Podcast
Questions and Answers
Which of the following mechanisms primarily facilitates the removal of carbon dioxide from the body?
Which of the following mechanisms primarily facilitates the removal of carbon dioxide from the body?
- Cellular respiration
- Ventilation (correct)
- Blood pressure regulation
- Sound production
How does the respiratory system contribute to maintaining blood pressure?
How does the respiratory system contribute to maintaining blood pressure?
- By regulating the pH of the blood via carbon dioxide levels
- By secreting angiotensin-converting enzyme (ACE) (correct)
- By directly altering blood volume through excretion of fluids
- By facilitating gas exchange in the alveoli
If a patient has difficulty swallowing, which anatomical structure of the respiratory system might be impaired?
If a patient has difficulty swallowing, which anatomical structure of the respiratory system might be impaired?
- Trachea
- Epiglottis
- Pharynx (correct)
- Larynx
What characteristic of the alveoli's epithelium makes it particularly well-suited for gas exchange?
What characteristic of the alveoli's epithelium makes it particularly well-suited for gas exchange?
Which of the following best describes the conducting airways as they extend from the bronchi to the bronchioles?
Which of the following best describes the conducting airways as they extend from the bronchi to the bronchioles?
According to Boyle's Law, what happens to the pressure within the lungs during inhalation?
According to Boyle's Law, what happens to the pressure within the lungs during inhalation?
Which muscles are primarily involved in active inspiration?
Which muscles are primarily involved in active inspiration?
Which of the following nervous system components stimulates the diaphragm, leading to its contraction?
Which of the following nervous system components stimulates the diaphragm, leading to its contraction?
What is the primary role of the Dorsal Respiratory Group (DRG) located in the medulla oblongata?
What is the primary role of the Dorsal Respiratory Group (DRG) located in the medulla oblongata?
How is the majority of oxygen transported in the blood?
How is the majority of oxygen transported in the blood?
What role does carbonic anhydrase play in carbon dioxide transport?
What role does carbonic anhydrase play in carbon dioxide transport?
What is the effect of the chloride shift on maintaining electrostatic neutrality during carbon dioxide transport?
What is the effect of the chloride shift on maintaining electrostatic neutrality during carbon dioxide transport?
What is the approximate value of a normal tidal volume (TV) in a healthy adult?
What is the approximate value of a normal tidal volume (TV) in a healthy adult?
Which of the following equations correctly defines Inspiratory Capacity (IC)?
Which of the following equations correctly defines Inspiratory Capacity (IC)?
Pulmonary edema primarily affects which aspect of respiratory function?
Pulmonary edema primarily affects which aspect of respiratory function?
What physiological change is characteristic of emphysema?
What physiological change is characteristic of emphysema?
Which lung sound is most indicative of fluid in the alveoli?
Which lung sound is most indicative of fluid in the alveoli?
What is the primary function of the cilia lining the trachea?
What is the primary function of the cilia lining the trachea?
During forced expiration, which muscles are actively engaged to reduce lung volume?
During forced expiration, which muscles are actively engaged to reduce lung volume?
Which of the following respiratory conditions is characterized by reversible airway constriction?
Which of the following respiratory conditions is characterized by reversible airway constriction?
How does the contraction of the diaphragm contribute to the process of inspiration?
How does the contraction of the diaphragm contribute to the process of inspiration?
What is the functional consequence of bronchioles gaining smooth muscle?
What is the functional consequence of bronchioles gaining smooth muscle?
Which of the following best explains the role of the pneumotaxic center in the pons?
Which of the following best explains the role of the pneumotaxic center in the pons?
How does the respiratory system contribute to the regulation of blood pH?
How does the respiratory system contribute to the regulation of blood pH?
How does an increase in altitude affect oxygen transport in the blood, and what compensatory mechanism might the body employ?
How does an increase in altitude affect oxygen transport in the blood, and what compensatory mechanism might the body employ?
Which of the following describes the most significant role of bicarbonate ions ($HCO_3^−$) in carbon dioxide transport?
Which of the following describes the most significant role of bicarbonate ions ($HCO_3^−$) in carbon dioxide transport?
How does the anatomical structure of the trachea support its function?
How does the anatomical structure of the trachea support its function?
What is the interdependence between tidal volume (TV), inspiratory reserve volume (IRV), and expiratory reserve volume (ERV) in determining vital capacity (VC)?
What is the interdependence between tidal volume (TV), inspiratory reserve volume (IRV), and expiratory reserve volume (ERV) in determining vital capacity (VC)?
How might a respiratory therapist use the understanding of lung volumes to assess a patient with restrictive lung disease?
How might a respiratory therapist use the understanding of lung volumes to assess a patient with restrictive lung disease?
