Podcast
Questions and Answers
Which primary function is carried out by the nasal cavity's mucous membranes?
Which primary function is carried out by the nasal cavity's mucous membranes?
- Filtering, warming, and moistening inhaled air. (correct)
- Exchanging oxygen and carbon dioxide.
- Facilitating vocal resonance.
- Initiating the cough reflex.
How does the structure of the trachea support its function?
How does the structure of the trachea support its function?
- The smooth muscle enables rapid changes in air flow.
- The mucous membrane traps pathogens.
- The cartilage rings allow it to expand during swallowing.
- The cartilage rings prevent collapse during pressure changes. (correct)
What is the primary role of the bronchioles in respiration?
What is the primary role of the bronchioles in respiration?
- To filter and humidify incoming air.
- To produce sound through vocal cord vibration.
- To conduct air to the alveoli and regulate airflow. (correct)
- To exchange gases between air and blood.
Which structural feature of the alveoli directly facilitates gas exchange?
Which structural feature of the alveoli directly facilitates gas exchange?
How does the arrangement of lobes in the lungs affect their function?
How does the arrangement of lobes in the lungs affect their function?
What is the role of the pleural coverings in lung function?
What is the role of the pleural coverings in lung function?
How does the thinness of the respiratory membrane contribute to its function?
How does the thinness of the respiratory membrane contribute to its function?
What is the primary mechanism driving pulmonary ventilation?
What is the primary mechanism driving pulmonary ventilation?
How is the majority of oxygen transported in the blood?
How is the majority of oxygen transported in the blood?
What role do bicarbonate ions play in carbon dioxide transport?
What role do bicarbonate ions play in carbon dioxide transport?
Which area of the brain is primarily responsible for setting the basic rhythm of breathing?
Which area of the brain is primarily responsible for setting the basic rhythm of breathing?
How do chemoreceptors influence respiration?
How do chemoreceptors influence respiration?
How does an increase in body temperature typically affect the breathing rate?
How does an increase in body temperature typically affect the breathing rate?
What is the primary role of carbon dioxide in modifying breathing rate and depth?
What is the primary role of carbon dioxide in modifying breathing rate and depth?
Why is it difficult to voluntarily stop breathing for an extended period?
Why is it difficult to voluntarily stop breathing for an extended period?
How does decreased lung elasticity, due to aging, affect respiration?
How does decreased lung elasticity, due to aging, affect respiration?
What role does the respiratory system play in relation to the circulatory system?
What role does the respiratory system play in relation to the circulatory system?
How do the kidneys support the respiratory system in maintaining homeostasis?
How do the kidneys support the respiratory system in maintaining homeostasis?
Which mechanism is responsible for the exchange of oxygen and carbon dioxide across capillary walls?
Which mechanism is responsible for the exchange of oxygen and carbon dioxide across capillary walls?
What role does hydrostatic pressure play in capillary exchange?
What role does hydrostatic pressure play in capillary exchange?
Flashcards
Nasal Cavity
Nasal Cavity
Hollow space behind the nose, lined with mucous membranes. It filters, warms, and moistens air, trapping dust and pathogens.
Pharynx
Pharynx
Muscular tube connecting nasal cavity to larynx. It's a passageway for air and food and aids in vocalization.
Larynx
Larynx
Cartilaginous structure containing vocal cords. It produces sound and prevents food from entering the trachea.
