Podcast
Questions and Answers
Which of the following factors is NOT considered a risk factor for rheumatoid arthritis?
Which of the following factors is NOT considered a risk factor for rheumatoid arthritis?
- PTPN22 gene
- HLA-DRB1 genes
- Smoking
- Regular exercise (correct)
What is a characteristic symptom of rheumatoid arthritis that differentiates it from osteoarthritis?
What is a characteristic symptom of rheumatoid arthritis that differentiates it from osteoarthritis?
- Presence of osteophytes
- Unilateral joint involvement
- Fingers typically involved are the distal joints
- Morning stiffness lasting over 30 minutes (correct)
Which of the following laboratory findings is NOT typically associated with rheumatoid arthritis?
Which of the following laboratory findings is NOT typically associated with rheumatoid arthritis?
- Increased levels of HDL cholesterol (correct)
- Elevated RF
- Positive anti-CCP antibodies
- Low hemoglobin levels
Which type of deformity is characterized by hyperextension of the PIP joints and flexion of the DIP joints?
Which type of deformity is characterized by hyperextension of the PIP joints and flexion of the DIP joints?
What is the primary goal of initiating DMARDs in the treatment of rheumatoid arthritis?
What is the primary goal of initiating DMARDs in the treatment of rheumatoid arthritis?
Which of the following is a common side effect of Methotrexate?
Which of the following is a common side effect of Methotrexate?
What is the most appropriate follow-up frequency for lab work and radiography in a patient on Methotrexate?
What is the most appropriate follow-up frequency for lab work and radiography in a patient on Methotrexate?
Which of the following conditions is contraindicated for Methotrexate therapy?
Which of the following conditions is contraindicated for Methotrexate therapy?
What is a crucial screening test before starting TNF inhibitors?
What is a crucial screening test before starting TNF inhibitors?
Which combination therapy is most commonly used for rheumatoid arthritis treatment?
Which combination therapy is most commonly used for rheumatoid arthritis treatment?
Flashcards are hidden until you start studying
Study Notes
Risk Factors
- HLA-DRB1 genes associated with "shared epitope" increase risk for rheumatoid arthritis (RA)
- PTPN22 gene is another genetic risk factor
- Predominantly affects females, particularly those aged 25-55
- Smoking is identified as a significant lifestyle risk factor
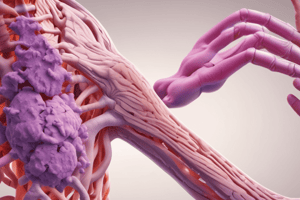
Pathophysiology
- Characterized by pannus formation in synovial tissues, leading to destruction of bones and cartilage
- Insidious onset linked to breakdown of self-tolerance mechanisms
Symptoms
- General: fatigue, weight loss, low-grade fever
- Rheumatoid nodules appear on extensor surfaces
- Vasculitis may occur, along with morning stiffness lasting over 30 minutes, improving with activity and worsening with rest
- Symmetric joint swelling, tenderness, and pain primarily affecting:
- Proximal interphalangeal (PIP) joints
- Metacarpophalangeal (MCP) joints (notable ulnar deviation)
- Metatarsophalangeal (MTP) joints, wrists, ankles, and knees
- Osteoarthritis (OA) differs: less involvement of wrists and feet, affecting only distal joints
Deformities
- Swan neck deformity: hyperextension of PIP joint and flexion of distal interphalangeal (DIP) joint
- Boutonnière deformity: flexion of PIP joint and extension of DIP joint
Systemic Symptoms
- Ocular complications, pulmonary issues, and cardiac involvement (e.g., pericarditis)
Laboratory Findings
- Elevated rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies
- Increased erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)
- Mild anemia and reactive thrombocytosis
- Synovial fluid analysis shows inflammatory effusion with predominant polymorphonuclear leukocytes (PMNs)
Radiographic Findings
- X-rays normal in early RA stages; soft tissue swelling and osteopenia observed initially
- Later stages show joint space narrowing and erosive changes
Diagnostic Criteria
- A score of at least 6 is required for RA diagnosis
Treatment (TX)
- Aim to control pain and inflammation; nonsteroidal anti-inflammatory drugs (NSAIDs) are not sufficient alone as they do not alter disease progression
- Preserve function and prevent deformity development
- Early diagnosis and initiation of disease-modifying anti-rheumatic drugs (DMARDs) are essential
- Corticosteroids used as a bridging treatment, taper as soon as possible, not for monotherapy or long-term use
- Methotrexate (MTX) initiated at 7.5 mg, effects observed in about a month, supplemented with daily folic acid; regular CBC and liver function tests (LFTs) are necessary
- Contraindications for MTX include pregnancy, liver disease, heavy alcohol use, and severe renal impairment, with side effects including GI upset and stomatitis
- Rheumatologist involvement is pivotal; patients may require combined DMARD therapies
- Common combination: MTX with TNF inhibitors
Biologics
- TNF inhibitors (e.g., Etanercept) are effective but come with high costs and risk of severe bacterial and granulomatous infections, including latent TB reactivation
- Screening for latent TB is mandatory prior to starting biologics
Pretreatment Screening
- Conduct comprehensive RA lab panel: RF, anti-CCP, ESR, CRP, CBC, and CMP
- Screen for Hepatitis B & C, perform baseline CBC, creatinine, LFTs, and assess for latent TB
- Conduct ophthalmic screening and rule out pregnancy
- Baseline radiographs to check for osteopenia and erosions
Follow-Up (F/U)
- Regular assessment of symptoms, functional status, lab work, and radiography every two years
Treatment Timeline
- Lifelong MTX therapy (with folic acid) begins with a notice of 4 weeks for noticeable effects
- Begin prednisone dosage of 5-20 mg/day with planned tapering
Felty's Syndrome
- Combination of symptoms including:
- Splenomegaly
- Anemia
- Neutropenia
- Thrombocytopenia
- Arthritis rheumatoid
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.