How do conditions like emphysema affect the mechanics of breathing, specifically regarding alveolar function and lung compliance?
How do conditions like emphysema affect the mechanics of breathing, specifically regarding alveolar function and lung compliance?
Which of the following scenarios would most likely result in an increase in the secretion of Angiotensin-Converting Enzyme (ACE)?
Which of the following scenarios would most likely result in an increase in the secretion of Angiotensin-Converting Enzyme (ACE)?
In a patient with pulmonary edema, the accumulation of fluid in the alveoli directly impairs which aspect of respiratory function?
In a patient with pulmonary edema, the accumulation of fluid in the alveoli directly impairs which aspect of respiratory function?
If a patient is experiencing inflammation of the larynx, which of the following symptoms would you most likely observe?
If a patient is experiencing inflammation of the larynx, which of the following symptoms would you most likely observe?
How does the mucociliary escalator, driven by the ciliated epithelium of the trachea, protect the respiratory system?
How does the mucociliary escalator, driven by the ciliated epithelium of the trachea, protect the respiratory system?
During forced expiration, such as when blowing out candles, which muscles are actively involved in decreasing the volume of the thoracic cavity?
During forced expiration, such as when blowing out candles, which muscles are actively involved in decreasing the volume of the thoracic cavity?
When auscultating a patient's lungs, you hear crackles (rales). What is the most likely cause of this lung sound?
When auscultating a patient's lungs, you hear crackles (rales). What is the most likely cause of this lung sound?
What type of epithelial tissue is primarily responsible for facilitating gas exchange in the alveoli?
What type of epithelial tissue is primarily responsible for facilitating gas exchange in the alveoli?
According to Boyle's Law, how are pressure and volume related in the context of pulmonary ventilation?
According to Boyle's Law, how are pressure and volume related in the context of pulmonary ventilation?
A patient is diagnosed with pharyngitis. Which anatomical structure is primarily affected by this condition?
A patient is diagnosed with pharyngitis. Which anatomical structure is primarily affected by this condition?
How does the body maintain electrostatic neutrality during the chloride shift?
How does the body maintain electrostatic neutrality during the chloride shift?
How does the secretion of Angiotensin-Converting Enzyme (ACE) by the respiratory system contribute to blood pressure regulation?
How does the secretion of Angiotensin-Converting Enzyme (ACE) by the respiratory system contribute to blood pressure regulation?
What is the functional relationship between the apneustic and pneumotaxic centers located in the pons?
What is the functional relationship between the apneustic and pneumotaxic centers located in the pons?
How does the anatomical structure of the bronchioles facilitate their function in respiration?
How does the anatomical structure of the bronchioles facilitate their function in respiration?
How does the process of ventilation directly support cellular respiration?
How does the process of ventilation directly support cellular respiration?
What is the role of carbonic anhydrase in the transport of carbon dioxide ($CO_2$) within the bloodstream?
What is the role of carbonic anhydrase in the transport of carbon dioxide ($CO_2$) within the bloodstream?
How does the respiratory system facilitate the excretion of metabolic waste products?
How does the respiratory system facilitate the excretion of metabolic waste products?
What is the primary function of the epiglottis during the process of swallowing?
What is the primary function of the epiglottis during the process of swallowing?
Which of the following best describes the mechanism by which the medulla oblongata regulates respiration during quiet breathing?
Which of the following best describes the mechanism by which the medulla oblongata regulates respiration during quiet breathing?
How does the anatomical arrangement of the trachea, specifically the C-shaped hyaline cartilage rings, support its function?
How does the anatomical arrangement of the trachea, specifically the C-shaped hyaline cartilage rings, support its function?
During forced expiration, which of the following muscular actions contributes most significantly to decreasing thoracic volume?
During forced expiration, which of the following muscular actions contributes most significantly to decreasing thoracic volume?
What is the relationship between lung compliance and alveolar structure in a patient with emphysema?
What is the relationship between lung compliance and alveolar structure in a patient with emphysema?
How does the respiratory system contribute to maintaining acid-base balance in the body?
How does the respiratory system contribute to maintaining acid-base balance in the body?
A patient presents with inflammation of the pharynx. Which of the following symptoms is most likely to be present?
A patient presents with inflammation of the pharynx. Which of the following symptoms is most likely to be present?
How does the chloride shift maintain electrostatic neutrality during carbon dioxide transport?
How does the chloride shift maintain electrostatic neutrality during carbon dioxide transport?
During auscultation of a patient's lungs, a respiratory therapist hears high-pitched whistling sounds primarily during exhalation. Which condition is most likely indicated by this observation?
During auscultation of a patient's lungs, a respiratory therapist hears high-pitched whistling sounds primarily during exhalation. Which condition is most likely indicated by this observation?