Trachea
Trachea
Signup and view all the flashcards
Bronchi
Bronchi
Signup and view all the flashcards
Bronchioles
Bronchioles
Signup and view all the flashcards
Alveoli
Alveoli
Signup and view all the flashcards
Lungs
Lungs
Signup and view all the flashcards
Pleural Coverings
Pleural Coverings
Signup and view all the flashcards
Respiratory Membrane
Respiratory Membrane
Signup and view all the flashcards
Pulmonary Ventilation
Pulmonary Ventilation
Signup and view all the flashcards
External Respiration
External Respiration
Signup and view all the flashcards
Internal Respiration
Internal Respiration
Signup and view all the flashcards
Oxygen Transport
Oxygen Transport
Signup and view all the flashcards
Carbon Dioxide Transport
Carbon Dioxide Transport
Signup and view all the flashcards
Gas Exchange in Lungs
Gas Exchange in Lungs
Signup and view all the flashcards
Homeostasis Role
Homeostasis Role
Signup and view all the flashcards
Medulla Oblongata's Role
Medulla Oblongata's Role
Signup and view all the flashcards
Inspiration
Inspiration
Signup and view all the flashcards
Expiration
Expiration
Signup and view all the flashcards
Study Notes
- Organs forming the respiratory passageway from the nasal cavity to alveoli include the nasal cavity, pharynx, larynx, trachea, bronchi, bronchioles, and alveoli.
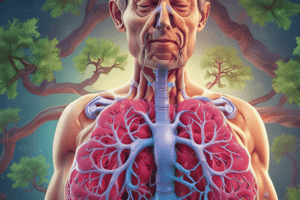
Nasal Cavity
- Structure: Hollow space behind nose, lined with mucous membranes.
- Function: Filters, warms, and moistens air; traps dust and pathogens.
Pharynx
- Structure: Muscular tube connecting the nasal cavity to the larynx.
- Function: Serves as a passageway for air and food; aids in vocalization.
Larynx
- Structure: Cartilaginous structure containing vocal cords.
- Function: Produces sound; prevents food from entering the trachea.
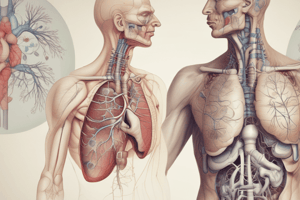
Trachea
- Structure: Tube reinforced with cartilage rings.
- Function: Conducts air to the bronchi; filters and humidifies air.
Bronchi
- Structure: Two main branches from the trachea leading to each lung.
- Function: Conducts air to the bronchioles; filters and humidifies air.
Bronchioles
- Structure: Smaller branches of the bronchi.
- Function: Conducts air to the alveoli; regulates airflow with smooth muscle.
Alveoli
- Structure: Tiny air sacs at the end of bronchioles.
- Function: Site of gas exchange between air and blood.
Lungs
- Structure: Two spongy organs located in the thoracic cavity, composed of lobes (three on the right and two on the left), containing bronchi, bronchioles, and alveoli.
- Function: Main organ for respiration.
- Facilitates gas exchange (oxygen and carbon dioxide) with blood.
Pleural Coverings
- Structure: Consist of two layers—visceral pleura (covers lungs) and parietal pleura (lines thoracic cavity)—with a pleural cavity containing pleural fluid between the layers.
- Function: Reduce friction during breathing movements, create a pressure gradient aiding lung expansion, and provide protection and support to the lungs.
Structure of the Respiratory Membrane
- Composed of alveolar and capillary walls with their fused basement membranes.
- Alveolar wall: Single layer of squamous epithelial cells (type I alveolar cells).
- Capillary wall: Single layer of endothelial cells.
- Fused basement membrane: Thin extracellular matrix between alveolar and capillary walls.
Function Facilitation of the Respiratory Membrane
- Thinness facilitates efficient gas exchange (oxygen and carbon dioxide) by diffusion.
- Large surface area: The extensive surface area of alveoli increases the area available for gas exchange.
- Proximity: Close proximity of blood in capillaries to alveolar air enhances rapid gas diffusion.
Four Events of Respiration
- Pulmonary Ventilation: Movement of air into and out of the lungs, involving inhalation and exhalation, driven by the diaphragm and intercostal muscles.
- External Respiration: Gas exchange between alveoli and blood in pulmonary capillaries, where oxygen diffuses into blood and carbon dioxide diffuses into alveoli.
