Podcast
Questions and Answers
What role does hydrogen bonding play in the surface tension of water?
What role does hydrogen bonding play in the surface tension of water?
- It creates a cohesive force that allows water molecules to cling together. (correct)
- It promotes the evaporation of water.
- It decreases the density of water.
- It increases the temperature of the water.
How does increased surface tension affect lung compliance?
How does increased surface tension affect lung compliance?
- It increases lung compliance.
- It decreases lung compliance. (correct)
- It only affects the alveoli during inspiration.
- It has no effect on lung compliance.
What effect does surface tension have on alveolar size?
What effect does surface tension have on alveolar size?
- It promotes alveolar expansion.
- It has no impact on alveolar size.
- It causes alveoli to collapse. (correct)
- It maintains a constant alveolar size.
What is a consequence of damage to the alveoli walls in emphysema?
What is a consequence of damage to the alveoli walls in emphysema?
What role do alveolar macrophages play in response to irritants in smokers?
What role do alveolar macrophages play in response to irritants in smokers?
What is the primary factor that causes air to flow out of the lungs during expiration?
What is the primary factor that causes air to flow out of the lungs during expiration?
During active expiration, which muscles primarily contribute to increasing intra-alveolar pressure?
During active expiration, which muscles primarily contribute to increasing intra-alveolar pressure?
What happens to the diaphragm at the end of inspiration?
What happens to the diaphragm at the end of inspiration?
Which of the following statements is true regarding the normal, resting ventilation rate for an adult?
Which of the following statements is true regarding the normal, resting ventilation rate for an adult?
What mechanism prevents the lungs from collapsing during expiration, despite the increase in intrapleural pressure?
What mechanism prevents the lungs from collapsing during expiration, despite the increase in intrapleural pressure?
Which physiological change characterizes expiration?
Which physiological change characterizes expiration?
What is the effect of abdominal muscle contraction during active expiration?
What is the effect of abdominal muscle contraction during active expiration?
What occurs when alveolar pressure equals atmospheric pressure?
What occurs when alveolar pressure equals atmospheric pressure?
How does air flow during expiration according to Boyle's law?
How does air flow during expiration according to Boyle's law?
What is the role of the suction pump in managing pneumothorax?
What is the role of the suction pump in managing pneumothorax?
What is the main characteristic of hypoxic hypoxia?
What is the main characteristic of hypoxic hypoxia?
Which condition is typically associated with ischemic hypoxia?
Which condition is typically associated with ischemic hypoxia?
What blood pH value is considered normal in arterial blood?
What blood pH value is considered normal in arterial blood?
Which of the following causes is classified under histotoxic hypoxia?
Which of the following causes is classified under histotoxic hypoxia?
Which factor contributes to anemic hypoxia?
Which factor contributes to anemic hypoxia?
What characterizes chronic obstructive pulmonary disease (COPD)?
What characterizes chronic obstructive pulmonary disease (COPD)?
Which of the following factors can trigger chronic bronchitis?
Which of the following factors can trigger chronic bronchitis?
How does asthma primarily differ from COPD in terms of airway obstruction?
How does asthma primarily differ from COPD in terms of airway obstruction?
What causes the thickening of airway walls during an asthma attack?
What causes the thickening of airway walls during an asthma attack?
What is the effect of pulmonary fibrosis on lung function?
What is the effect of pulmonary fibrosis on lung function?
Which of the following defines hypoxia?
Which of the following defines hypoxia?
What is the primary role of the body in response to hypoxia and hypercapnia?
What is the primary role of the body in response to hypoxia and hypercapnia?
In chronic bronchitis, what primarily causes the airways to narrow?
In chronic bronchitis, what primarily causes the airways to narrow?
What primarily stimulates the diaphragm during inspiration?
What primarily stimulates the diaphragm during inspiration?
Which of the following muscles is NOT considered an inspiratory muscle?
Which of the following muscles is NOT considered an inspiratory muscle?
During quiet breathing, expiration is primarily considered a ___ process.
During quiet breathing, expiration is primarily considered a ___ process.
What happens to intra-alveolar pressure during inspiration?
What happens to intra-alveolar pressure during inspiration?
What is the role of the intercostal muscles during inspiration?
What is the role of the intercostal muscles during inspiration?
What occurs at the end of inspiration regarding lung volume?
What occurs at the end of inspiration regarding lung volume?
