Podcast
Questions and Answers
What is the primary characteristic of Rheumatoid Arthritis (RA) in terms of its course?
What is the primary characteristic of Rheumatoid Arthritis (RA) in terms of its course?
- It's a degenerative condition that causes gradual breakdown of cartilage only, without inflammation.
- It is characterized by constant, relentless progression.
- It is a rapidly progressing, acute disease.
- It exhibits periods of remission where symptoms lessen, followed by periods of exacerbation where symptoms worsen. (correct)
Which of the following is considered an extra-articular manifestation of RA?
Which of the following is considered an extra-articular manifestation of RA?
- Cartilage erosion
- Joint stiffness
- Fatigue (correct)
- Joint pain and swelling
Which of the following statements accurately describes the etiology of RA?
Which of the following statements accurately describes the etiology of RA?
- RA is caused by a specific bacterial infection.
- RA is caused by a known viral infection.
- The exact cause of RA is unknown, but an autoimmune reaction is widely accepted as a primary factor. (correct)
- RA is caused by a genetic predisposition alone.
What is the primary role of rheumatoid factor in the development of RA?
What is the primary role of rheumatoid factor in the development of RA?
What is 'pannus' and its role in RA?
What is 'pannus' and its role in RA?
What is the significance of the 'Stage 1 - Early' classification of RA in terms of joint changes?
What is the significance of the 'Stage 1 - Early' classification of RA in terms of joint changes?
Which of the following is NOT a characteristic finding in a Stage III - Severe RA case based on x-ray findings?
Which of the following is NOT a characteristic finding in a Stage III - Severe RA case based on x-ray findings?
What is 'ankylosis' in relation to RA?
What is 'ankylosis' in relation to RA?
Which of the following is NOT a common criterion used to diagnose RA?
Which of the following is NOT a common criterion used to diagnose RA?
Which of the following is NOT a common nursing diagnosis for patients with rheumatoid arthritis, psoriatic arthritis, or gout?
Which of the following is NOT a common nursing diagnosis for patients with rheumatoid arthritis, psoriatic arthritis, or gout?
A patient with gout is experiencing pain in their big toe. What type of treatment would be MOST appropriate to address this symptom?
A patient with gout is experiencing pain in their big toe. What type of treatment would be MOST appropriate to address this symptom?
What is the main distinction between primary and secondary gout?
What is the main distinction between primary and secondary gout?
Which of the following is a potential complication associated with long-term corticosteroid therapy for gout?
Which of the following is a potential complication associated with long-term corticosteroid therapy for gout?
What is the PRIMARY goal of nursing management for patients with rheumatoid arthritis, psoriatic arthritis, or gout?
What is the PRIMARY goal of nursing management for patients with rheumatoid arthritis, psoriatic arthritis, or gout?
Which of the following therapeutic approaches is NOT specifically indicated for managing rheumatoid arthritis, psoriatic arthritis, or gout?
Which of the following therapeutic approaches is NOT specifically indicated for managing rheumatoid arthritis, psoriatic arthritis, or gout?
What is the primary goal of joint protection techniques in patients with rheumatoid arthritis, psoriatic arthritis, or gout?
What is the primary goal of joint protection techniques in patients with rheumatoid arthritis, psoriatic arthritis, or gout?
Which of the following is an appropriate intervention for a patient with rheumatoid arthritis who is experiencing difficulties with self-care due to impaired mobility?
Which of the following is an appropriate intervention for a patient with rheumatoid arthritis who is experiencing difficulties with self-care due to impaired mobility?
What is the rationale for using both hot and cold therapy for patients with rheumatoid arthritis, psoriatic arthritis, or gout?
What is the rationale for using both hot and cold therapy for patients with rheumatoid arthritis, psoriatic arthritis, or gout?
Which of the following is a common concern for older adults with rheumatoid arthritis, psoriatic arthritis, or gout?
Which of the following is a common concern for older adults with rheumatoid arthritis, psoriatic arthritis, or gout?
What is the characteristic symptom that distinguishes Rheumatoid Arthritis from other inflammatory conditions in the early stages?
What is the characteristic symptom that distinguishes Rheumatoid Arthritis from other inflammatory conditions in the early stages?
Which of the following is NOT a common extra-articular manifestation of Rheumatoid Arthritis?
Which of the following is NOT a common extra-articular manifestation of Rheumatoid Arthritis?
What is the main characteristic feature of Stage IV Rheumatoid Arthritis?
What is the main characteristic feature of Stage IV Rheumatoid Arthritis?
Which lab test is considered a marker of inflammation and can be elevated in Rheumatoid Arthritis?
Which lab test is considered a marker of inflammation and can be elevated in Rheumatoid Arthritis?
What is the most accurate blood test used to screen for latent tuberculosis (TB) before initiating biologic therapies for Rheumatoid Arthritis?
