modality is primarily utilized for assessing soft tissues of the shoulder, including the rotator cuff?
What is a characteristic of acromial spurs in relation to rotator cuff injuries?
What is a characteristic of acromial spurs in relation to rotator cuff injuries?
In the evaluation of rotator cuff tears, what advantage does ultrasound have over MRI?
In the evaluation of rotator cuff tears, what advantage does ultrasound have over MRI?
What type of tear is characterized by fluid between the layers of the tendon but no disruption of its articular side insertion?
What type of tear is characterized by fluid between the layers of the tendon but no disruption of its articular side insertion?
What condition can mimic rotator cuff tears when evaluating the acromioclavicular joint?
What condition can mimic rotator cuff tears when evaluating the acromioclavicular joint?
Which imaging technique is typically reserved for evaluating fractures or prosthetic joints in shoulder assessments?
Which imaging technique is typically reserved for evaluating fractures or prosthetic joints in shoulder assessments?
What imaging finding is indicative of rotator cuff tendinopathy?
What imaging finding is indicative of rotator cuff tendinopathy?
Which type of rotator cuff tear affects less than 50% of the tendon thickness on the bursal side?
Which type of rotator cuff tear affects less than 50% of the tendon thickness on the bursal side?
Weakness during which maneuver indicates a positive test for supraspinatus rotator cuff tear or bicipital tendinitis?
Weakness during which maneuver indicates a positive test for supraspinatus rotator cuff tear or bicipital tendinitis?
Which test is most effective for assessing infraspinatus involvement due to its sensitivity?
Which test is most effective for assessing infraspinatus involvement due to its sensitivity?
What does pain or weakness during the External Rotation Resistance Test primarily indicate?
What does pain or weakness during the External Rotation Resistance Test primarily indicate?
Which composite test assesses both pain and weakness to potentially diagnose rotator cuff diseases?
Which composite test assesses both pain and weakness to potentially diagnose rotator cuff diseases?
What is the primary purpose of the Gerber Lift Off Test?
What is the primary purpose of the Gerber Lift Off Test?
What is the negative likelihood ratio (LR) for the Internal Rotation Lag Test?
What is the negative likelihood ratio (LR) for the Internal Rotation Lag Test?
What histological change indicates the transition from reactive tendinopathy to degenerative tendinopathy?
What histological change indicates the transition from reactive tendinopathy to degenerative tendinopathy?
Which of the following statements about the treatment of rotator cuff partial tears is correct?
Which of the following statements about the treatment of rotator cuff partial tears is correct?
Which condition is most likely to contribute to the development of tendinopathy in rotator cuff tendons?
Which condition is most likely to contribute to the development of tendinopathy in rotator cuff tendons?
What percentage of the population exhibits partial rotator cuff tears according to the study?
What percentage of the population exhibits partial rotator cuff tears according to the study?
Which of the following features is commonly associated with a complete rotator cuff tear?
Which of the following features is commonly associated with a complete rotator cuff tear?
What is a potential outcome of partial tears larger than 50% in the rotator cuff?
What is a potential outcome of partial tears larger than 50% in the rotator cuff?
What is the significance of neovascularization in degenerative tendinopathy?
What is the significance of neovascularization in degenerative tendinopathy?
What complicates the diagnosis of a complete rotator cuff tear in a clinical setting?
What complicates the diagnosis of a complete rotator cuff tear in a clinical setting?
What is a common cause of axillary nerve denervation in older patients?
What is a common cause of axillary nerve denervation in older patients?
Which MRI finding indicates chronic changes associated with nerve injury?
Which MRI finding indicates chronic changes associated with nerve injury?
What notable appearance may occur after a biceps tenotomy?
What notable appearance may occur after a biceps tenotomy?
What type of trauma is primarily associated with isolated greater tuberosity fractures?
What type of trauma is primarily associated with isolated greater tuberosity fractures?
Which factor is a risk for a proximal biceps rupture?
Which factor is a risk for a proximal biceps rupture?
What complication can arise due to a paralabral cyst in the shoulder?
What complication can arise due to a paralabral cyst in the shoulder?
What characterizes distal biceps tendon ruptures?
What characterizes distal biceps tendon ruptures?
What defines a type IV acromioclavicular injury?
What defines a type IV acromioclavicular injury?
Which condition typically warrants surgical management among acromioclavicular joint injuries?
Which condition typically warrants surgical management among acromioclavicular joint injuries?
In what scenario would a type III acromioclavicular joint injury potentially be treated surgically?
In what scenario would a type III acromioclavicular joint injury potentially be treated surgically?
What distinguishes a type VI acromioclavicular joint injury?
What distinguishes a type VI acromioclavicular joint injury?
When assessing a type III acromioclavicular joint injury on x-ray, what significant measurement change is noted?
When assessing a type III acromioclavicular joint injury on x-ray, what significant measurement change is noted?
What imaging finding is indicative of a type V acromioclavicular joint injury?
What imaging finding is indicative of a type V acromioclavicular joint injury?
What common mechanism of injury is associated with type VI acromioclavicular injuries?
What common mechanism of injury is associated with type VI acromioclavicular injuries?
What is a clinical consequence of a type III acromioclavicular joint injury?