- Transport of Respiratory Gases: Oxygen and carbon dioxide are transported in the blood; oxygen is carried by hemoglobin in red blood cells, and carbon dioxide is transported as bicarbonate ions.
- Internal Respiration: Gas exchange between blood and tissues, where oxygen diffuses from blood to tissues and carbon dioxide diffuses from tissues to blood.
Mechanisms of Inspiration (Inhalation)
- The diaphragm contracts and moves downward, increasing the thoracic cavity's volume.
- External intercostal muscles contract, lifting the rib cage and further expanding the thoracic cavity.
- Increased volume leads to decreased pressure in the thoracic cavity compared to atmospheric pressure.
- Air flows into the lungs to equalize the pressure difference.
Mechanisms of Expiration (Exhalation)
- The diaphragm relaxes and moves upward, decreasing the thoracic cavity's volume.
- External intercostal muscles relax, allowing the rib cage to descend.
- Decreased volume leads to increased pressure in the thoracic cavity compared to atmospheric pressure.
- Air flows out of the lungs to equalize the pressure difference.
Conditions Necessary for Pulmonary Ventilation
- Clear airways for unobstructed airflow.
- Functional respiratory muscles (diaphragm and intercostals).
- Elasticity of lung tissue to allow expansion and recoil.
- Intact pleural membranes to maintain negative pressure in the pleural cavity.
Oxygen Transport
- Hemoglobin Binding: About 98.5% of oxygen is transported bound to hemoglobin in red blood cells, forming oxyhemoglobin.
- Dissolved in Plasma: A small amount (about 1.5%) is dissolved directly in the plasma.
Carbon Dioxide Transport
- Bicarbonate Ions: About 70% of carbon dioxide is transported as bicarbonate ions (HCO3) in the plasma, formed by the reaction of CO2 with water.
- Carbaminohemoglobin: About 20% binds to hemoglobin, forming carbaminohemoglobin.
- Dissolved in Plasma: Approximately 10% is dissolved directly in the plasma.
Maintenance of Homeostasis
- Oxygen Delivery: Ensures tissues receive adequate oxygen for cellular respiration and energy production.
- Carbon Dioxide Removal: Prevents acid-base imbalance by removing CO2, a byproduct of metabolism, from the body.
- Regulation: Respiratory and cardiovascular systems adjust breathing rate and blood flow to meet the body's changing demands, maintaining homeostasis.
Gas Exchange in the Lungs (External Respiration)
- Occurs in the alveoli: Oxygen from inhaled air diffuses across the alveolar membrane into the blood in pulmonary capillaries.
- Carbon dioxide: A waste product from metabolism, diffuses from the blood into the alveoli to be exhaled.
Gas Exchange in the Tissues (Internal Respiration)
- Oxygen-rich blood: Oxygen diffuses from the blood into the cells of the body tissues.
- Carbon dioxide: Produced by cells as a metabolic waste diffuses into the blood to be sent back to the lungs.
Brain Areas Involved in Control of Respiration
- Medulla Oblongata: Contains the respiratory rhythmicity centers that set the basic rhythm of breathing and regulates the rate and depth of breathing through the dorsal and ventral respiratory groups.
- Pons: Contains the pneumotaxic and apneustic centers that modulate the medulla's activity and helps smooth the transition between inhalation and exhalation.
Roles of Medulla Oblongata in Respiration
- Initiates and maintains the rhythmic cycle of breathing.
- It responds to changes in carbon dioxide and pH levels in the blood to adjust breathing rate.
Roles of Pons in Respiration
- Fine-tunes the breathing pattern to ensure smooth and coordinated respiratory movements.
Nervous System Influence on Respiration
- Medulla Oblongata: Respiratory centers regulate the basic rhythm of breathing, responding to changes in blood levels of carbon dioxide and pH.
- Pons: Modulates the activity of the medulla to ensure smooth transitions between inhalation and exhalation.