What is the most accurate blood test used to screen for latent tuberculosis (TB) before initiating biologic therapies for Rheumatoid Arthritis?
Which of the following is NOT a treatment goal for Rheumatoid Arthritis?
Which of the following is NOT a treatment goal for Rheumatoid Arthritis?
Which drug category is specifically designed to target the molecules causing inflammation in Rheumatoid Arthritis?
Which drug category is specifically designed to target the molecules causing inflammation in Rheumatoid Arthritis?
What is a common clinical manifestation of Psoriatic Arthritis that involves the fingers?
What is a common clinical manifestation of Psoriatic Arthritis that involves the fingers?
What is the primary cause for the eventual development of Psoriatic Arthritis?
What is the primary cause for the eventual development of Psoriatic Arthritis?
Which of the following are major signs and symptoms commonly associated with Psoriatic Arthritis?
Which of the following are major signs and symptoms commonly associated with Psoriatic Arthritis?
What is the term for the inflammation that occurs at the point where tendons, ligaments, or joint capsules attach to bones, which is commonly seen in Psoriatic Arthritis?
What is the term for the inflammation that occurs at the point where tendons, ligaments, or joint capsules attach to bones, which is commonly seen in Psoriatic Arthritis?
What is the underlying pathology of Psoriatic Arthritis?
What is the underlying pathology of Psoriatic Arthritis?
Which of the following is NOT a characteristic of the Pathophysiology of Psoriatic Arthritis?
Which of the following is NOT a characteristic of the Pathophysiology of Psoriatic Arthritis?
What is the potential result of untreated Psoriatic Arthritis, affecting the quality of life and overall health of patients?
What is the potential result of untreated Psoriatic Arthritis, affecting the quality of life and overall health of patients?
Which of the following is a common factor contributing to the development of Psoriatic Arthritis?
Which of the following is a common factor contributing to the development of Psoriatic Arthritis?
What is the typical age of onset for Psoriatic Arthritis?
What is the typical age of onset for Psoriatic Arthritis?
Flashcards
Rheumatoid Arthritis
Rheumatoid Arthritis
A chronic autoimmune disorder causing joint inflammation.
Clinical Manifestations
Clinical Manifestations
Symptoms observed in a patient with rheumatoid arthritis.
Morning Stiffness
Morning Stiffness
Stiffness lasting 60+ minutes after waking.
Extraarticular Manifestations
Extraarticular Manifestations
Signup and view all the flashcards
C-Reactive Protein (CRP)
C-Reactive Protein (CRP)
Signup and view all the flashcards
NSAIDs
NSAIDs
Signup and view all the flashcards
Disease-modifying Antirheumatic Drugs (DMARDs)
Disease-modifying Antirheumatic Drugs (DMARDs)
Signup and view all the flashcards
Psoriatic Arthritis (PsA)
Psoriatic Arthritis (PsA)
Signup and view all the flashcards
Dactylitis
Dactylitis
Signup and view all the flashcards
Enthesitis
Enthesitis
Signup and view all the flashcards
Pathophysiology of PsA
Pathophysiology of PsA
Signup and view all the flashcards
Biologics
Biologics
Signup and view all the flashcards
Fatigue in RA
Fatigue in RA
Signup and view all the flashcards
Joint Damage
Joint Damage
Signup and view all the flashcards
Generalized Stiffness
Generalized Stiffness
Signup and view all the flashcards
Gout
Gout
Signup and view all the flashcards
Acute gouty arthritis
Acute gouty arthritis
Signup and view all the flashcards
Tophi
Tophi
Signup and view all the flashcards
Primary gout
Primary gout
Signup and view all the flashcards
Secondary gout
Secondary gout
Signup and view all the flashcards
Hyperuricemia
Hyperuricemia
Signup and view all the flashcards
Uric acid kidney stones
Uric acid kidney stones
Signup and view all the flashcards
Nursing Diagnoses for Gout
Nursing Diagnoses for Gout
Signup and view all the flashcards
Joint protection
Joint protection
Signup and view all the flashcards
Heat and Cold Therapy
Heat and Cold Therapy
Signup and view all the flashcards
Rheumatoid Arthritis (RA)
Rheumatoid Arthritis (RA)
Signup and view all the flashcards
Joint Stiffness
Joint Stiffness
Signup and view all the flashcards
Criteria for RA Diagnosis
Criteria for RA Diagnosis
Signup and view all the flashcards
Rheumatoid Factor
Rheumatoid Factor
Signup and view all the flashcards
Pannus
Pannus
Signup and view all the flashcards
Joint Deformities
Joint Deformities
Signup and view all the flashcards
Stages of RA
Stages of RA
Signup and view all the flashcards
Subluxation
Subluxation
Signup and view all the flashcards
Etiology of RA
Etiology of RA
Signup and view all the flashcards
Study Notes
Rheumatoid, Psoriatic Arthritis & Gout
- Rheumatoid Arthritis (RA), Psoriatic Arthritis, and Gout are presented as distinct conditions. Each has unique symptoms and characteristics.
