Podcast
Questions and Answers
What mechanism allows for efficient oxygenation of blood in gills?
What mechanism allows for efficient oxygenation of blood in gills?
- Lateral flow
- Counter current flow (correct)
- Parallel flow
- Globular flow
What unique feature of birds allows for continuous gas exchange during expiration?
What unique feature of birds allows for continuous gas exchange during expiration?
- Air sacs and parabronchi (correct)
- Lungs with alveoli
- Pneumatized bones
- Diaphragm and ribcage
At what altitude does the partial pressure of oxygen drop to nearly half of that at sea level?
At what altitude does the partial pressure of oxygen drop to nearly half of that at sea level?
- 6000 m (correct)
- 3000 m
- 4000 m
- 5000 m
Which center in the brain controls the rate and depth of breathing?
Which center in the brain controls the rate and depth of breathing?
What substance is released as a byproduct during the oxidation of food materials such as glucose?
What substance is released as a byproduct during the oxidation of food materials such as glucose?
Which type of animal supplies oxygen directly to each cell through a system of tracheae?
Which type of animal supplies oxygen directly to each cell through a system of tracheae?
What typically forces a human to breathe after holding their breath?
What typically forces a human to breathe after holding their breath?
What component found in the muscles of certain aquatic mammals increases their affinity for oxygen?
What component found in the muscles of certain aquatic mammals increases their affinity for oxygen?
What is the primary cause of asbestosis?
What is the primary cause of asbestosis?
Which disorder is caused by long term exposure to silica dust?
Which disorder is caused by long term exposure to silica dust?
What is a possible outcome of inhaling iron particles over time?
What is a possible outcome of inhaling iron particles over time?
Which respiratory disorder is commonly associated with coal mining?
Which respiratory disorder is commonly associated with coal mining?
Which of the following statements best describes siderosis?
Which of the following statements best describes siderosis?
What is the main purpose of the respiratory process known as breathing?
What is the main purpose of the respiratory process known as breathing?
Which of the following best describes anaerobic respiration?
Which of the following best describes anaerobic respiration?
Where does the process of internal respiration take place?
Where does the process of internal respiration take place?
Which structure in the human respiratory system is primarily responsible for sound production?
Which structure in the human respiratory system is primarily responsible for sound production?
How do aquatic arthropods primarily exchange gases?
How do aquatic arthropods primarily exchange gases?
What is the function of the nasal chambers in the human respiratory system?
What is the function of the nasal chambers in the human respiratory system?
What structure prevents food from entering the larynx during swallowing?
What structure prevents food from entering the larynx during swallowing?
What characterizes the respiratory system of mammals?
What characterizes the respiratory system of mammals?
Which of the following statements is true regarding the bronchi and bronchioles?
Which of the following statements is true regarding the bronchi and bronchioles?
What is the main cellular outcome of aerobic respiration?
What is the main cellular outcome of aerobic respiration?
Which part of the larynx is responsible for producing a high pitch sound?
Which part of the larynx is responsible for producing a high pitch sound?
What is the role of the pleural fluid in the lungs?
What is the role of the pleural fluid in the lungs?
What type of respiration do yeast undergo in the absence of oxygen?
What type of respiration do yeast undergo in the absence of oxygen?
Which component prevents the trachea from collapsing?
Which component prevents the trachea from collapsing?
What is the primary mechanism for oxygen transport in red blood cells?
What is the primary mechanism for oxygen transport in red blood cells?
How much of oxygen is typically delivered to tissues by 100 ml of oxygenated blood?
How much of oxygen is typically delivered to tissues by 100 ml of oxygenated blood?
What change occurs in haemoglobin's affinity for oxygen at low pO2 levels?
What change occurs in haemoglobin's affinity for oxygen at low pO2 levels?
Which factor does NOT influence the binding of oxygen with haemoglobin?
Which factor does NOT influence the binding of oxygen with haemoglobin?
What is the primary form in which carbon dioxide is transported in the blood?
What is the primary form in which carbon dioxide is transported in the blood?
What does the oxyhaemoglobin dissociation curve illustrate?
What does the oxyhaemoglobin dissociation curve illustrate?
Which statement best describes the Bohr Effect?
Which statement best describes the Bohr Effect?
What percentage of carbon dioxide is transported in dissolved form within plasma?
What percentage of carbon dioxide is transported in dissolved form within plasma?
What happens to oxyhaemoglobin in tissues with low pO2?
What happens to oxyhaemoglobin in tissues with low pO2?
What occurs when the pCO2 levels rise in the blood?
What occurs when the pCO2 levels rise in the blood?
Which of the following statements about bicarbonate is true?
Which of the following statements about bicarbonate is true?
During vigorous exercise, what percentage of oxygen may be unloaded to tissues?
During vigorous exercise, what percentage of oxygen may be unloaded to tissues?
What adaptation allows haemoglobin to effectively manage oxygen and carbon dioxide transport?
What adaptation allows haemoglobin to effectively manage oxygen and carbon dioxide transport?
What role does hemoglobin play in buffering H+ ions during gas exchange?
What role does hemoglobin play in buffering H+ ions during gas exchange?
What occurs during the chloride shift in red blood cells?
What occurs during the chloride shift in red blood cells?
Which center in the brain is primarily responsible for regulating respiratory rhythm?
Which center in the brain is primarily responsible for regulating respiratory rhythm?
How does an increase in CO2 and H+ concentration affect breathing?
How does an increase in CO2 and H+ concentration affect breathing?
What is the primary effect of the pneumotaxic center on respiration?
What is the primary effect of the pneumotaxic center on respiration?