How does the mucociliary escalator protect the respiratory system from infection and irritation?
How does the mucociliary escalator protect the respiratory system from infection and irritation?
What is the effect of an increase in altitude on the oxygen saturation of hemoglobin and what compensatory mechanism might the body employ?
What is the effect of an increase in altitude on the oxygen saturation of hemoglobin and what compensatory mechanism might the body employ?
What immediate effect would fluid accumulation in the alveoli, caused by pulmonary edema, elicit on respiratory function?
What immediate effect would fluid accumulation in the alveoli, caused by pulmonary edema, elicit on respiratory function?
What is the primary function of Type II alveolar cells in the lungs?
What is the primary function of Type II alveolar cells in the lungs?
Which statement accurately describes the interdependence between tidal volume (TV), inspiratory reserve volume (IRV), and expiratory reserve volume (ERV) in determining vital capacity (VC)?
Which statement accurately describes the interdependence between tidal volume (TV), inspiratory reserve volume (IRV), and expiratory reserve volume (ERV) in determining vital capacity (VC)?
Flashcards
Gas Exchange
Gas Exchange
Transfer of oxygen (O2) into blood and removal of carbon dioxide (CO2) from blood.
Cellular Respiration
Cellular Respiration
Oxygen used by mitochondria to generate ATP.
Ventilation
Ventilation
Mechanical movement of air into and out of lungs.
pH Regulation
pH Regulation
Signup and view all the flashcards
Excretion (Respiratory)
Excretion (Respiratory)
Signup and view all the flashcards
Sound Production (Respiratory)
Sound Production (Respiratory)
Signup and view all the flashcards
Blood Pressure Regulation (Respiratory)
Blood Pressure Regulation (Respiratory)
Signup and view all the flashcards
Nasal Cavity Function
Nasal Cavity Function
Signup and view all the flashcards
Pharynx (throat)
Pharynx (throat)
Signup and view all the flashcards
Larynx (voice box)
Larynx (voice box)
Signup and view all the flashcards
Epiglottis
Epiglottis
Signup and view all the flashcards
Trachea
Trachea
Signup and view all the flashcards
Alveoli
Alveoli
Signup and view all the flashcards
Boyle's Law
Boyle's Law
Signup and view all the flashcards
Inspiration (Active)
Inspiration (Active)
Signup and view all the flashcards
Expiration (Passive during rest)
Expiration (Passive during rest)
Signup and view all the flashcards
Phrenic Nerve
Phrenic Nerve
Signup and view all the flashcards
DRG (Dorsal Respiratory Group)
DRG (Dorsal Respiratory Group)
Signup and view all the flashcards
VRG (Ventral Respiratory Group)
VRG (Ventral Respiratory Group)
Signup and view all the flashcards
Tidal Volume (TV)
Tidal Volume (TV)
Signup and view all the flashcards
Bronchi to Bronchioles
Bronchi to Bronchioles
Signup and view all the flashcards
Cilia in the trachea
Cilia in the trachea
Signup and view all the flashcards
Apneustic Center
Apneustic Center
Signup and view all the flashcards
Pneumotaxic Center
Pneumotaxic Center
Signup and view all the flashcards
Inspiratory Reserve Volume (IRV)
Inspiratory Reserve Volume (IRV)
Signup and view all the flashcards
Expiratory Reserve Volume (ERV)
Expiratory Reserve Volume (ERV)
Signup and view all the flashcards
Residual Volume (RV)
Residual Volume (RV)
Signup and view all the flashcards
Vital Capacity (VC)
Vital Capacity (VC)
Signup and view all the flashcards
Inspiratory Capacity (IC)
Inspiratory Capacity (IC)
Signup and view all the flashcards
Functional Residual Capacity (FRC)
Functional Residual Capacity (FRC)
Signup and view all the flashcards
Total Lung Capacity (TLC)
Total Lung Capacity (TLC)
Signup and view all the flashcards
Pharyngitis
Pharyngitis
Signup and view all the flashcards
Laryngitis
Laryngitis
Signup and view all the flashcards
Asthma
Asthma
Signup and view all the flashcards
COPD
COPD
Signup and view all the flashcards
Emphysema
Emphysema
Signup and view all the flashcards
Pulmonary Edema
Pulmonary Edema
Signup and view all the flashcards
Wheezes
Wheezes
Signup and view all the flashcards
Stridor
Stridor
Signup and view all the flashcards
Crackles (Rales)
Crackles (Rales)
Signup and view all the flashcards
Muscles of Forced Inspiration
Muscles of Forced Inspiration
Signup and view all the flashcards
Muscles of Forced Expiration
Muscles of Forced Expiration
Signup and view all the flashcards
Chloride Shift
Chloride Shift
Signup and view all the flashcards
Pleural Friction Rub