- A key learning objective is recognizing the symptoms and characteristics of RA, psoriatic arthritis, and gout.
- Learning objectives also include comparing and contrasting pharmacological therapies for these conditions as well as designing individualized nursing care and monitoring plans for patients.
- Understanding the etiology (cause), socioeconomic burden, and psychosocial impact of these conditions is important, along with early detection for effective treatment.
Rheumatoid Arthritis (RA)
- RA is a chronic, systemic disease affecting connective tissue in diarthrodial (synovial) joints.
- Periods of remission (having the disease but it is not active) and exacerbation (symptoms worsen) occur.
- Extraarticular manifestations (symptoms outside the joint) occur. Subjective and objective symptoms are crucial for identifying and monitoring.
- Subjective symptoms include: fatigue and pain
- Objective symptoms include: anorexia, weight loss, low-grade fever, and anemia.
- Key criteria for RA, include: morning stiffness (at least 1 hour for 6 weeks), swelling of 3+ joints for at least 6 weeks, swelling at the wrist, metacarpophalangeal and proximal interphalangeal joints, systemic joint swelling, and hand X-ray changes. Rheumatoid nodules and serum rheumatoid factor are included.
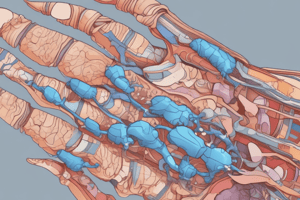
Results of Progressive Joint Destruction
- RA can lead to subluxation, instability, and limitation of movement in the joints.
- Subluxation is the dislocation of the joint, misalignment of the bone ends.
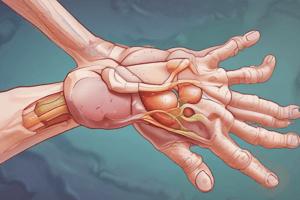
Rheumatoid Arthritis (RA) Etiology & Pathophysiology
-
The cause of RA is currently unknown. A widely accepted theory proposes the involvement of an abnormal immune response. More specifically, abnormal/foreign antigen/Immunoglobulin G (IgG), plus the presence of autoantibodies like rheumatoid factor are considered key findings.
-
IgG and rheumatoid factor form deposits on synovial membranes and articular cartilage.
-
Inflammation results in pannus (granulation tissue at joint margins), leading to destruction of articular cartilage.
-
Genetic predisposition may play a role, notably human leukocyte antigen (HLA).
Rheumatoid Arthritis Joint Deformities
- Joint deformities associated with RA include boutonniere deformity of the thumb, ulnar deviation of metacarpophalangeal joints, and swan-neck deformity of fingers.
Rheumatoid Arthritis Anatomic 4 Stages
- Stage 1 (Early): No destructive changes on X-ray, possible osteoporosis.
- Stage II (Moderate): X-ray evidence of bone loss but no joint deformity. Extra-articular soft tissue lesions are possible.
- Stage III (Severe): X-ray evidence of cartilage and bone destruction. Joint deformity, subluxation, ulnar deviation, hyperextension, bony ankylosis.
- Stage IV (Terminal): Fibrous or bony ankylosis (fusion of joints).
Rheumatoid Arthritis Clinical Manifestations
- RA symptoms can be insidious (beginning slowly and gradually), displaying as various symptoms. Early symptoms might resemble other ailments.
- Specific symptoms include fatigue, anorexia, weight loss, generalized stiffness, and morning stiffness. Symptoms can last 60+ minutes to several hours, and worsen with progression of the disease.
- Symptoms in joints include stiffness and pain localized to joints, edema (swelling), limited motion, inflammation warm to touch and spindle-shaped fingers.
Rheumatoid Arthritis Extraarticular Manifestations
- Extraarticular manifestations include Sjogren's syndrome (decreased tear & saliva production, dry eyes and mouth), Raynaud's phenomenon (color change in digits responding to cold or stress), valvular lesions / pericarditis, interstitial pulmonary fibrosis/pleuritis (lung pathology), lymphadenopathy (enlarged lymph nodes), peripheral neuropathy and edema (including an increased fall risk), and myositis (muscle inflammation).
Rheumatoid Arthritis Clinical Manifestations (Effects on Body)
- Several systemic effects are associated with RA. Examples include: anemia, hardened arteries, heart attack, scarred lungs, lung nodules, rashes, skin nodules, delayed wound healing, and constipation problems
Rheumatoid Arthritis Diagnostic Studies
- Diagnostic tests may include rheumatoid factor (present in 80%), erythrocyte sedimentation rate (ESR), and WBCs. Synovial biopsy (examining joint tissue) and Bone scans (locating areas of increased bone activity), are used.