What does the residual volume represent in respiratory volumes?
What does the residual volume represent in respiratory volumes?
Which respiratory capacity includes tidal volume and inspiratory reserve volume?
Which respiratory capacity includes tidal volume and inspiratory reserve volume?
What is a primary symptom of asthma?
What is a primary symptom of asthma?
Which of the following is a major cause of emphysema?
Which of the following is a major cause of emphysema?
What is included in the definition of vital capacity?
What is included in the definition of vital capacity?
How does pneumonia affect gas exchange in the lungs?
How does pneumonia affect gas exchange in the lungs?
Which of the following components reflects the normal range of tidal volume?
Which of the following components reflects the normal range of tidal volume?
What is the significance of histidine in hemoglobin's function as a buffer?
What is the significance of histidine in hemoglobin's function as a buffer?
What is the primary function of the conducting part of the respiratory system?
What is the primary function of the conducting part of the respiratory system?
What role does the diaphragm play during inspiration?
What role does the diaphragm play during inspiration?
Which part of the respiratory system is primarily involved in gas exchange?
Which part of the respiratory system is primarily involved in gas exchange?
In which circumstance does expiration primarily occur?
In which circumstance does expiration primarily occur?
What is one factor that affects the rate of gas diffusion across the respiratory membrane?
What is one factor that affects the rate of gas diffusion across the respiratory membrane?
What is primarily responsible for creating pressure gradients necessary for breathing?
What is primarily responsible for creating pressure gradients necessary for breathing?
Which gas has a higher diffusion rate due to greater solubility in the pulmonary membrane?
Which gas has a higher diffusion rate due to greater solubility in the pulmonary membrane?
Which muscles are primarily involved in forced expiration?
Which muscles are primarily involved in forced expiration?
What is the typical respiratory rate for a healthy human adult?
What is the typical respiratory rate for a healthy human adult?
How is the volume of air involved in breathing typically measured?
How is the volume of air involved in breathing typically measured?
What anatomical structure forms the lower boundary of the thoracic cavity?
What anatomical structure forms the lower boundary of the thoracic cavity?
What describes the process of diffusion in the exchange of gases?
What describes the process of diffusion in the exchange of gases?
Which sequence correctly describes the order of respiration steps?
Which sequence correctly describes the order of respiration steps?
What anatomical feature best ensures that the thoracic cavity remains air-tight?
What anatomical feature best ensures that the thoracic cavity remains air-tight?
What process is primarily responsible for releasing energy from food molecules?
What process is primarily responsible for releasing energy from food molecules?
How do insects and some arthropods deliver oxygen to their cells?
How do insects and some arthropods deliver oxygen to their cells?
What role does the diaphragm play in respiration for mammals?
What role does the diaphragm play in respiration for mammals?
What happens to the partial pressure of oxygen as altitude increases?
What happens to the partial pressure of oxygen as altitude increases?
What substance is formed as a harmful byproduct during cellular metabolism?
What substance is formed as a harmful byproduct during cellular metabolism?
What helps control the homeostasis of oxygen and carbon dioxide levels?
What helps control the homeostasis of oxygen and carbon dioxide levels?
What adaptation allows the elephant seal to remain underwater for extended periods?
What adaptation allows the elephant seal to remain underwater for extended periods?
What phenomenon is likely to occur when someone ascends to high altitudes without proper acclimatization?
What phenomenon is likely to occur when someone ascends to high altitudes without proper acclimatization?
What is asbestosis primarily caused by?
What is asbestosis primarily caused by?
Which disorder is associated with long term exposure to silica dust?
Which disorder is associated with long term exposure to silica dust?
Siderosis can cause which of the following disorders?
Siderosis can cause which of the following disorders?
What is the primary cause of black-lung disease?
What is the primary cause of black-lung disease?
Which of the following is NOT a type of siderosis?
Which of the following is NOT a type of siderosis?
What is the primary function of the conducting part of the respiratory system?
What is the primary function of the conducting part of the respiratory system?
Which structure contributes to increasing the thoracic volume during inspiration?
Which structure contributes to increasing the thoracic volume during inspiration?
What drives the process of expiration in the respiratory system?
What drives the process of expiration in the respiratory system?
What factor has the greatest impact on the rate of diffusion of gases across the respiratory membrane?
What factor has the greatest impact on the rate of diffusion of gases across the respiratory membrane?
What entails the diffusion of oxygen from the alveoli to the blood?
What entails the diffusion of oxygen from the alveoli to the blood?
Which component of the respiratory system is primarily responsible for the exchange of gases?
Which component of the respiratory system is primarily responsible for the exchange of gases?
What is the role of the pleural fluid in the respiratory system?
What is the role of the pleural fluid in the respiratory system?
Which factor does NOT influence the binding of oxygen to hemoglobin?
Which factor does NOT influence the binding of oxygen to hemoglobin?
Why is the alveolar wall structure important for gas exchange?
Why is the alveolar wall structure important for gas exchange?
What is the typical respiratory rate of a healthy human at rest?
What is the typical respiratory rate of a healthy human at rest?
What is primarily responsible for the creation of pressure differences that facilitate breathing?
What is primarily responsible for the creation of pressure differences that facilitate breathing?
Which respiratory process is considered an active process?
Which respiratory process is considered an active process?
In what way does carbon dioxide diffusion differ from oxygen diffusion?
In what way does carbon dioxide diffusion differ from oxygen diffusion?
What is the primary distinction between breathing and respiration?
What is the primary distinction between breathing and respiration?
Which structure is responsible for preventing food from entering the trachea?
Which structure is responsible for preventing food from entering the trachea?