- Chemoreceptors: Located in the medulla, aortic arch, and carotid bodies; detect changes in blood CO2, O2, and pH levels, sending signals to the respiratory centers to adjust breathing.
Physical Factors Influencing Breathing Rate
- Temperature: An increase, such as during fever or exercise, can increase the breathing rate to help dissipate heat and meet the increased oxygen demand.
- Exercise: Physical activity increases the breathing rate to meet the metabolic needs for oxygen and eliminate carbon dioxide.
- Lung Stretch Receptors: Activation of stretch receptors in the lungs during inhalation can influence the rate and depth of breathing.
- Emotional State: Emotions like stress, anxiety, or excitement can affect breathing rate through the autonomic nervous system.
- Body Position: Lying down can decrease lung volume and affect breathing rate, while standing or sitting upright can facilitate easier breathing.
Volition (Conscious Control)
- Individuals can consciously control their breathing rate and depth, such as during speaking, singing, or holding their breath.
Emotional Factors
- Emotions like stress, anxiety, excitement, or relaxation can influence breathing patterns.
- The autonomic nervous system mediates these changes, often increasing breathing rate during stress or anxiety.
Chemical Factors (Oxygen and Carbon Dioxide)
- Levels of CO2 and O2 in the blood are monitored by chemoreceptors.
Roles of Oxygen and Carbon Dioxide in Modifying Breathing Rate and Depth
- Carbon Dioxide (CO2): Primary driver for changes in breathing rate and depth; high levels of CO2 lead to increased acidity, detected by central chemoreceptors in the medulla oblongata.
- Oxygen (O2): Detected by peripheral chemoreceptors located in the carotid bodies and aortic arch; low levels can trigger an increase in breathing rate and depth, although this response is less sensitive compared to CO2.
Why It's Not Possible to Stop Breathing Voluntarily
- Involuntary Control: Breathing is primarily controlled by the autonomic nervous system, which operates independently of conscious control.
- Homeostasis: The body's need to maintain stable levels of oxygen and carbon dioxide overrides voluntary control.
- Chemoreceptor Response: High levels of carbon dioxide or low levels of oxygen in the blood trigger automatic responses to resume breathing.
- Protective Mechanism: The inability to voluntarily stop breathing for extended periods is a protective mechanism to prevent harm from oxygen deprivation.
Effects of Aging on the Respiratory System
- Decreased Lung Elasticity: Lungs lose their flexibility, reducing the ability to expand and contract efficiently.
- Reduced Respiratory Muscle Strength: The diaphragm and intercostal muscles weaken, making it harder to breathe deeply.
- Decreased Alveolar Surface Area: The number of functional alveoli decreases, reducing the surface area available for gas exchange.
- Impaired Gas Exchange: Changes in the alveolar walls and capillaries can lead to less efficient oxygen and carbon dioxide exchange.
- Altered Breathing Patterns: Older adults may experience changes in breathing patterns, such as increased breathing rate or shallower breaths.
- Increased Susceptibility to Infections: The immune response in the respiratory tract may weaken, increasing the risk of infections like pneumonia.
Homeostatic Relationship Between the Respiratory System and Other Body Systems
- Circulatory System: The respiratory system provides oxygen to the blood and removes carbon dioxide, which is transported by the circulatory system to and from cells.
- Nervous System: The nervous system regulates breathing rate and depth through the medulla oblongata and pons.
It responds to changes in blood gas levels, ensuring proper oxygen and carbon dioxide balance.
- Muscular System: Respiratory muscles, such as the diaphragm and intercostal muscles, facilitate breathing movements.
- Renal System: The kidneys help regulate blood pH by excreting hydrogen ions and reabsorbing bicarbonate, complementing the respiratory system's role in maintaining acid-base balance.
- Immune System: The respiratory system acts as a barrier to pathogens and contains immune cells that help protect against infections.
Cardiac Output Definition
- Cardiac output is the volume of blood the heart pumps per minute.
- It is a crucial measure of heart function and overall circulatory efficiency.