What is a clinical consequence of a type III acromioclavicular joint injury?
What characterizes the precalcification phase of calcified tendinopathy?
What characterizes the precalcification phase of calcified tendinopathy?
Which of the following findings on MRI is associated with adhesive capsulitis?
Which of the following findings on MRI is associated with adhesive capsulitis?
Which of the following potential causes is NOT associated with calcified tendinopathy?
Which of the following potential causes is NOT associated with calcified tendinopathy?
What is a significant complication arising from calcified tendinopathy regarding CPPD deposits?
What is a significant complication arising from calcified tendinopathy regarding CPPD deposits?
What is the most common clinical manifestation of nerve denervation syndromes like suprascapular neuropathy?
What is the most common clinical manifestation of nerve denervation syndromes like suprascapular neuropathy?
Which stage of calcified tendinopathy involves a severe inflammatory reaction?
Which stage of calcified tendinopathy involves a severe inflammatory reaction?
What does MR arthrography typically reveal in cases of adhesive capsulitis?
What does MR arthrography typically reveal in cases of adhesive capsulitis?
What is the significance of the intrabone migration of hydroxyapatite deposition in calcified tendinopathy?
What is the significance of the intrabone migration of hydroxyapatite deposition in calcified tendinopathy?
Which of the following conditions is associated with the degeneration of collagen protein within a tendon?
Which of the following conditions is associated with the degeneration of collagen protein within a tendon?
Which statement accurately describes a contrasting condition to tendinopathy?
Which statement accurately describes a contrasting condition to tendinopathy?
What happens to larger tears in the rotator cuff over time?
What happens to larger tears in the rotator cuff over time?
Which extrinsic shoulder pain cause is associated with left shoulder pain specifically?
Which extrinsic shoulder pain cause is associated with left shoulder pain specifically?
Which condition can lead to shoulder pain due to its impact on the cervical region?
Which condition can lead to shoulder pain due to its impact on the cervical region?
What is the likely relationship between rotator cuff tears and surgical intervention based on size?
What is the likely relationship between rotator cuff tears and surgical intervention based on size?
Which of the following presentations is indicative of a more significant rotator cuff injury?
Which of the following presentations is indicative of a more significant rotator cuff injury?
Which of these extrinsic shoulder pain causes is linked to a cardiovascular issue?
Which of these extrinsic shoulder pain causes is linked to a cardiovascular issue?
Which type of rotator cuff tear is commonly associated with younger individuals and traumatic events?
Which type of rotator cuff tear is commonly associated with younger individuals and traumatic events?
What factor increases the likelihood of recurrence after surgical repair of a rotator cuff tear?
What factor increases the likelihood of recurrence after surgical repair of a rotator cuff tear?
Which structural changes are characteristic of glenohumeral arthrosis in advanced stages?
Which structural changes are characteristic of glenohumeral arthrosis in advanced stages?
What is a common risk factor for developing rotator cuff degeneration?
What is a common risk factor for developing rotator cuff degeneration?
Which type of rotator cuff tear extends from the articular side to the bursal side?
Which type of rotator cuff tear extends from the articular side to the bursal side?
What condition is associated with the presence of osteophytes and loss of joint space?
What condition is associated with the presence of osteophytes and loss of joint space?
In the context of rotator cuff tears, what symptom is most frequently observed during overhead activities?
In the context of rotator cuff tears, what symptom is most frequently observed during overhead activities?
What typically complicates the prognosis of massive rotator cuff tears?
What typically complicates the prognosis of massive rotator cuff tears?
What is the positive likelihood ratio (LR) for the painful arc of abduction test in diagnosing subacromial impingement?
What is the positive likelihood ratio (LR) for the painful arc of abduction test in diagnosing subacromial impingement?
Which test performed by internally rotating the shoulder while flexed at 90 degrees is primarily associated with supraspinatus impingement?
Which test performed by internally rotating the shoulder while flexed at 90 degrees is primarily associated with supraspinatus impingement?
Which of the following clinical tests has the lowest specificity when diagnosing rotator cuff disorders?
Which of the following clinical tests has the lowest specificity when diagnosing rotator cuff disorders?
In the context of rotator cuff disease, what does simultaneous absence of the Hawkins and Neer signs indicate?
In the context of rotator cuff disease, what does simultaneous absence of the Hawkins and Neer signs indicate?
What action signifies a positive result in the Drop arm test?
What action signifies a positive result in the Drop arm test?
What is the negative likelihood ratio (LR) for the Physical Abduction Test in diagnosing supraspinatus impingement?
What is the negative likelihood ratio (LR) for the Physical Abduction Test in diagnosing supraspinatus impingement?
What does weakness during the drop arm test maneuver indicate?
What does weakness during the drop arm test maneuver indicate?
Which test has the highest positive likelihood ratio associated with infraspinatus disorders?
Which test has the highest positive likelihood ratio associated with infraspinatus disorders?
What finding during the External Rotation Lag Test suggests supraspinatus or infraspinatus disorders?
What finding during the External Rotation Lag Test suggests supraspinatus or infraspinatus disorders?
For which disorder is the Gerber Lift Off Test most indicative?