Which type of respiration yields the most energy?
Which type of respiration yields the most energy?
What is the role of the trachea in the respiratory system?
What is the role of the trachea in the respiratory system?
How do earthworms primarily exchange gases?
How do earthworms primarily exchange gases?
Which component is NOT part of the structure of the larynx?
Which component is NOT part of the structure of the larynx?
What is the function of the pleural fluid in the lungs?
What is the function of the pleural fluid in the lungs?
Which type of respiration occurs in organisms like yeast in the absence of oxygen?
Which type of respiration occurs in organisms like yeast in the absence of oxygen?
What structure in the respiratory system aids in sound production?
What structure in the respiratory system aids in sound production?
Which respiratory organ is primarily used for gas exchange in aquatic arthropods?
Which respiratory organ is primarily used for gas exchange in aquatic arthropods?
What part of the nasal chambers is responsible for filtering dust particles?
What part of the nasal chambers is responsible for filtering dust particles?
Which type of cartilage is found in the wall of the trachea?
Which type of cartilage is found in the wall of the trachea?
What is the initial structure through which inhaled air enters the human respiratory system?
What is the initial structure through which inhaled air enters the human respiratory system?
During which respiratory phase does gas exchange specifically take place in the lungs?
During which respiratory phase does gas exchange specifically take place in the lungs?
What primarily triggers the regulation of respiratory rhythm?
What primarily triggers the regulation of respiratory rhythm?
Which volume specifically refers to the air remaining in the lungs after forcible expiration?
Which volume specifically refers to the air remaining in the lungs after forcible expiration?
What role does carbon dioxide play in the respiratory process?
What role does carbon dioxide play in the respiratory process?
What is the primary mechanism by which bicarbonate ions move out of red blood cells?
What is the primary mechanism by which bicarbonate ions move out of red blood cells?
Which statement best describes the relationship between hemoglobin and hydrogen ions?
Which statement best describes the relationship between hemoglobin and hydrogen ions?
What is the primary mechanism through which oxygen is transported in the blood?
What is the primary mechanism through which oxygen is transported in the blood?
How does the partial pressure of oxygen (pO2) affect the binding of oxygen to hemoglobin?
How does the partial pressure of oxygen (pO2) affect the binding of oxygen to hemoglobin?
Which respiratory volume can be utilized to gauge lung function and potential disorders?
Which respiratory volume can be utilized to gauge lung function and potential disorders?
What effect does the pneumotaxic center have on breathing?
What effect does the pneumotaxic center have on breathing?
What happens to the oxyhemoglobin in tissues with low pO2 levels?
What happens to the oxyhemoglobin in tissues with low pO2 levels?
Which factor decreases the affinity of hemoglobin for oxygen according to the Bohr Effect?
Which factor decreases the affinity of hemoglobin for oxygen according to the Bohr Effect?
What defines the difference between Chronic Obstructive Pulmonary Diseases (COPDs)?
What defines the difference between Chronic Obstructive Pulmonary Diseases (COPDs)?
What percentage of carbon dioxide is typically transported as bicarbonate in the blood?
What percentage of carbon dioxide is typically transported as bicarbonate in the blood?
How is the connection between the respiratory rhythm center and the chemo-sensitive area significant?
How is the connection between the respiratory rhythm center and the chemo-sensitive area significant?
Which condition favors the formation of oxyhemoglobin in the alveoli?
Which condition favors the formation of oxyhemoglobin in the alveoli?
Which condition is characterized by inflammation and increased mucus production in bronchi?
Which condition is characterized by inflammation and increased mucus production in bronchi?
What does the term 'Inspiratory Capacity' refer to?
What does the term 'Inspiratory Capacity' refer to?
What is the primary way in which carbon dioxide is transported in the blood?
What is the primary way in which carbon dioxide is transported in the blood?
At what partial pressure of oxygen (pO2) is hemoglobin typically around 75% saturated in resting tissues?
At what partial pressure of oxygen (pO2) is hemoglobin typically around 75% saturated in resting tissues?
Which of the following is a characteristic symptom of emphysema?
Which of the following is a characteristic symptom of emphysema?
Which statement accurately describes the oxygen-hemoglobin dissociation curve?
Which statement accurately describes the oxygen-hemoglobin dissociation curve?
Which gas reaction occurs at the alveolar site where pCO2 is low?
Which gas reaction occurs at the alveolar site where pCO2 is low?
Which gas primarily drives the loading and unloading of oxygen in hemoglobin?
Which gas primarily drives the loading and unloading of oxygen in hemoglobin?
What best describes the role of chloride ions during the chloride shift?
What best describes the role of chloride ions during the chloride shift?
What role does hemoglobin serve due to its amphoteric nature?
What role does hemoglobin serve due to its amphoteric nature?
During vigorous exercise, what is the maximum percentage of oxygen that may be unloaded to the tissues?
During vigorous exercise, what is the maximum percentage of oxygen that may be unloaded to the tissues?
What characterizes the blood transport of carbon dioxide as carbamino compounds?
What characterizes the blood transport of carbon dioxide as carbamino compounds?
What impact does a rise in pCO2 have on blood pH?
What impact does a rise in pCO2 have on blood pH?
Flashcards are hidden until you start studying
Study Notes
Respiration: Energy Release and Oxygen Utilization
- Respiration is a catabolic process where energy is released through the oxidation of food.
- Oxygen is used to produce 'metabolic water,' a byproduct of calorie burning.
- 'Counter-current flow' in gills ensures efficient oxygenation of blood.
- Birds have 'air sacs' and 'parabronchi' for continuous gas exchange, even during exhalation.