Which pressure is lower than atmospheric pressure during inspiration?
Which pressure is lower than atmospheric pressure during inspiration?
How is a pneumothorax created?
How is a pneumothorax created?
What happens to the diaphragm during expiration?
What happens to the diaphragm during expiration?
Which accessory muscles assist during deeper inspirations?
Which accessory muscles assist during deeper inspirations?
The transmural pressure gradient is responsible for what effect during breathing?
The transmural pressure gradient is responsible for what effect during breathing?
What pressure is generally considered as atmospheric pressure at sea level?
What pressure is generally considered as atmospheric pressure at sea level?
During a single inspiration, what happens to the thoracic volume?
During a single inspiration, what happens to the thoracic volume?
What is the normal adult ventilation rate at rest?
What is the normal adult ventilation rate at rest?
Flashcards are hidden until you start studying
Study Notes
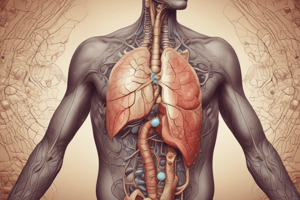
Respiratory Mechanics: Inspiration and Expiration
- Diaphragm moves downward and ribs elevate during inspiration.
- Inspiratory muscles expand thoracic cavity: external intercostals, sternocleidomastoid, anterior serrati, and scalenes.
- Phrenic nerve stimulates diaphragm to contract, leading to abdominal muscle bulging.
- External intercostals contract, lifting ribs and sternum up and out.
- Decreased intra-alveolar pressure (759 mmHg) allows air to flow into lungs.
- Intrapleural pressure decreases to allow lung expansion.
- Quiet breathing occurs at 12-20 breaths/minute in adults.
Breathing Dynamics
- Single inspiration starts at alveolar pressure equal to atmospheric pressure.
- During inspiration, thoracic volume increases, lowering alveolar pressure, which results in airflow into the lungs.
- End of inspiration reaches maximum lung volume, and intrapleural pressure decreases.
- Expiration is primarily passive; inspiratory muscles relax, diaphragm returns to dome shape, and rib cage falls due to gravity.
- Lung volume decreases as air pressure in the lungs increases, facilitating air expulsion until alveolar pressure equals atmospheric pressure.
Active Expiration
- Occurs during exercise or forced breathing.
- Involves contraction of internal intercostal and abdominal muscles to raise intra-alveolar pressure.
- Abdominal muscles push diaphragm upwards; intercostal muscles pull ribs down and inwards.
- Intrapleural pressure rises without lung collapse due to the transmural pressure gradient.
- Ventilation rates can increase to 30-40 breaths/minute during active respiration.
Pneumothorax
- Occurs when air enters the pleural cavity, leading to equalization of intrapleural and intra-alveolar pressures with atmospheric pressure.
- Loss of transmural pressure gradient causes lung collapse and thoracic wall expansion.
- Treatment involves air removal with a suction pump and sealing the puncture.
Types of Hypoxia
- Hypoxic hypoxia: Low arterial oxygen, caused by high altitude or poor ventilation.
- Anemic hypoxia: Low oxygen bound to hemoglobin due to anemia or carbon monoxide poisoning.
- Ischemic hypoxia: Reduced blood flow due to heart failure or shock.
- Histotoxic hypoxia: Cells can't use oxygen due to metabolic poisoning.
Normal Blood Values
- Arterial PO2: 95 mmHg (range 85–100)
- Venous PO2: 40 mmHg
- Arterial PCO2: 40 mmHg (range 35–45)
- Venous PCO2: 46 mmHg
- Normal blood pH: 7.4 (range 7.38–7.42)
Conditions Affecting Lung Compliance
- Emphysema: Damage to alveoli decreases lung surface area and elastic recoil, making expiration effortful.
- Chronic obstructive pulmonary disease (COPD): Includes chronic bronchitis, leading to airway inflammation and increased resistance.
- Asthma: Characterized by airway inflammation, mucus production, and muscle spasms prompting severe airway constriction.
Respiratory Resistance and Compliance
- Increased airway resistance in conditions like COPD complicates expiration.
- Normal compliance indicates the lungs can easily expand; impaired compliance results in retention of air, affecting lung mechanics.
- Surface tension from alveolar fluid, stemming from hydrogen bonding, resists lung expansion and contributes to elastic recoil after inspiration.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.