For which disorder is the Gerber Lift Off Test most indicative?
Which composite test assesses omplexity of pain and weakness in rotator cuff diseases?
Which composite test assesses omplexity of pain and weakness in rotator cuff diseases?
Which activity might increase the likelihood of a positive test result for infraspinatus involvement?
Which activity might increase the likelihood of a positive test result for infraspinatus involvement?
What is a common sign that indicates a distal biceps tendon rupture?
What is a common sign that indicates a distal biceps tendon rupture?
Which patient demographic is most commonly associated with distal biceps tendon ruptures?
Which patient demographic is most commonly associated with distal biceps tendon ruptures?
What is one reason proximal biceps ruptures can often coexist with other shoulder conditions?
What is one reason proximal biceps ruptures can often coexist with other shoulder conditions?
What is one significant consequence of a complete distal biceps tendon rupture if left untreated?
What is one significant consequence of a complete distal biceps tendon rupture if left untreated?
Which imaging technique is specifically suggested to assist in the diagnosis of biceps tendon injuries when the clinical diagnosis is unclear?
Which imaging technique is specifically suggested to assist in the diagnosis of biceps tendon injuries when the clinical diagnosis is unclear?
What factor complicates the diagnosis of biceps tendon ruptures?
What factor complicates the diagnosis of biceps tendon ruptures?
What is a characteristic feature of distal biceps tendon ruptures observed clinically?
What is a characteristic feature of distal biceps tendon ruptures observed clinically?
What clinical symptom is characterized by a dull pain becoming sharp during overhead motion?
What clinical symptom is characterized by a dull pain becoming sharp during overhead motion?
Which of the following findings may indicate a chronic full-thickness rotator cuff tear?
Which of the following findings may indicate a chronic full-thickness rotator cuff tear?
Which shoulder examination technique involves comparing the affected extremity with the unaffected side?
Which shoulder examination technique involves comparing the affected extremity with the unaffected side?
What condition can be suggested by scapular winging during shoulder examination?
What condition can be suggested by scapular winging during shoulder examination?
Which examination technique includes assessing tenderness around the biceps tendon and glenohumeral joint?
Which examination technique includes assessing tenderness around the biceps tendon and glenohumeral joint?
Identifying asymmetry and muscle atrophy during an examination may require which of the following considerations?
Identifying asymmetry and muscle atrophy during an examination may require which of the following considerations?
What is one of the factors examined during the inspection phase of a shoulder evaluation?
What is one of the factors examined during the inspection phase of a shoulder evaluation?
Which symptom is often assessed during the physical examination for rotator cuff conditions?
Which symptom is often assessed during the physical examination for rotator cuff conditions?
What is the most common cause of referred pain to the shoulder?
What is the most common cause of referred pain to the shoulder?
Which of the following age groups has the highest prevalence of symptomatic rotator cuff disorders?
Which of the following age groups has the highest prevalence of symptomatic rotator cuff disorders?
When assessing shoulder pain, which symptom would most likely indicate intrinsic causes?
When assessing shoulder pain, which symptom would most likely indicate intrinsic causes?
What percentage range of adults experience shoulder pain at any given time?
What percentage range of adults experience shoulder pain at any given time?
What initial step should be taken when assessing shoulder pain?
What initial step should be taken when assessing shoulder pain?
Which condition is classified as an extrinsic cause of shoulder pain?
Which condition is classified as an extrinsic cause of shoulder pain?
Which factor is least associated with the onset of common shoulder conditions?
Which factor is least associated with the onset of common shoulder conditions?
Which of the following is NOT part of the diagnostic approach for shoulder conditions?
Which of the following is NOT part of the diagnostic approach for shoulder conditions?
What is the initial response of the rotator cuff tendons to load and activity?
What is the initial response of the rotator cuff tendons to load and activity?
What percentage of the population was found to have partial rotator cuff tears?
What percentage of the population was found to have partial rotator cuff tears?
Which of the following changes is NOT part of the progression to degenerative tendinopathy?
Which of the following changes is NOT part of the progression to degenerative tendinopathy?
What is the recommended treatment approach for partial tears larger than 50%?
What is the recommended treatment approach for partial tears larger than 50%?
Which histological change signifies the transition from reactive tendinopathy to degenerative tendinopathy?
Which histological change signifies the transition from reactive tendinopathy to degenerative tendinopathy?
What diagnostic feature can create confusion when assessing for a complete rotator cuff tear?
What diagnostic feature can create confusion when assessing for a complete rotator cuff tear?
Which clinical finding may indicate a potential tear in the rotator cuff?
Which clinical finding may indicate a potential tear in the rotator cuff?
What condition is associated with the degeneration and increased risk of rotator cuff tears?
What condition is associated with the degeneration and increased risk of rotator cuff tears?
What is considered the gold standard imaging technique for evaluating a suspected labral tear or shoulder instability?
What is considered the gold standard imaging technique for evaluating a suspected labral tear or shoulder instability?
Which of the following conditions is most likely to occur as a progression of untreated supraspinatus tendonitis?
Which of the following conditions is most likely to occur as a progression of untreated supraspinatus tendonitis?
What imaging method can be used when there are contraindications to MRI or when a patient is claustrophobic?