- 'Tracheate animals' like insects have tracheae and tracheoles to deliver oxygen directly to cells, enabling high activity levels.
- At high altitudes (around 6000m), oxygen levels are significantly reduced, leading to 'mountain sickness'.
- The ribcage and diaphragm aid mammals in breathing more effectively.
- Oxygen and carbon dioxide homeostasis are controlled by the respiratory center.
- Inhalation and exhalation are regulated by the medulla oblongata.
- The pneumotaxic center in the pons controls the rate and depth of breathing.
- Elephant seals can stay submerged for up to two hours due to myoglobin in their muscles, which has a higher affinity for oxygen.
Cellular Respiration
- All living cells require a constant energy supply for metabolic activities.
- Energy is produced by the oxidation of digested micromolecules like glucose, amino acids, and fatty acids.
- These molecules are transported to cells via the circulatory system.
- Oxygen is used by organisms to break down stored food materials (glucose, fatty acids).
- Carbon dioxide (CO2), a byproduct of metabolism, is harmful as it dissolves in water to form carbonic acid, lowering blood pH and disrupting homeostasis.
- The body requires continuous oxygen supply and CO2 removal.
Overview of Respiration
- The process of exchanging oxygen from the environment (air or water) with CO2 produced by cells is called 'breathing.'
- Gaseous exchange, including the entry of oxygen and exit of CO2, is often called 'external respiration' or 'ventilation.'
- The chemical breakdown of food materials to generate energy is referred to as 'respiration.'
- Because this chemical breakdown occurs inside the cells of all organisms, it's known as 'internal respiration' or 'cellular respiration.'
Types of Respiration
- Anaerobic respiration: Incomplete breakdown of organic molecules, yielding less energy. Occurs in the absence of oxygen in organisms like yeast, bacteria, and muscles under certain conditions.
- C6H12O6 → 2CO2 + 2C2H5OH (ethanol) + 2ATP
- C6H12O6 → 2C3H6O3 (lactic acid) + 2ATP
- Aerobic respiration: Complete breakdown of organic molecules, yielding more energy in the presence of oxygen.
- C6H12O6 + 6H2O + 6O2 → 6CO2 + 12H2O + 36ATP
Respiratory Organs in Animals
- Respiration mechanisms vary depending on animal habitat and organization.
- Protozoans and simpler invertebrates (sponges, cnidarians, flatworms) exchange gases through simple diffusion across their body surface.
- Earthworms use their moist body wall.
- Insects have a tracheal system for air transport.
- Spiders and scorpions have 'book lungs' for breathing air.
- Aquatic arthropods and molluscs have gills for gas exchange.
- Terrestrial organisms like reptiles, birds, and mammals breathe using lungs.
- Amphibians like frogs use both moist skin and lungs for respiration.
- Mammals have a well-developed respiratory system.
Human Respiratory System
- Consists of the following structures:
- External Nostrils (External Nares): Openings above the upper lip leading to nasal chambers.
- Nasal Chambers: Located above the palate, separated by a nasal septum. Divided into three parts:
- Vestibular part: Contains hair and sebaceous glands to filter dust.
- Respiratory part: Conditioning inhaled air, supported by turbinals (conchae).
- Olfactory part: Lined with olfactory epithelium for smell detection.
- Naso-pharynx: Connects nasal chambers to the nasopharynx (upper portion of the pharynx).
- Larynx: Cartilaginous box called the voice box.
- Cartilages: Nine cartilages support the larynx:
- Unpaired: Thyroid, cricoid, epiglottis
- Paired: Corniculate (cartilages of Santorini), arytenoids, cuneiform
- Epiglottis: Cartilaginous flap preventing food from entering the larynx.
- Vocal Cords: Elastic fibers connecting thyroid and arytenoid cartilages.
- True vocal cords: Produce sound.
- False vocal cords: Folds of mucous membrane, not involved in sound production.
- Rima glottidis: Narrow opening between vocal cords.
- Laryngeal prominence (Adam's apple): Mid-ventral part of thyroid cartilage.
- Cartilages: Nine cartilages support the larynx:
- Trachea (Windpipe): Straight tube extending to the mid-thoracic cavity.
- C-shaped hyaline cartilage rings: Support the trachea, keeping it open.
- Pseudostratified ciliated epithelium: Lines the trachea internally.
- Bronchi and Bronchioles:
- Primary bronchi: Trachea divides into right and left primary bronchi at the level of the fifth thoracic vertebra.
- Secondary bronchi: Branching of primary bronchi within the lungs.
- Tertiary bronchi: Further branching of secondary bronchi.
- Bronchioles: Repeated divisions of bronchi forming primary, secondary, tertiary, terminal, and respiratory bronchioles.
- Alveolar ducts: Respiratory bronchioles terminate into alveolar ducts.
- Alveolar sacs: Alveolar ducts end in alveolar sacs.
- Incomplete cartilaginous rings: Support bronchi and initial bronchioles.
- Pulmonary tree: Branching network of trachea, bronchi, and bronchioles, resembling an upside-down tree.
- Lungs: Fill the majority of the thoracic cavity.
- Pleura: Double-layered membrane surrounding the lungs, with pleural fluid between them to reduce friction.
- Conducting part: External nostrils to terminal bronchioles, transporting air, clearing particles, humidifying, and warming air.
- Respiratory (exchange part): Alveoli and their ducts, where O2 and CO2 exchange occurs.
- Thoracic chamber: Anatomically airtight chamber containing the lungs.
- Dorsal: Vertebral column.
- Ventral: Sternum.
- Lateral: Ribs.
