Podcast
Questions and Answers
What type of condition is Rheumatoid Arthritis?
What type of condition is Rheumatoid Arthritis?
- Metabolic
- Autoimmune (correct)
- Infectious
- Genetic
Which of the following is initially affected in Rheumatoid Arthritis?
Which of the following is initially affected in Rheumatoid Arthritis?
- Muscle tissue
- Bone marrow
- Synovial joint (correct)
- Articular cartilage
What is the main action of Disease-Modifying Antirheumatic Drugs (DMARDs)?
What is the main action of Disease-Modifying Antirheumatic Drugs (DMARDs)?
- Retarding the disease process (correct)
- Treating infections
- Providing immediate pain relief
- Lowering blood pressure
How long can DMARDs typically take to show their effect?
How long can DMARDs typically take to show their effect?
Which of the following is classified as a conventional DMARD?
Which of the following is classified as a conventional DMARD?
What is the primary mechanism of action of Methotrexate?
What is the primary mechanism of action of Methotrexate?
How soon should DMARD treatment start for Rheumatoid Arthritis?
How soon should DMARD treatment start for Rheumatoid Arthritis?
Which drug is commonly considered the drug of choice in early DMARD therapy for Rheumatoid Arthritis?
Which drug is commonly considered the drug of choice in early DMARD therapy for Rheumatoid Arthritis?
What should NSAIDs primarily be used for in the treatment of Rheumatoid Arthritis?
What should NSAIDs primarily be used for in the treatment of Rheumatoid Arthritis?
What is a common side effect associated with Chloroquine and Hydroxychloroquine?
What is a common side effect associated with Chloroquine and Hydroxychloroquine?
What is the main mechanism of action of Azathioprine?
What is the main mechanism of action of Azathioprine?
What is a contraindication (C/I) for Methotrexate?
What is a contraindication (C/I) for Methotrexate?
Which of the following is an example of a TNF$,\alpha$ inhibitor?
Which of the following is an example of a TNF$,\alpha$ inhibitor?
TNF$\alpha$ inhibitors work by binding to?
TNF$\alpha$ inhibitors work by binding to?
A potential side effect associated with TNF$\alpha$ inhibitors is?
A potential side effect associated with TNF$\alpha$ inhibitors is?
What is a common adverse effect of leflunomide?
What is a common adverse effect of leflunomide?
Which of the following is a characteristic of biological DMARDs compared to conventional DMARDs?
Which of the following is a characteristic of biological DMARDs compared to conventional DMARDs?
What kind of drug is Infliximab?
What kind of drug is Infliximab?
Infliximab is a useful treatment for Rheumatoid Arthritis because it acts as?
Infliximab is a useful treatment for Rheumatoid Arthritis because it acts as?
Which drug has tuberculosis(TB) as a possible side effect?
Which drug has tuberculosis(TB) as a possible side effect?
Flashcards
Rheumatoid Arthritis Pathophysiology
Rheumatoid Arthritis Pathophysiology
Autoimmune condition causing synovial joint inflammation, proliferation and articular cartilage destruction.
DMARDs
DMARDs
A class of drugs that retards the disease process and can induce remission in rheumatoid arthritis.
Methotrexate
Methotrexate
Inhibits dihydrofolate reductase, has prominent immunosuppressant and anti-inflammatory properties. It's the first-line drug for RA.
Azathioprine
Azathioprine
Signup and view all the flashcards
Hydroxychloroquine
Hydroxychloroquine
Signup and view all the flashcards
TNFα Inhibitors
TNFα Inhibitors
Signup and view all the flashcards
Infliximab
Infliximab
Signup and view all the flashcards
Azathioprine
Azathioprine
Signup and view all the flashcards
Study Notes
- Drugs Used in Management of Rheumatoid Arthritis provided by Patson Kalunga (Dr. Kaluson)
Clinical Sense
- A Rheumatoid arthritis patient experiences worsening of symptoms and progressive destruction in the joints of several fingers.
- The patient is on methotrexate and another second-line agent for rheumatoid arthritis was considered.
- Etanercept is a parenterally administered DMARD whose mechanism of anti-inflammatory action is antagonism of tumor necrosis factor.