What imaging method can be used when there are contraindications to MRI or when a patient is claustrophobic?
What is a common outcome for large rotator cuff tears if not referred to a specialist?
What is a common outcome for large rotator cuff tears if not referred to a specialist?
In evaluating shoulder pain prognosis, which factor indicates a potentially chronic condition?
In evaluating shoulder pain prognosis, which factor indicates a potentially chronic condition?
What term describes changes that often go unnoticed until a rotator cuff tear has been present for some time?
What term describes changes that often go unnoticed until a rotator cuff tear has been present for some time?
Which imaging characteristic is most indicative of fatty atrophy of the supraspinatus?
Which imaging characteristic is most indicative of fatty atrophy of the supraspinatus?
What is a known side effect of chronic rotator cuff tears if left untreated?
What is a known side effect of chronic rotator cuff tears if left untreated?
What is a common cause of axillary nerve denervation in older patients?
What is a common cause of axillary nerve denervation in older patients?
Which condition is associated with fatty atrophy in chronic phases?
Which condition is associated with fatty atrophy in chronic phases?
What is a key difference between biceps tenotomy and tenodesis?
What is a key difference between biceps tenotomy and tenodesis?
What is a likely complication of a paralabral cyst in the shoulder?
What is a likely complication of a paralabral cyst in the shoulder?
What feature is indicative of a proximal biceps rupture?
What feature is indicative of a proximal biceps rupture?
Which factor is NOT a risk factor for proximal biceps rupture?
Which factor is NOT a risk factor for proximal biceps rupture?
What degree of displacement is characterized by isolated greater tuberosity fractures?
What degree of displacement is characterized by isolated greater tuberosity fractures?
Which MRI finding indicates chronic changes associated with nerve injury?
Which MRI finding indicates chronic changes associated with nerve injury?
Flashcards are hidden until you start studying
Study Notes
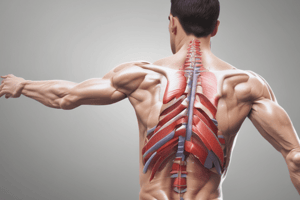
Rotator Cuff Injuries
- Rotator cuff tears are common, with partial tears occurring in 20% and full-thickness tears in 15% of the population.
- Rotator cuff tendinopathy is a progressive condition caused by repetitive stress, leading to structural changes in the tendons.
- The tendons undergo histological changes including:
- Reactive tendinopathy
- Tendon disrepair
- Degenerative tendinopathy
- Tendon rupture
- Initial stages are reversible but progression to degeneration and rupture occurs when the tissue's repair capacity is exceeded.
- Early signs of tendinopathy are disorganized extracellular matrix, subtle inflammation, and peritendinitis visible on imaging.
- Advanced tendinopathy involves changes such as:
- Mucoid degeneration
- Chondral metaplasia
- Amyloid deposition
- Increased fibroblastic cells
- Neovascularization
- These changes are precursors to tendon tears.
Partial Rotator Cuff Tears
- Inability to heal leads to partial tears, which decrease the tendon's mechanical properties.
- Tears greater than 50% are more likely to progress to full thickness tears.
- Tears less than 50% are often treated conservatively, surgery is only recommended if conservative measures fail.
- Clinically assessing partial tears can be challenging and requires imaging confirmation with ultrasound or MRI.
- Drop Arm test can be positive in both tears and inflamed tendons. This may lead to misdiagnosis.
- Early non-surgical interventions for patients with rotator cuff tendonitis may improve prognosis.
Prognosis
- Partial rotator cuff tears may heal with non-operative treatment.
- Physical therapy and muscle strengthening are recommended for most partial tears.
- 40% of partial tears progress to full-thickness tears within 2 years.
- Physical therapy can compensate for strength loss and has a high success rate for chronic tears.
- Full-thickness tears do not heal well and tend to increase in size over time.
- 49% of full-thickness tears increase in size over an average of 2.8 years.
- Larger tears are associated with worsening pain.
- Fatty infiltration is a degenerative process where muscle is replaced by fat following injury.
- Fatty infiltration progresses in full-thickness tears and is a negative prognostic factor for surgical success.
- Fatty infiltration is irreversible, surgery is usually performed when infiltration is minimal.
- Most young, active patients with acute, full-thickness tears should receive operative fixation.
- Full-thickness subscapularis tendon tears require surgical repair to prevent premature osteoarthritis.
- Physical therapy can be successful for atraumatic degenerative rotator cuff tears, with success rates as high as 70%.
- Long-term (10-year) studies show surgical repair provides better outcomes than physical therapy alone.
Differential Diagnosis
- Rotator cuff tendinopathy should be differentiated from:
- Subacromial impingement
- Rotator cuff tear (partial or full-thickness)
- Bicipital tendonitis
- Glenohumeral arthritis
- Acromioclavicular arthritis
- These conditions can occur concurrently.
- A high-riding humeral head is a potential sign of supraspinatus tendon tear.
Imaging of Rotator Cuff Injuries
- Radiographic views can assess:
- Acromion shape for acromial spurs (associated with increased tear risk).
- Acromioclavicular joint for arthritis and spurs that can cause rotator cuff injuries.