- Lower: Dome-shaped diaphragm.
- Pulmonary volume: Changes in thoracic chamber volume affect lung volume, essential for breathing.
Steps Involved in Human Respiration
- Breathing or Pulmonary Ventilation: Drawing in atmospheric air (21% O2) and expelling alveolar air (rich in CO2).
- Diffusion of Gases Across the Alveolar Membrane: Exchange of O2 and CO2 between the alveoli and blood.
- Transport of Gases by Blood: Moving gases between lungs and tissues.
- Diffusion of O2 and CO2 Between Blood and Tissues: Gas exchange between blood in systemic capillaries and tissues.
- Utilization of O2 by Cells and CO2 Production: Cellular respiration - cells use O2 for catabolic reactions, producing CO2, H2O, and ATP.
Mechanism of Breathing
- Breathing: Process of maximizing gas exchange by creating a pressure gradient between lungs and atmosphere.
- Inspiration: Active process involving muscle contraction.
- Diaphragm: Contraction increases thoracic chamber volume in the anteroposterior axis.
- External intercostal muscles: Contraction lifts ribs and sternum, increasing thoracic volume in the dorso-ventral axis.
- Increased thoracic volume: Leads to an increase in pulmonary volume, decreasing intra-pulmonary pressure below atmospheric pressure, forcing air into the lungs.
- Expiration: Passive process involving muscle relaxation.
- Diaphragm and external intercostal muscles: Relaxation returns diaphragm and sternum to their normal positions, decreasing thoracic and pulmonary volume.
- Increased intra-pulmonary pressure: Exceeds atmospheric pressure, forcing air out of the lungs.
- Forced expiration: Contraction of internal intercostal muscles and lateral abdominal muscles.
- Average breathing rate: 12-16 breaths per minute.
- Spirometer: Used to measure air volume involved in breathing movements, aiding in the assessment of pulmonary function.
Gas Exchange
- Alveoli: Primary sites of gas exchange in the lungs.
- Simple Diffusion: The exchange of gases is based on simple diffusion, influenced by:
- Partial pressure/concentration gradient: Difference in gas pressures between alveoli and blood, and between blood and tissues.
- Solubility of gases: CO2 is more soluble than O2, facilitating its diffusion.
- Thickness of the respiratory membrane: Thin membrane favors diffusion.
- Surface area: Larger surface area maximizes diffusion.
- Distance of diffusion: Short diffusion distance is beneficial.
- Partial Pressure: Individual gas pressure in a mixture.
- pO2: Partial pressure of oxygen.
- pCO2: Partial pressure of carbon dioxide.
- Gas exchange gradients:
- Alveoli to blood: High pO2 in alveoli drives O2 diffusion into blood.
- Blood to tissues: High pO2 in blood drives O2 diffusion into tissues.
- Tissues to blood: High pCO2 in tissues drives CO2 diffusion into blood.
- Blood to alveoli: High pCO2 in blood drives CO2 diffusion into alveoli.
Transport of Gases
- Blood: Medium for transporting O2 and CO2.
- Transport of Oxygen:
- Plasma: Carries about 3% of O2 in dissolved form.
- Red blood cells (RBCs): Carry about 97% of O2.
- Hemoglobin (Hb): Oxygen-carrying pigment in RBCs.
- Oxyhemoglobin: Hb bound to oxygen, bright red in color.
- Oxygenation of hemoglobin: Hb + 4O2 → Hb(O2)4
- Factors affecting oxygen binding:
- Partial pressure of O2: Higher pO2 at lungs promotes oxygen binding.
- Partial pressure of CO2: Higher pCO2 reduces oxygen affinity.
- Hydrogen ion concentration (pH): Lower pH (higher acidity) reduces oxygen affinity.
- Temperature: Higher temperature reduces oxygen affinity.
- Hemoglobin (Hb): Oxygen-carrying pigment in RBCs.
- Oxygen-Hemoglobin Dissociation Curve: A sigmoid curve showing the relationship between hemoglobin saturation and pO2.
- Shift to the right: Conditions like high pCO2, low pH, and high temperature decrease oxygen affinity and shift the curve to the right.
- Bohr Effect: The effect of pCO2 and H+ concentration on oxygen affinity of hemoglobin.
- Transport of Carbon Dioxide:
- Dissolved state: 7% of CO2 is carried dissolved in plasma.
- Carbamino compounds: 20-25% of CO2 combines with hemoglobin to form carbaminohemoglobin.
- Bicarbonates: About 70% of CO2 is transported as bicarbonate.
- Carbonic anhydrase: Enzyme in RBCs and plasma that facilitates the conversion of CO2 to carbonic acid.
- Hemoglobin: Amphoteric compound, can bind oxygen and release CO2 in oxygen-rich areas, and bind CO2 and release oxygen in CO2-rich areas.
Carbon Dioxide Transport
- Carbon dioxide is transported in the blood as bicarbonate, dissolved in plasma, and bound to haemoglobin.
- At the tissues, high partial pressure of CO2 leads to formation of carbonic acid, which dissociates to bicarbonate and hydrogen ions.
- Bicarbonate diffuses out of red blood cells into the plasma, while hydrogen ions are buffered by haemoglobin.
- This process, known as the chloride shift, involves the exchange of chloride and bicarbonate ions between the red blood cells and plasma to maintain electrolyte balance.
- At the lungs, low partial pressure of CO2 reverses this process.
Regulation of Respiratory Movements
- The respiratory rhythm centre in the medulla controls breathing.
- The pneumotaxic centre in the pons can modify the duration of inspiration and respiratory rate.