Rheumatoid Arthritis Treatment Goals
- Goals of treatment for RA include reducing pain, minimizing stiffness and swelling, maintaining mobility, and becoming an informed consumer of health care.
Rheumatoid Arthritis Drug Therapy
- Therapy includes NSAIDS, disease-modifying antirheumatic drugs (DMARDs), anti-inflammatory drugs, Plaquenil (hydroxychloroquine-an antimalarial), Methotrexate, gold salt therapy (given by injection), corticosteroids.
- Nutrition (balanced diet) is also important
Rheumatoid Arthritis Drug Therapy (Biologics)
- Additional drug therapy, "Biologics," targets molecules that drive inflammation in RA.
- Before beginning biologics treatment, patients should be tested for latent Tuberculosis (TB) using a Quantiferon Gold test, which is considered the most accurate blood test for TB.
Psoriatic Arthritis (PsA)
- PsA is a chronic inflammatory arthritis that often develops alongside psoriasis.
- PsA causes persistent pain, diminished quality of life and damage to the joints and can cause disability.
Psoriatic Arthritis (PsA) Etiology
- PsA is linked to pre-existing psoriasis or family history of psoriasis; 30% of psoriasis patients develop PsA alongside their psoriasis condition.
- Both males and females are equally likely to develop PsA. It often starts at ages 30 to 50.
Psoriatic Arthritis (PsA) Signs and Symptoms
- Symptoms of PsA include joint pain; reduced quality of life; joint damage and disability.
- PsA frequently presents with low back pain
- Common initial signs include Dactylitis ("sausage digits") and enthesitis(inflammation in the ligaments or tendons).
- Skin and nail changes. In cases with axial PsA, there could be asymmetric sacroiliitis or spondylitis, associated with lower back pain. Spinal changes occur such as fusion of the vertebrae.
Psoriatic Arthritis (PsA) Pathophysiology
- The exact details of PsA pathophysiology are not completely understood but involves an autoimmune reaction.
- A hallmark feature is an autoimmune response that activates T-cells in the immune system; these lead to the development of inflammatory cytokines and mediators which can erode joints, surrounding tissue, and cause reactive bony growth.
Psoriatic Arthritis (PsA) Treatment
- Treatment options for PsA might include physical therapy, hot/cold compresses, and topical steroids.
Gout
- Gout is a condition characterized by an accumulation of uric acid crystals in the joints and surrounding tissues, causing inflammation and pain.
- Elevated uric acid levels (> 6.8 mg/dL) are a crucial indicator of possible gout.
Gout Symptoms
- Key features of acute gout include attacks of severe articular and peri-articular inflammation.
- Tophi (a build-up of urate crystals) develop in articular surfaces, other soft tissues, and cartilage. Gout may cause complications such as gouty nephropathy, renal impairment, and uric acid kidney stones.
Types of Gout
- Primary gout is when the cause of the disorder is unknown or due to a metabolic error.
- Secondary gout is when the cause of the hyperuricemia is known, but gout itself isn't the main disorder being diagnosed.
Gout Treatment
- Gout treatment aims at preventing and stopping attacks, reducing hyperuricemia, and inhibiting further precipitation of sodium urate crystals. Therapies include medications, absorption of urate crystal deposits in tissues, and other supportive measures.
Nursing Diagnoses for conditions
- Possible diagnoses for individuals with the previously discussed conditions include chronic pain related to inflammation, impaired physical mobility, and a disturbed body image related to chronic illness.
- Ineffective therapy management and self-care deficits related to the disease may also arise.
Nursing Management Goals
- Satisfactory pain relief, minimal loss of functional ability in affected joints, patient participation in planning and managing therapies are important nursing goals for people with these arthritic conditions. A positive self-image and self-care capability are important too.
Treatment for all conditions
- Rest and activity alternation, energy conservation and joint protection with bracing, heat/cold therapy to relieve stiffness and pain of muscles, and individual exercises/aquatic therapy are helpful recommendations.
Gerontologic Considerations
- Considerations for geriatric patients with these conditions include medication sensitivities (especially with NSAIDs and corticosteroids), GI issues related to medication use, corticosteroid therapy side effects (such as osteopenia, increased risk of bone fractures), and addressing challenges to self-care and decision-making in older populations along with issues pertaining to assisted living and care.
Practice Questions:
- Diagnostic tests for suspected RA include rheumatoid factor, erythrocyte sedimentation rate (ESR), x-ray imaging, and evaluation of other relevant markers.
- Rheumatoid arthritis distinguishes itself from osteoarthritis via its effect on other body systems.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.