- CT scan is reserved for evaluating fractures, fracture-dislocations, and prosthetic joints.
- MRI is the primary imaging modality for evaluating soft tissues:
- Rotator cuff tendons
- Biceps muscle
- Subacromial and subdeltoid bursae
- MRI has high sensitivity for detecting:
- Subtle fractures
- Acromioclavicular joint changes
- Erosive changes to the distal clavicle
- Early avascular necrosis
- Bone marrow edema
- Muscular atrophy
- Acromion morphology
- Radionuclide bone scans are used for evaluating post-arthroplasty infection or suspected metastases.
Ultrasound vs. MRI
- MRI and ultrasound are effective for detecting full-thickness rotator cuff tears.
- Ultrasound may be better for detecting partial tears and is cost-effective for detecting full-thickness tears.
- Some tears, such as intra-substance rotator cuff tears, are unlikely to be repaired even when detected.
- Not all patients with full-thickness tears require surgery, especially if their symptoms are not severe.
Rotator Cuff Tendinopathy Imaging
- MRI can demonstrate increased tendon thickness in rotator cuff tendinopathy.
- MRI images can depict:
- Delaminating partial tendon rupture with fluid between layers but no disruption of articular side insertion.
- Articular side partial rupture greater than 50% of tendon thickness.
- Bursal side partial rupture affecting less than 50% of tendon thickness.
- Full-thickness tear of the supraspinatus.
Rotator Cuff Pathology
- 20% of asymptomatic shoulders have partial rotator cuff tears
- 15% of asymptomatic shoulders have full-thickness tears
- Tendons undergo progressive histological changes:
- Reactive tendinopathy
- Tendon disrepair
- Degenerative tendinopathy
- Tendon rupture
- Early changes are reversible and can be visualized on high-resolution MR or US
- Degenerative changes are associated with mucoid degeneration, chondral metaplasia, amyloid deposition, fibroblastic cells and neovascularization
- Partial tears can progress to full-thickness tears especially when greater than 50%
- Partial tears are commonly treated conservatively
- Assessing partial tears clinically is challenging, usually requiring imaging such as US or MRI
Clinical Tests for Rotator Cuff Disease
- Drop Arm Test:
- Positive for supraspinatus rotator cuff tear or bicipital tendinitis
- Positive LR = 3.3
- Negative LR = 0.82
- Sensitivity = 24%
- Specificity = 93%
- External Rotation Lag Test:
- Pain and/or weakness suggests infraspinatus involvement (tear/RCD)
- Positive LR = 3.2
- Negative LR = 0.35
- Sensitivity = 73%
- Specificity = 77%
- Internal Rotation Lag Test:
- Inability to hold the hand in internal rotation suggests subscapularis disorder
- Positive LR = 5.6 to 6.2
- Negative LR = 0.04
- Sensitivity = 97%
- Specificity = 83%
- Gerber Lift Off Test:
- Inability to lift the hand away from the back indicates internal rotation deficit
- Positive LR = 1.4-1.5
- Negative LR = 0.63-0.85
- Sensitivity = 34-68%
- Specificity = 50-77%
Composite Tests for Pain and Weakness
- External Rotation Resistance:
- Positive for infraspinatus disorders
- Positive LR = 2.6
- Negative LR = 0.49
- Sensitivity = 63%
- Specificity = 75%
- Full Can Test:
- Assesses lesions of the supraspinatus muscle and tendon
- Resisted Abduction:
- Assesses lesions of the supraspinatus muscle and tendon
- Empty Can (Jobe) Test:
- Assesses lesions of the supraspinatus muscle and tendon
- Patte Test:
- Assesses lesions of the supraspinatus muscle and tendon
Calcified Tendinopathy
- Crystal deposition (CPPD) on the tendon causes inflammation
- Often self-limited and resolves spontaneously
- Different clinical stages:
- Precalcification - clinically silent
- Calcification - crystal deposition occurs, may cause pain
- Resorptive - pain associated with inflammatory reaction
- Post-calcification
- Deposits may migrate to the subacromial bursa or into bone
Adhesive Capsulitis
- Clinical diagnosis based on pain and decreased range of motion, especially external rotation
- MRI findings:
- Axillary capsular thickening and edema (acute)
- Hypervascularization and fibrosis (progressive)
- Coracohumeral ligament thickening
- Subcoracoid fibrosis
- Capsular thickening
- Arthrography: low volume contrast medium and thickening of structures
Nerve Denervation Syndromes
- Suprascapular neuropathy:
- Related to compression of paralabral cyst in superior labrum injury
- Other causes: viral inflammation and overuse
- MRI findings:
- Acute: supraspinatus and infraspinatus muscle edema
- Chronic: fatty atrophy and volume loss
- Axillary nerve denervation:
- Secondary to shoulder dislocation, compression in quadrilateral space, or idiopathic
- MRI role: rule out compression causes and associated injuries
- MRI findings:
- Axillary nerve edema or fatty atrophy (chronic)
Isolated Greater Tuberosity Fractures
- Secondary to direct or indirect trauma or minor trauma in osteoporotic patients
- Treatment depends on displacement:
- Little or no displacement: conservative management
- Significant displacement: surgical intervention
Proximal Biceps Tendon Pathology
- Persistent, debilitating symptoms indicate surgical candidacy
- Surgical options:
- Tenotomy: tendon cut, not reattached