- Chemosensitive areas in the medulla are sensitive to changes in CO2 and hydrogen ion concentrations and stimulate the respiratory rhythm centre to adjust breathing.
- Receptors in the aortic arch and carotid artery detect changes in CO2 and H+ levels and send signals to the respiratory rhythm centre and pneumotaxic centre.
Respiratory Volumes and Capacities
- Tidal Volume (TV): The amount of air inhaled or exhaled during normal breathing (approximately 500 ml).
- Inspiratory Reserve Volume (IRV): The additional volume of air that can be inhaled during forced inspiration (about 2500-3000 ml).
- Expiratory Reserve Volume (ERV): The additional volume of air that can be exhaled during forced expiration (about 1000-1100 ml).
- Residual Volume (RV): The volume of air remaining in the lungs after forceful expiration (about 1100-1200 ml).
- Inspiratory Capacity (IC): The total volume of air that can be inhaled after normal expiration (IC = TV + IRV, about 3000-3500 ml).
- Functional Residual Capacity (FRC): The volume of air remaining in the lungs after normal expiration (FRC = ERV + RV).
- Vital Capacity (VC): The maximum volume of air that can be exhaled after a forced inspiration (VC = TV + IRV + ERV).
- Total Lung Capacity (TLC): The total volume of air that can be accommodated in the lungs at the end of a forced inspiration (TLC = VC + RV or TLC = ERV + IRV + TV + RV).
Disorders of the Respiratory System
- Asthma: Difficulty breathing due to inflammation of bronchi and bronchioles, characterized by spasms of smooth muscles in the airway walls. Symptoms include coughing, wheezing, and shortness of breath.
- Emphysema: Chronic disorder where alveolar walls are damaged and respiratory surface area is decreased. Caused by smoking and characterized by fewer, larger alveoli and a more fibrous, less elastic lung.
- Bronchitis: Inflammation of bronchi, leading to swelling of the mucus lining, increased mucus production, and narrowing of airways. Symptoms include chronic cough with thick mucus.
- Pneumonia: Infection of the lungs caused by bacteria, viruses, fungi, protozoans, and mycoplasmas. Symptoms include inflammation of the lungs, accumulation of mucus in alveoli, and impaired gas exchange.
- Emphysema, chronic bronchitis, and asthma fall under Chronic Obstructive Pulmonary Diseases (COPDs).
- Occupational Respiratory Disorders: Caused by exposure to harmful substances in various industries, leading to inflammation of the airways and lungs.
- Asbestosis: Chronic exposure to asbestos dust.
- Silicosis: Long-term exposure to silica dust in mining industries.
- Siderosis: Deposition of inhaled iron particles in tissues can cause pneumoconiosis, hyperferremia, and hemosiderosis.
- Black-lung disease: Developed from inhalation of coal dust, common in coal miners.
Respiration and Energy
- Respiration is a catabolic process that releases energy through the oxidation of food.
- Oxygen is used in the production of metabolic water, a byproduct of calorie burning.
- Gills use a countercurrent flow mechanism to efficiently oxygenate blood.
- Birds have air sacs and parabronchi that allow for continuous gas exchange during both inhalation and exhalation.
- Tracheate animals, like insects, have tracheae and tracheoles that deliver oxygen directly to each cell, making them very active.
- Mountain sickness occurs at high altitudes due to decreased oxygen levels (pO2).
- The ribcage and diaphragm help mammals breathe more effectively.
- The respiratory center controls oxygen and carbon dioxide homeostasis.
- The medulla oblongata regulates inhalation and exhalation.
- A pneumotaxic center in the pons controls the rate and depth of breathing.
- Humans cannot hold their breath for long due to the body's need for oxygen.
- Marine mammals, like elephant seals, have myoglobin (muscle hemoglobin) with a higher affinity for oxygen, allowing them to stay underwater for extended periods.
- Cells require a constant supply of energy produced by the oxidation of glucose, amino acids, and fatty acids, transported through the circulatory system.
Types of Respiration
- Anaerobic respiration: incomplete breakdown of organic molecules with less energy yield, occurring in the absence of oxygen.
- Examples: yeast, bacteria, and muscles under certain conditions.
- C6H12O6 → 2CO2+ 2C2H5OH(ethanol)+2ATP
- C6H12O6 → 2C3H6O3(lactic acid)+2ATP
- Aerobic respiration: complete breakdown of organic molecules with more energy yield, requiring oxygen.
- C6H12O6+6H2O+6O2 → 6CO2+12H2O+36ATP
Respiratory Organs in Animals
- Protozoans and lower invertebrates have simple diffusion across their body surface for gas exchange.
- Earthworms use their moist body wall for gas exchange.
- Insects use a network of tubes (tracheal system) to transport air.
- Spiders and scorpions have "book lungs" for aerial respiration.
- Aquatic arthropods and mollusks use gills for gas exchange.
- Terrestrial forms use lungs, including reptiles, birds, and mammals.
- Amphibians use both moist skin and lungs for gas exchange.
Human Respiratory System
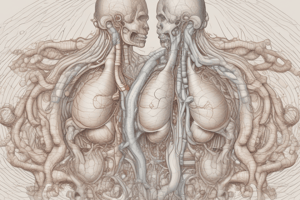
-
External Nostrils: Openings that lead into the nasal chambers.
-
Nasal Chambers: Cavities above the palate separated by a nasal septum, with three parts: (1) vestibular part (hair and glands to filter dust), (2) respiratory part (conditioning inhaled air, containing turbinals), and (3) olfactory part (detecting smell).
-
Naso-pharynx: Upper portion of the pharynx connected to the nasal chambers via internal nostrils.