Factors Contributing to Cardiac Output
- Heart Rate (HR): The number of heartbeats per minute; increased heart rate can raise cardiac output, assuming stroke volume remains constant.
- Stroke Volume (SV): The amount of blood ejected by the left ventricle with each heartbeat, influenced by preload, contractility, and afterload.
Cardiac Output (CO) = Heart Rate (HR) × Stroke Volume (SV)
- Additional Influencing Factors:
- Preload: The degree of stretch of the heart muscle before contraction, affecting stroke volume.
- Contractility: The strength of heart muscle contraction, influencing stroke volume.
- Afterload: The resistance the heart must overcome to eject blood, impacting stroke volume.
Phases of the Cardiac Cycle and Maintaining Cardiac Output
- Atrial Systole: Atria contract, pushing blood into the ventricles; proper atrial contraction ensures optimal ventricular filling, affecting preload and stroke volume.
- Ventricular Systole: Ventricles contract, ejecting blood into the aorta and pulmonary artery; effective ventricular contraction is crucial for maintaining stroke volume and cardiac output.
- Diastole: Heart muscle relaxes, allowing chambers to fill with blood.
Maintaining Cardiac Output
- Heart Rate Regulation: The autonomic nervous system adjusts heart rate to meet the body's oxygen demands, influencing cardiac output.
- Stroke Volume Optimization: Factors like preload, contractility, and afterload are managed to ensure efficient blood ejection and filling.
- Balance Between Phases: Proper timing and coordination of the cardiac cycle phases ensure efficient blood flow and cardiac output.
Effects on Heart Rate and Cardiac Output
- Stimulation by the Vagus Nerve: The vagus nerve decreases heart rate by releasing acetylcholine, which slows the pacemaker activity of the sinoatrial node.
- *Exercise: Increases heart rate and stroke volume to meet the higher oxygen demands of muscles and enhances cardiac output due to increased sympathetic stimulation and improved venous return.
- Epinephrine: Increases heart rate and contractility.
- Various Ions:
- Calcium (Ca2+): Increases contractility and can increase heart rate.
- Potassium (K+): High levels can decrease heart rate and contractility.
- Sodium (Na+): Imbalances can affect heart rhythm and contractility.
Comparison and Contrast of Blood Vessels
- Arteries: Thick, elastic walls with a narrow lumen, composed of three layers (tunica intima, tunica media, and tunica externa); carry oxygenated blood away from the heart (except pulmonary arteries) at high pressure and velocity.
- Veins: Thinner walls than arteries, with a wider lumen and valves to prevent backflow; carry deoxygenated blood back to the heart (except pulmonary veins) at lower pressure and velocity.
- Arterioles: Smaller branches of arteries with a thinner wall and more smooth muscle; regulate blood flow into capillaries through vasoconstriction and vasodilation, controlling blood pressure.
- Venules: Small vessels that collect blood from capillaries, with thin walls; drain blood from capillaries into larger veins.
- Capillaries: Microscopic vessels with a single layer of endothelial cells; site of exchange of gases, nutrients, and waste between blood and tissues.
Unique Features of Arterial Circulation of the Brain
- Circle of Willis: A circular network of arteries at the base of the brain that provides multiple pathways for blood flow, ensuring consistent supply even if one part is blocked.
- Blood-Brain Barrier: Protects the brain by preventing harmful substances from entering, while allowing essential nutrients to pass through.
- High Oxygen Demand: The brain requires a constant and rich supply of oxygenated blood due to its high metabolic activity.
Unique Features of Hepatic Portal Circulation
- Portal Vein System: Transports nutrient-rich blood from the gastrointestinal tract and spleen directly to the liver for processing.
- Liver Processing: The liver metabolizes nutrients, detoxifies substances, and stores energy, playing a crucial role in maintaining homeostasis.
- Dual Blood Supply: The liver receives blood from both the hepatic portal vein and the hepatic artery, ensuring it gets both oxygenated and nutrient-rich blood.