- Tenodesis: damaged section removed, remaining tendon reattached to bone
- Biceps tenotomy may result in "Popeye effect"
Biceps Tendon Rupture
- Etiology:
- Distal biceps rupture: excessive eccentric force during extension from flexion
- Proximal biceps rupture: highly correlated with rotator cuff disease
- Risk factors: age, smoking, obesity, corticosteroid use, overuse
- Rare causes: quinolone use, diabetes, lupus, chronic kidney disease
Acromioclavicular Joint Injury
- Type III:
- Tearing of acromioclavicular and coracoclavicular ligaments
- Clavicle elevation above acromion
- Increased coracoclavicular distance on x-ray
- Management: often non-operative, surgery considered for certain conditions
- Type IV:
- Posterior clavicle displacement into trapezius
- Type V:
- Superior displacement (more than 100%) compared to contralateral side
- Type VI:
- Inferior displacement (subacromial or subcoracoid)
- Rare, typically associated with other injuries
- Requires surgical reduction
Acromioclavicular Joint Injury - Imaging
- X-ray:
- Type III: vertical diastasis, clavicular elevation
- Type V: marked widening of coracoclavicular and AC joint intervals
- Ultrasound:
- Superior clavicle displacement relative to acromion
- Effusion distending the joint
- Superior capsule elevation
- MRI:
- Not always necessary
Infection of joint or soft tissues
- Prevalence in primary care is unknown
- 77% of patients in one study had more than one diagnosis
Causes of extrinsic shoulder pain
- Chest disorders: Myocardial infarction, Angina pectoris, Pericarditis, Aortic dissection, Pulmonary embolism, Pneumothorax, Pneumonia, Pleuritis, Pancoast tumour, Mesothelioma, Mediastinal or lung neoplasm
- Abdominal and pelvic disorders: Splenic infarction, Splenic rupture, Hepatic abscess, Cholecystitis, Hepatic hematoma, Subphrenic abscess, Intra-abdominal hemorrhage, Ruptured abdominal viscus
- Neurological disorders: Cervical radiculopathy, Brachial plexopathy, Entrapment neuropathy, Herpes zoster, Cervical spinal stenosis, Thoracic outlet syndrome
- Esophageal disease: Aneurysm, Peptic ulcer, Pancreatitis, Abdominal neoplasms, Ectopic pregnancy
- Vascular insufficiency: Arteritis, Venous thrombosis
Rotator Cuff Disease
- Tendinopathy, full or partial tendon tears and subacromial bursitis
- Majority of patients improve with non-operative treatment
- Smaller tears are less likely to propagate, larger tears may become irreparable
- Bursal-side tears have a tendency to heal
- Partial articular surface tears are more frequent, they do not heal properly and tend to progress to full-thickness tears
- Insertional tears occur in younger populations and are trauma-related
Full-Thickness Tears
- Extend from the articular side to the bursal side
- Size of the tear, number of tendons affected, retraction and the shape of the tear affect prognosis
- Most tears are found in the supraspinatus, subscapularis tendon tears are also common
- Fat atrophy can significantly affect healing and patient prognosis
Massive Rotator Cuff Tears, Rotator Cuff Arthropathy
- Involvement of two or more tendons or retraction greater than 5cm
- Progressive migration of the humeral head superiorly
- Glenohumeral arthrosis with loss of joint space and inferior humeral osteophytes
- Subchondral cyst formation and ultimately collapse of the humeral head
Etiology and Risk Factors of Rotator Cuff Disease
- Excessive overloading, chronic repetitive injuries
- Instability of the glenohumeral and acromioclavicular joints
- Muscle imbalance
- Adverse anatomical features
- Rotator cuff degeneration with aging
- Ischemia
- Musculoskeletal diseases
- Acute injuries related to falls on an outstretched arm
Clinical Presentation of Rotator Cuff Disease
- Shoulder and arm pain/weakness, especially during overhead activities
- Acromioclavicular joint tenderness and compression tenderness
- Neer impingement sign: Pain reproduced with full passive shoulder flexion
- Painful arc of abduction: Shoulder pain from 60° to 120°
- Hawkins impingement sign: Pain is reproduced with shoulder forward flexed at 90 degrees and maximally internally rotated
- Passive Abduction: Pain reproduced with passive shoulder abduction
- Yocum Test: Pain when the patient elevates the elbow without raising ipsilateral shoulder
Clinical Tests for Rotator Cuff Disease: Strength Tests
- Drop arm test: Immediate pain and patient “drops” the arm as they are unable to lower it slowly
- Dropping Sign: Pain and or weakness in the shoulder when resisting external rotation
- External Rotation Lag Test: Inability of the patient to maintain external rotation
- Internal Rotation Lag Test: Inability of the patient to hold the hand in internal rotation lag position
- Gerber Lift Off Test: Inability of the patient to lift the hand away from their back by internally rotating the arm
Clinical Tests for Rotator Cuff Disease: Composite tests for pain and weakness
- External rotation resistance: Pain or weakness during external rotation
- Full can test: Pain or weakness with arm fully abducted and externally rotated
- Resisted abduction: Pain or weakness with arm abducted against resistance
- Empty can (Jobe): Pain or weakness with arm at 90 degrees abduction and externally rotated