-
Larynx: Cartilaginous box for sound production (voice box) containing nine cartilages.
- Thyroid: Unpaired cartilage that forms the Adam's apple, larger in males.
- Cricoid: Unpaired cartilage.
- Epiglottis: Unpaired, leaf-like flap that prevents food from entering the larynx.
- Corniculate: Paired, small cartilages.
- Arytenoid: Paired cartilages that anchor the vocal cords.
- Cuneiform: Paired cartilages.
- Vocal Cords: Yellow elastic fibres connecting the thyroid and arytenoid cartilages, producing sound.
- True vocal cords: produce sound
- False vocal cords: folds of mucous membrane that do not produce sound.
- Rima Glottidis: Opening between the true vocal cords and the arytenoid cartilages.
-
Trachea: Windpipe, supported by "C" shaped hyaline cartilage rings.
-
Bronchi: Trachea branches into two primary bronchi, each entering a lung and further dividing into secondary and tertiary bronchi.
-
Bronchioles: Tertiary bronchi further divide into smaller bronchioles.
- Bronchi and initial bronchioles are supported by incomplete cartilaginous rings.
-
Alveoli: Tiny air sacs at the ends of bronchioles, the primary sites of gas exchange.
-
Lungs: Paired organs located in the thoracic cavity, surrounded by a double-layered pleura with pleural fluid for lubrication.
- Conducting part: External nostrils to terminal bronchioles, transports air, cleanses it, humidifies it and warms it.
- Respiratory part: Alveoli, where gas exchange takes place.
-
Thoracic Cavity: Anatomically airtight chamber formed by the vertebral column, sternum, ribs, and diaphragm.
Mechanism of Breathing
- Breathing (Pulmonary Ventilation): Movement of air into and out of the lungs, creating a pressure gradient.
- Inspiration: Drawing air into the lungs, active process requiring muscle contraction.
- Diaphragm contraction increases thoracic volume in the anteroposterior axis.
- External intercostal muscle contraction lifts ribs and sternum, increasing thoracic volume in the dorso-ventral axis.
- Overall thoracic volume increase leads to pulmonary volume increase, decreasing intra-pulmonary pressure and drawing air into the lungs.
- Expiration: Release of alveolar air, passive process due to muscle relaxation.
- Diaphragm and external intercostal muscles relax, reducing thoracic and pulmonary volume.
- Intra-pulmonary pressure increases, forcing air out of the lungs.
- Forced expiration: Internal intercostal muscles and lateral abdominal muscles contract to increase the force of expiration.
- Inspiration: Drawing air into the lungs, active process requiring muscle contraction.
- Spirometer: A device used to measure the volume of air involved in breathing movements, assessing pulmonary function.
Gas Exchange
- Alveoli: Primary sites of gas exchange in the lungs, along with blood and tissues.
- Simple Diffusion: Gas exchange occurs through simple diffusion based on partial pressure gradients, solubility of gases, thickness of the respiratory membrane, surface area, and distance of diffusion.
- Partial Pressure: Pressure contributed by an individual gas in a mixture.
- pO2: Partial pressure of oxygen.
- pCO2: Partial pressure of carbon dioxide.
Partial Pressure of O2 and CO2 at Different Locations:
| Location | pO2 (mmHg) | pCO2 (mmHg) |
|---|---|---|
| Atmospheric Air | 159 | 0.3 |
| Alveoli | 104 | 40 |
| Deoxygenated Blood | 40 | 45 |
| Oxygenated Blood | 95 | 40 |
| Tissues | 40 | 45 |
- Solubility: CO2 is more soluble than O2, meaning it can diffuse faster across the respiratory membrane.
- Respiratory Membrane: Includes the squamous epithelium of the alveolar wall, endothelium of the alveolar capillaries, and basement material.
- Thin membrane facilitates fast diffusion.
Gas Exchange in the Body:
- Pulmonary Gas Exchange (External Respiration):
- O2 diffuses from alveolar air into the blood in the pulmonary capillaries.
- CO2 diffuses from blood into the alveolar air.
- Systemic Gas Exchange (Internal Respiration):
- O2 diffuses from the blood in systemic capillaries into tissues.
- CO2 diffuses from tissues into the systemic capillaries.
Transport of Gases
- Blood: Medium used to transport O2 and CO2.
Oxygen Transport:
-
Plasma: 3% of O2 transported dissolved in plasma.
-
Red Blood Cells (RBCs): 97% of O2 transported by RBCs using haemoglobin.
- Haemoglobin: Red pigmented protein containing iron, each molecule can bind up to four oxygen molecules.
- Oxygenation: Binding of oxygen to haemoglobin in the lungs, forming oxyhaemoglobin, which is bright red. Hb + 4O2 → Hb(O2)4
- Deoxygenation: Dissociation of oxygen from oxyhaemoglobin in tissues, resulting in haemoglobin and oxygen.
- Haemoglobin: Red pigmented protein containing iron, each molecule can bind up to four oxygen molecules.
-
Factors Affecting Oxygen Binding:
- Partial Pressure of O2: Higher pO2 in the lungs promotes binding of oxygen to haemoglobin, while lower pO2 in tissues promotes dissociation.
- Partial Pressure of CO2: Higher pCO2 decreases the affinity of haemoglobin for oxygen.
- Hydrogen Ion Concentration (pH): Higher H+ concentration (lower pH) decreases the affinity of haemoglobin for oxygen.
- Temperature: Higher temperature decreases the affinity of haemoglobin for oxygen.