Pulse Definition
- The pulse is the rhythmic expansion and contraction of an artery as blood is forced through it by the beating of the heart.
Common Pulse Points
- Radial Pulse: Located on the wrist (thumb side).
- Carotid Pulse: Located on either side of the neck (windpipe side).
- Brachial Pulse: Inside of the arm (near the elbow).
- Femoral Pulse: In the groin area (where the leg meets the pelvis).
- Popliteal Pulse: Behind the knee.
- Dorsalis Pedis Pulse: On the top of the foot.
- Posterior Tibial Pulse: Behind the ankle bone (inner side of the leg).
Blood Pressure Definition
- Blood pressure is the force exerted by circulating blood on the walls of blood vessels, measured in millimeters of mercury (mmHg) as systolic pressure (pressure during heartbeats) over diastolic pressure (pressure between heartbeats).
Factors Affecting Blood Pressure
- Heart Rate: An increased heart rate can raise blood pressure as more blood is pumped through the vessels.
- Blood Volume: Higher blood volume increases pressure on vessel walls.
- Resistance of Blood Vessels: Narrow or constricted vessels increase resistance.
- Elasticity of Arteries: Less elastic arteries can lead to higher blood pressure.
- Blood Viscosity: Thicker blood can increase resistance and pressure.
- Hormones: Like adrenaline, can increase heart rate and blood pressure.
- Diet & Lifestyle: High salt intake, obesity, and lack of exercise can contribute to higher blood pressure.
Maintaining Homeostasis through Blood Pressure Regulation
- Heart Rate: Increased heart rate raises blood pressure, ensuring sufficient blood flow during activities or stress, regulated by the autonomic nervous system.
- Blood Volume: Higher blood volume increases pressure; kidneys play a key role in regulating blood volume, ensuring tissues receive sufficient nutrients.
- Vessel Resistance: Constriction increases resistance and pressure, directing blood flow to essential organs.
- Elasticity of Arteries: Elastic arteries help buffer changes in pressure, maintaining steady flow.
- Aging or disease can reduce elasticity, impacting homeostasis.
Exchanges Across Capillary Walls
- Diffusion: Oxygen, carbon dioxide, and small solutes move across capillary walls from areas of high concentration to low concentration.
- Filtration: Driven by hydrostatic pressure, water and small solutes are forced out of the capillaries into the interstitial fluid.
- Osmosis: Water moves back into the capillaries due to osmotic pressure, influenced by plasma proteins.
Forces Influencing Exchanges
- Hydrostatic Pressure: The force exerted by the fluid inside the capillaries pushes fluid out into the interstitial space.
- Osmotic Pressure: The pull exerted by proteins draws water back into the capillaries.
- Net Filtration Pressure: The balance between hydrostatic and osmotic pressures determines the direction and rate of fluid movement.
Impact of Aging on the Cardiovascular System
- Heart Structure Changes: Thickening of the heart walls, particularly the left ventricle, and a decrease in the number of pacemaker cells.
- Blood Vessels: Arteries become stiffer and less elastic, increasing blood pressure, with the accumulation of plaque (atherosclerosis).
- Blood Pressure Regulation: Increased risk of hypertension due to changes in vessel elasticity and plaque buildup; altered blood pressure regulation mechanisms.
- Cardiac Output: Reduced efficiency in pumping blood and decreased maximum heart rate during physical activity.
Homeostatic Relationship Between the Cardiovascular System and Other Body Systems
- Respiratory System: Transports oxygen from the lungs to tissues and removes carbon dioxide.
- Renal System: Regulates blood volume and pressure through filtration and reabsorption of fluids.
- Endocrine System: Coordinates responses to stress and regulates long-term blood pressure control.
- Digestive System: Supplies nutrients absorbed from food to the bloodstream.
- Musculoskeletal System: Provides oxygen and nutrients to muscles for contraction and movement.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.