- Patte: Patient abducts shoulder to 90 degrees then internally rotates arm, positive test if patient is unable to maintain position
Biceps Tendon Rupture
- Incidence of distal biceps tendon rupture is around 2.55 per 100,000 patient-years
- Most patients are male and the injury happens during middle age
- Proximal biceps rupture is more common in elderly patients, and its exact incidence is unknown
- Distal biceps ruptures mainly involve the dominant limb
Evaluation of Biceps Tendon Rupture
- Diagnosis is often clinically made, imaging is helpful when the diagnosis is unclear
- Three criteria for diagnosis:
- History of a single traumatic event
- Sudden painful pop whilst the elbow is eccentrically loaded
- Grossly palpable retraction of the biceps muscle belly (reverse popeye deformity)
- Weakness of flexion of the elbow and supination of the forearm
Differential Diagnosis of Biceps Tendon Rupture
- Rotator cuff disease
- Shoulder dislocation/instability
- Impingement syndrome
- Humeral/radial head fracture
Prognosis of Biceps Tendon Rupture
- Proximal biceps rupture patients generally recover with non-operative treatment
- Distal biceps rupture can cause persistent pain and forearm supination weakness
- Timely diagnosis is critical, especially in a young active patient
Acromioclavicular Joint Injury
- Common injury in athletes and young individuals
- Frequently seen in sporting events, car accidents, falls from a bicycle
Shoulder Pain Epidemiology
- Shoulder pain is the third most common musculoskeletal reason for seeking medical care
- Shoulder pain affects between 7% and 26% of adults
- Most shoulder complaints arise from intrinsic causes, involving articular and periarticular structures
- Extrinsic causes involving neurologic disorders or visceral conditions may refer pain to the shoulder
- Cervical spine disease is the most common cause of referred pain to the shoulder
- The prevalence of symptomatic rotator cuff disorders increases with age, occurring in about 2.8% of those older than 30 years and in 15% of those older than 70 years
### Diagnostic Approach to Shoulder Pain
- The first step in assessing shoulder pain is to consider intrinsic versus extrinsic causes
- If the pain is not quite related to shoulder and arm movements then extrinsic causes must not be overlooked
- One study of asymptomatic shoulders detailed that partial rotator cuff tears were present in 20% of the population, and 15% had full-thickness tearing
Tendinopathy
- Rotator cuff tendons experience structural changes over the years due to repetitive contact of the tendons with movements between the acromioclavicular arch and the humeral head and between the joint capsule and the glenoid rim
- Tendons undergo progressive histological changes that start in reactive tendinopathy and continue into tendon disrepair and degenerative tendinopathy and end in tendon rupture
- The capacity of the tissue to repair is often insufficient, leading to degeneration and rupture
- Initially, the changes are reversible, but shift to degeneration and rupture when the capacity of the tissue to repair is not enough
Tendinopathy Histological Changes
- Initially the reaction of the tendon to load, friction, and activity results in small changes with disorganized extracellular matrix and subtle inflammatory reaction around the tendon that can be seen as peritendinitis and focal thickness of the tendon on high-resolution MR or US.
- Progressive histological changes include: mucoid degeneration, chondral metaplasia, and amyloid deposition together with reparative changes and inflammation such as an increase of fibroblastic cells and neovascularization.
- These changes represent degenerative tendinopathy, and they are precursors of tendon tears.
Partial Tears
- The inability to heal and restore the normal histological structure of the tendon leads to partial tear with scar formation that decreases mechanical properties.
- Tears that are bigger than 50% have a higher probability to progress to a full-thickness tear than those that are smaller than 50% of the thickness.
- Tears that are smaller than 50% are usually treated conservatively; surgical treatment is only recommended when conservative measures fail.
Assessment of Partial Tears
- Assessing the shoulder for partial tears in a clinical setting is challenging
- One can infer from an examination that there may be a possibility of a tear, however this can only be confirmed by imaging such as; ultrasound or MRI
- A complete tear is commonly associated with a positive Drop Arm test however this may be positive because of the pain lowering the arm in an intact inflamed tendon without a tear.
- This can create a diagnostic conundrum and be a bit frustrating initially in practice
Clinical Presentation of Rotator Cuff Disorders
- The pain is often felt in the distribution of the deltoid muscle to its insertion at the deltoid tuberosity
- Other symptoms include: night pain, weakness, stiffness, or crepitus heard during shoulder movement
- The presence of pain is not required to diagnose RCD, as a chronic full-thickness rotator cuff tear may present with painless loss of active motion.