-
Oxyhaemoglobin Dissociation Curve: A sigmoid curve showing the relationship between haemoglobin saturation with oxygen and partial pressure of oxygen.
- Shift to the right: Indicates decreased affinity of haemoglobin for oxygen, caused by high pCO2, low pH, or higher temperature.
- Shift to the left: Higher affinity of haemoglobin for oxygen, caused by low pCO2, high pH, or low temperature.
-
Bohr Effect: The effect of pCO2 and H+ concentration on the oxygen affinity of haemoglobin.
- High CO2 and low pH: decrease the affinity of haemoglobin for oxygen.
- Low CO2 and high pH: increase the affinity of haemoglobin for oxygen.
Carbon Dioxide Transport:
-
Dissolved State: 7% of CO2 transported dissolved in plasma.
-
Carbaminohaemoglobin: 20-25% of CO2 binds to amino groups in haemoglobin, forming carbaminohaemoglobin. Hb-NH2 + CO2 → Hb-NHCOO- + H+.
- Binding depends on pCO2: High pCO2 in tissues promotes binding, while low pCO2 in alveoli promotes dissociation.
-
Bicarbonates: 70% of CO2 transported as bicarbonate.
- Carbonic Anhydrase: Enzyme present in RBCs that catalyses the reversible reaction between CO2 and H2O to form carbonic acid (H2CO3).
- Bicarbonate Formation: Carbonic acid dissociates into bicarbonate (HCO3-) and H+.
- Bicarbonate Movement: HCO3- diffuses out of RBCs into plasma, while H+ binds to haemoglobin to maintain PH balance.
- Bicarbonate Transport: Bicarbonate ions are transported to the lungs.
- Reverse Reaction: In lungs, low pCO2 promotes the conversion of bicarbonate back into CO2, which is exhaled.
-
Deoxygenated (Venous) Blood: Has a slightly lower pH than oxygenated (arterial) blood due to the presence of CO2.
-
**Hb: ** Amphoteric compound, meaning it can act as both an acid and a base.
Carbon Dioxide Transport
- CO2 is transported in the blood in three ways: dissolved in plasma, bound to hemoglobin, and as bicarbonate ions.
- Bicarbonate ions are the most abundant form of transported CO2.
- At tissues, CO2 diffuses into the blood and reacts with water to form carbonic acid (H2CO3), which then dissociates into bicarbonate ions (HCO3-) and hydrogen ions (H+).
- Hemoglobin buffers the H+ ions, preventing a decrease in blood pH.
- At the lungs, the reaction reverses, releasing CO2 for exhalation.
Chloride Shift
- Bicarbonate ions diffuse from the RBC into the plasma at the tissues.
- Chloride ions diffuse from the plasma into the RBC to maintain electrical neutrality – this is the chloride shift.
- The chloride shift helps facilitate CO2 transport and maintains blood pH.
Regulation of Respiratory Movements
- The respiratory rhythm center in the medulla oblongata controls the basic rhythm of breathing.
- The pneumotaxic center in the pons moderates the rhythm of breathing.
- Chemoreceptors in the medulla oblongata and aortic arch and carotid arteries detect changes in blood CO2 and H+ levels.
- Oxygen plays a relatively insignificant role in regulating breathing.
Respiratory Volumes and Capacities
- Tidal volume (TV): The volume of air inhaled or exhaled during normal breathing (approximately 500 mL).
- Inspiratory reserve volume (IRV): The additional volume of air that can be inhaled forcefully after a normal inhalation (about 2500-3000 mL).
- Expiratory reserve volume (ERV): The additional volume of air that can be exhaled forcefully after a normal exhalation (about 1000-1100 mL).
- Residual volume (RV): The volume of air remaining in the lungs after forced expiration (about 1100-1200 mL).
- Inspiratory capacity (IC): The total volume of air that can be inhaled after a normal exhalation; IC = TV + IRV (around 3000-3500 mL).
- Functional residual capacity (FRC): The volume of air remaining in the lungs after a normal exhalation; FRC = ERV + RV.
- Vital capacity (VC): The maximum volume of air that can be exhaled after a forced inhalation; VC = TV + IRV + ERV.
- Total lung capacity (TLC): The total volume of air that the lungs can hold; TLC = VC + RV, or TLC = ERV + IRV + TV + RV.
Disorders of the Respiratory System
- Asthma: Inflammation of the bronchi and bronchioles, causing spasms of smooth muscle in the airway walls. Symptoms include coughing, wheezing, and difficulty breathing.
- Emphysema: Chronic disorder characterized by damage to and coalescence of alveolar walls, reducing respiratory surface area. Lung shows larger but fewer alveoli, with increased fibrosis and decreased elasticity.
- Bronchitis: Inflammation of the bronchi, causing swelling of the mucous lining, increased mucus production, and narrowing of the bronchi. Symptoms include chronic cough with thick mucus or phlegm.
- Pneumonia: Infection of the lungs caused by bacteria, viruses, fungi, protozoa, or mycoplasmas. Symptoms include inflammation of the lungs, accumulation of mucus in alveoli, and impaired gas exchange.
- Chronic obstructive pulmonary disease (COPD): A group of progressive lung diseases that cause airflow obstruction; includes emphysema, chronic bronchitis, and asthma.
- Occupational respiratory disorders: Lung diseases caused by exposure to harmful substances in the workplace, including:
- Asbestosis: Caused by chronic exposure to asbestos dust.
- Silicosis: Caused by long-term exposure to silica dust.
- Siderosis: Caused by deposition of inhaled iron particles in tissues.
- Black-lung disease (coal workers' pneumoconiosis): Caused by inhalation of coal dust.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.