Pleural Friction Rub
Signup and view all the flashcards
Study Notes
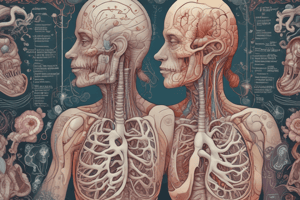
Key Functions of the Respiratory System
- Gas exchange involves transferring oxygen (O₂) into the blood and removing carbon dioxide (CO₂) from the blood
- Cellular respiration refers to the use of oxygen by mitochondria to produce ATP
- Ventilation is the mechanical process of moving air into and out of the lungs
- pH regulation happens because CO₂ levels affect pH; the respiratory system helps regulate pH by exhaling CO₂
- Excretion removes volatile wastes, such as water vapor and CO₂
- Sound production occurs via the larynx, specifically the vocal cords
- Blood pressure regulation happens through the secretion of angiotensin-converting enzyme (ACE)
Respiratory Anatomy and Epithelium
-
The nasal cavity warms, filters, and humidifies air
-
The pharynx (throat) utilizes stratified squamous epithelium, and acts as a passage for both food and air
-
The larynx (voice box) contains vocal cords, with laryngitis referring to inflammation
-
The epiglottis is a flap made of hyaline cartilage that prevents food from entering the trachea
-
The trachea is made of C-shaped hyaline cartilage and lined with pseudostratified ciliated columnar epithelium
-
Cilia beat to move mucus and debris upwards, working against airflow
-
The series of bronchi to bronchioles serve as conducting airways, and the bronchioles lose cartilage while gaining smooth muscle
-
The alveoli are the site of gas exchange and use simple squamous epithelium for rapid diffusion
Mechanics of Breathing
- Boyle’s Law states that pressure and volume are inversely related
Inspiration (Active)
- The diaphragm and external intercostals contract during inspiration
- Volume increases and pressure decreases, resulting in air flowing in
Expiration (Passive during rest)
- The diaphragm and intercostals relax during expiration
- Volume decreases and pressure increases, resulting in air flowing out
Forced Breathing
- Forced inspiration involves the sternocleidomastoid, scalenes, and pectoralis major muscles
- Forced expiration involves abdominal muscles, like rectus abdominis and obliques, as well as internal intercostals
Nervous System Control
- The phrenic nerve stimulates the diaphragm
- The medulla oblongata has two key regions:
- The Dorsal Respiratory Group (DRG) controls quiet breathing
- The Ventral Respiratory Group (VRG) controls forced breathing
- The pons also contains respiratory centers:
- The Apneustic Center stimulates the DRG, promoting inspiration
- The Pneumotaxic Center inhibits the apneustic center, promoting expiration
Gas Exchange and Transport
- Oxygen (O₂) primarily binds to hemoglobin in red blood cells (98%)
- Some oxygen (2%) dissolves in plasma
- Carbon dioxide (CO₂) is transported in three ways:
- As bicarbonate (HCO₃⁻) – 70% via carbonic anhydrase
- Bound to hemoglobin (carbaminohemoglobin) – 23%
- Dissolved in plasma – 7%
- The chloride shift maintains electrostatic neutrality as HCO₃⁻ exits RBCs and Cl⁻ enters
Respiratory Volumes and Capacities
- Tidal Volume (TV) is the volume of a normal breath, approximately 500 mL
- Inspiratory Reserve Volume (IRV) is the additional volume from a forced inhale after a normal breath, roughly 3100 mL
- Expiratory Reserve Volume (ERV) is the additional volume from a forced exhale after a normal breath, about 1200 mL
- Residual Volume (RV) is the air remaining after a maximal exhale, around 1200 mL
Capacities
- Vital Capacity (VC) = TV + IRV + ERV
- Inspiratory Capacity (IC) = TV + IRV
- Functional Residual Capacity (FRC) = ERV + RV
- Total Lung Capacity (TLC) = TV + IRV + ERV + RV
Respiratory Conditions
- Pharyngitis is inflammation of the pharynx, resulting in a sore throat
- Laryngitis is inflammation of the larynx, leading to loss of voice
- Asthma is a reversible airway constriction
- COPD (Chronic Obstructive Pulmonary Disease) is a chronic airflow obstruction, including conditions like emphysema and chronic bronchitis
- Emphysema involves alveolar destruction and increased compliance
- Pulmonary Edema refers to fluid in the alveoli, leading to decreased diffusion distance
Auscultation – Lung Sounds
- Wheezes are high-pitched sounds caused by narrowed airways
- Stridor is a harsh sound caused by upper airway obstruction
- Crackles (Rales) are caused by fluid in the alveoli
- Pleural Friction Rub is a sound caused by inflamed pleural surfaces rubbing together
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.