Physical Examination of Rotator Cuff Disorders
- Physical examination includes inspection, palpation, range of motion, strength and provocative shoulder tests
- The neck and the elbow should also be examined to exclude the possibility that the shoulder pain is referred from either of these regions
Inspection of Shoulder
- Observing the way the patient moves and carries the shoulder
- The patient should be properly disrobed to permit complete inspection of both shoulders
- Swelling, asymmetry, muscle atrophy, scars, ecchymosis and any venous distention should be noted
- Venous distention may indicate an extrinsic cause for the shoulder pain such as venous thoracic outlet syndrome
- Deformity, such as squaring of the shoulder that occurs with anterior dislocation or a step defect at the AC joint could suggest a diagnosis
- Scapular “winging,” can be associated with shoulder instability and serratus anterior or trapezius dysfunction
- Atrophy of the supraspinatus or infraspinatus should prompt a further work-up for such conditions as rotator cuff tear, suprascapular nerve entrapment or neuropathy
### Palpation of Shoulder
- Palpation should include examination of: Acromioclavicular and sternoclavicular joints, cervical spine and the biceps tendon.
- The anterior/posterior glenohumeral joint, coracoid process, acromion and scapula should also be palpated for any tenderness and deformity.
Range of Motion Testing
- The complex series of articulations of the shoulder (SC/AC joints, glenohumeral joint and the scapulothoracic joint) allows a wide range of motion, therefore the affected extremity should be compared with the unaffected side to determine the patient's normal range
- Active and passive ranges should be assessed
- Shoulder abduction involves the glenohumeral joint and the scapulothoracic articulation
- Glenohumeral motion can be isolated by holding the patient's scapula with one hand while the patient abducts the arm.
### Shoulder Arthrography
- Glenohumeral arthrography was described in 1933 by Oberholzer when he injected air into the shoulder joint to evaluate the structures, including the axillary recess, on a conventional radiograph
- In 1934, Codman had suggested that injecting contrast material into the shoulder joint could demonstrate rupture within the rotator cuff
- The use of iodinated contrast, computed tomography, and magnetic resonance imaging came into use later on
- Currently, MRI is the first-line imaging modality for assessing joints as it has a superior soft-tissue contrast capability
- MR arthrography, or MRA, is the gold standard in evaluating a suspected labral tear or shoulder instability
- CT can be performed if there are contraindications to MRI or the patient is claustrophobic
- The arthrogram can aid in facilitating the identification of ligamentous or tendon injuries, intraarticular "loose" bodies, cartilage or synovial abnormalities, loosening of the joint prosthesis, and sinus tracts.
### Prognosis of Shoulder Pain
- The prognosis of shoulder pain depends on the nature of the specific problem
- Periarticular disorders, such as impingement, may be self-limited and respond to rest, analgesics, and range of motion and strengthening exercises
- Impingement syndrome can be chronic and recurrent, leading to rotator cuff tendinopathy
- This can ultimately progress to full-thickness rotator cuff tears and secondary glenohumeral osteoarthritis
- By middle age, asymptomatic rotator cuff tears are common
- Large tears can often lead to loss of abduction and decreased strength and function; these patients should be referred to a specialist
### Prognosis of Rotator Cuff Disorders
- With regards to prognosis, a significant portion of untreated supraspinatus tendonitis may go on to rotator cuff tears
- In some cases, these early changes may be subclinical and may not present until the tear has been present for some time
- A significant portion of rotator cuff defects enlarge and became symptomatic over time
- When there is no compression, there are two main origins: a viral inflammation and or overuse in athletes with overhead activities
- On imaging in the acute phase, supraspinatus and infraspinatus muscle edema is seen, whereas in chronic phases fatty atrophy and volume loss of the muscle are shown
Nerve Denervation Syndromes
- Axillary nerve denervation can be secondary to injury of the axillary nerve in anterior inferior shoulder dislocation, especially in patients older than 40 years of age
- It can also be secondary to compression due to a lesion in the quadrilateral space; or can be idiopathic
- The role of MRI is to rule out compression causes and associated injuries in shoulder dislocation
- MRI will demonstrate axillary nerve edema or fatty atrophy on chronic stages
Isolated Greater Tuberosity Fractures
- Isolated fractures of the greater tuberosity can be secondary to shoulder direct or indirect trauma or in older population to minor trauma in osteoporotic patients
- When there is little or no displacement ( 25% to 50%)
Medial LHB Tendon Subluxation/Dislocation
- Occurs in 6% of patients with shoulder instability
- The LHB tendon insertion is torn or the tendon is subluxed in the bicipital groove
- The majority of these injuries result from recurrent anterior shoulder instability
Prognosis of Biceps Pathology
- Patients with persistent, debilitating symptoms in the setting of known proximal biceps tendon pathology are good surgical candidates for either a tenotomy or tenodesis procedure
- Biceps tenotomy means cutting off one tendon and not reattaching it
- The biceps will still function well after tenotomy, but there may be a change in the appearance of the arm, “Popeye effect”.
- Biceps tenodesis is a procedure where a surgeon removes a damaged section of the biceps and reattaches the rest of the tendon to the bone of the upper arm
Biceps Tendon Rupture
- Distal biceps rupture is from excessive eccentric force as the arm is brought into extension from flexion
- These activities include weightlifting, wrestling, and labor- intensive job
- Proximal biceps rupture is generally not due to a unique mechanism of injury but is highly correlated with rotator cuff disease
- Risk factors include age, smoking, obesity, use of corticosteroids, and overuse
- Rare causes include the use of quinolones, diabetes, lupus, and chronic kidney disease
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.