Pathophysiology
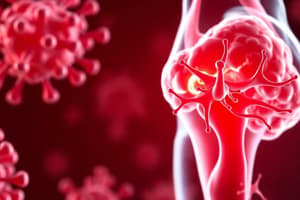
- Rheumatoid arthritis is an autoimmune condition causing inflammation of the synovial joint, synovial proliferation, and articular cartilage destruction.
- Untreated, it causes disability and loss of function.
- Chronic inflammation can lead to higher risk of CVS disease, osteoporosis and certain cancers (e.g., lymphoma).
- TNFa and IL-1 have a major role in the disease process.
Drug Classes Used
- Disease Modifying Antirheumatic Drugs (DMARDs) retard the disease process and can bring about remission and can take up to 6 months to bring about an effect.
- DMARDs can be conventional (nonbiological) or biological.
- Conventional DMARDs: Immunosuppressants like Methotrexate, Azathioprine, Cyclosporine, Sulfasalazine, Chloroquine or Hydroxychloroquine and Leflunomide.
- Biological DMARDs: TNFa inhibitors like Etanercept and Infliximab.
- IL-1 antagonists include Anakinra.
- IL-6 receptor antagonists: tocilizumab, sarilumab.
- T-cell costimulation blocker: abatacept.
- B cell deplete monoclonal antibody: Rituximab.
- JAX inhibitors: Tofacitinib.
- Adjuvant drugs do not modify the disease process but provide supportive treatment like NSAIDs (Nonsteroidal anti-inflammatory drugs) and Glucocorticoids.
Approach in Management
- The 2022 recommendations of the European Alliance of Associations for Rheumatology recommend an early start of a DMARD or combination of DMARD.
- Methotrexate is the drug of choice as first line of treatment.
- Second line includes the other conventional DMARDs (Sulfasalazine etc.) or a TNFa inhibitor.
- NSAIDs and glucocorticoids are mostly used in the initiate stages for symptomatic relief as DMARD is taking effect. Never use as primary treatment drugs.
Methotrexate
- Methotrexate is a dihydrofolate reductase inhibitor, having immunosuppressant and anti-inflammatory properties, reducing cytokine production, chemotaxis, and cell-mediated response.
- Methotrexate is the first-line drug in RA management, and it takes 4-6 weeks to work.
- Side effects include Oral ulceration, GI upset, Liver damage and cirrhosis (long term) and increased incidence of infection (especially chest).
- Contraindications: Pregnancy, breastfeeding mothers, liver disease, active infection, peptic ulcers, leucopeci.
- Azathioprine works as a purine synthase inhibitor, selectively suppressing T-cells and NK cells, reducing inflammation.
Other Conventional DMARDs
- Sulfasalazine: Sulfapyridine (active metabolite) decreases B-cell functions; 5-ASA possibly inhibits COX.
- Side effects: Hemolysis in G6PD deficiency, rash, gastrointestinal disturbance, dizziness, headache, leukopenia.
- Chloroquine and hydroxychloroquine (antimalarial drugs): MOA: Monocyte IL-1 inhibiting B-lymphocytes.
- Side effects: accumulation in melanin containing tissue like the retina leading to retinal damage and corneal ulceration.
- Other side effects: rashes, graying of hair, irritable bowel syndrome, myopathy, and neuropathy.
- Leflunomide decreases proliferation of stimulated lymphocytes.
- ADRs: leflunomide includes diarrhoea, headache, nausea, rashes, loss of hair, thrombocytopenia, leucopenia, increased chances of chest infection, and raised hepatic transaminases
- Contraindications: in pregnancy.
Gold
- Sodium aurothiomalate (gold salts thiomalic acid).
- MOA is not well known but can arrest progression of RA.
- Now obsolete due to high toxicity: (hypertension, dermatitis, stomatitis, kidney/ liver/bone marrow damage).
TNFa Inhibitors
- Can either be soluble TNFa or TNF antibodies which can bind TNF.
- They work mainly by suppression of macrophages and reduction of T cell function and inflammation.
- They have quicker response than conventional DMARDs.
- Etanercept: TNF receptor + Fc portion of IgG.
- Infliximab: monoclonal TNF antibody.
- Adalimumab: anti-TNF antibody.
- Side effects include increased infection risk, malignancy and hepatotoxicity.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.