Podcast
Questions and Answers
What is the primary role of the blood-epididymis barrier?
What is the primary role of the blood-epididymis barrier?
- To increase seminal fluid production
- To enhance sperm motility
- To regulate testosterone levels
- To protect maturing sperm from the immune system (correct)
Which component is responsible for producing the majority of alkaline semen?
Which component is responsible for producing the majority of alkaline semen?
- Epididymal epithelial cells
- Prostate
- Seminal vesicles (correct)
- Ejaculatory duct
What function do prostaglandins serve in the female reproductive system?
What function do prostaglandins serve in the female reproductive system?
- Strengthening the uterine wall
- Inhibiting sperm movement
- Stimulating muscular contractions within reproductive organs (correct)
- Increasing semen viscosity
Which substance from the seminal vesicles aids in the coagulation of semen after ejaculation?
Which substance from the seminal vesicles aids in the coagulation of semen after ejaculation?
What is the main function of acid phosphatase in semen?
What is the main function of acid phosphatase in semen?
What role does zinc play in sperm function?
What role does zinc play in sperm function?
What initiates the process of semen liquefaction after ejaculation?
What initiates the process of semen liquefaction after ejaculation?
Which of the following substances is primarily produced by the prostate?
Which of the following substances is primarily produced by the prostate?
What is the main challenge in the direct measurement of reactive oxygen species (ROS)?
What is the main challenge in the direct measurement of reactive oxygen species (ROS)?
Which antioxidant contributes the most to the total antioxidant capacity (TAC) of seminal plasma?
Which antioxidant contributes the most to the total antioxidant capacity (TAC) of seminal plasma?
What types of DNA damage can occur in spermatozoa?
What types of DNA damage can occur in spermatozoa?
What is the principle behind the Comet assay?
What is the principle behind the Comet assay?
Which of the following is NOT considered an enzymatic antioxidant found in epididymal fluid?
Which of the following is NOT considered an enzymatic antioxidant found in epididymal fluid?
What can potentially result from fertilization with sperm that have DNA damages?
What can potentially result from fertilization with sperm that have DNA damages?
How do non-enzymatic antioxidants function in seminal plasma?
How do non-enzymatic antioxidants function in seminal plasma?
What role does sperm DNA integrity play in fertilization?
What role does sperm DNA integrity play in fertilization?
What does the size and intensity of the comet tail in the comet assay indicate about spermatozoa?
What does the size and intensity of the comet tail in the comet assay indicate about spermatozoa?
What color indicates good chromatin integrity in sperm when using toluidine blue staining?
What color indicates good chromatin integrity in sperm when using toluidine blue staining?
How is DNA damage assessed using CMA3 staining?
How is DNA damage assessed using CMA3 staining?
What procedure follows the preparation of a thin smear for toluidine blue staining?
What procedure follows the preparation of a thin smear for toluidine blue staining?
Which of the following statements about deep violet staining in toluidine blue is true?
Which of the following statements about deep violet staining in toluidine blue is true?
What is a significant implication of >30% DNA damage as determined by the CMA3 assay?
What is a significant implication of >30% DNA damage as determined by the CMA3 assay?
In the comet assay, where do the intact DNA fragments remain after separation?
In the comet assay, where do the intact DNA fragments remain after separation?
What is the primary purpose of the epididymis in sperm maturation?
What is the primary purpose of the epididymis in sperm maturation?
What does the cumulus expansion indicate about the oocyte?
What does the cumulus expansion indicate about the oocyte?
What stage must oocytes reach to be suitable for ICSI procedures?
What stage must oocytes reach to be suitable for ICSI procedures?
What is the role of cumulus cells surrounding the oocyte during maturation?
What is the role of cumulus cells surrounding the oocyte during maturation?
Which of the following structures is evaluated to determine oocyte quality?
Which of the following structures is evaluated to determine oocyte quality?
How are oocytes categorized as Metaphase II?
How are oocytes categorized as Metaphase II?
During which phase does the first polar body extrusion occur?
During which phase does the first polar body extrusion occur?
What type of cells differentiate into mural and cumulus cells during follicular development?
What type of cells differentiate into mural and cumulus cells during follicular development?
What role do mitochondria play in human spermatozoa?
What role do mitochondria play in human spermatozoa?
What does a high mitochondrial membrane potential (MMP) indicate when using JC-1 dye?
What does a high mitochondrial membrane potential (MMP) indicate when using JC-1 dye?
Why are oocytes at Prophase I not suitable for ICSI?
Why are oocytes at Prophase I not suitable for ICSI?
Which fertilization event is NOT directly mentioned as part of sperm function testing?
Which fertilization event is NOT directly mentioned as part of sperm function testing?
During in vitro fertilization (IVF), which barrier remains for sperm selection?
During in vitro fertilization (IVF), which barrier remains for sperm selection?
What is the JC-1 ratio used to evaluate?
What is the JC-1 ratio used to evaluate?
Which statement is true regarding sperm selection during intracytoplasmic sperm injection (ICSI)?
Which statement is true regarding sperm selection during intracytoplasmic sperm injection (ICSI)?
Which factor can indicate dysfunctional sperm despite normal morphology and motility?
Which factor can indicate dysfunctional sperm despite normal morphology and motility?
What is a common misconception about sperm selection barriers in IVF?
What is a common misconception about sperm selection barriers in IVF?
What is the primary function of prostate-specific antigen (PSA) in semen?
What is the primary function of prostate-specific antigen (PSA) in semen?
Which gland contributes 20% to the volume of semen and provides mucoid alkaline fluid?
Which gland contributes 20% to the volume of semen and provides mucoid alkaline fluid?
What is a significant cause of male infertility linked to swelling of veins above the testicle?
What is a significant cause of male infertility linked to swelling of veins above the testicle?
Which hormonal factor can negatively influence spermatogenesis in males?
Which hormonal factor can negatively influence spermatogenesis in males?
What color change in semen could indicate inflammation of the prostate?
What color change in semen could indicate inflammation of the prostate?
What does semen analysis predominantly evaluate regarding male fertility?
What does semen analysis predominantly evaluate regarding male fertility?
Which anatomical abnormality is characterized by the failure of the testes to descend into the scrotum?
Which anatomical abnormality is characterized by the failure of the testes to descend into the scrotum?
What contributes to the liquefaction of semen post-ejaculation?
What contributes to the liquefaction of semen post-ejaculation?
Flashcards
Epididymal Antioxidant Protection
Epididymal Antioxidant Protection
Cells lining the epididymis release antioxidant enzymes like superoxide dismutase, which neutralize damaging reactive oxygen species, protecting sperm from harm.
Blood-Epididymis Barrier
Blood-Epididymis Barrier
A tight barrier separates blood from the epididymis, preventing harmful substances and immune cells from reaching developing sperm cells.
Seminal Vesicle Function
Seminal Vesicle Function
Seminal vesicles contribute a majority of the semen volume, rich in fructose, an energy source for sperm, and prostaglandins, which help with sperm movement.
Seminal Prostaglandins and Immune Modulation
Seminal Prostaglandins and Immune Modulation
Signup and view all the flashcards
Semen Coagulation: Semenogelins
Semen Coagulation: Semenogelins
Signup and view all the flashcards
Semen Coagulation: Fibrinogen
Semen Coagulation: Fibrinogen
Signup and view all the flashcards
Prostate Gland Contribution
Prostate Gland Contribution
Signup and view all the flashcards
Acid Phosphatase and Sperm Activation
Acid Phosphatase and Sperm Activation
Signup and view all the flashcards
Kallikrein
Kallikrein
Signup and view all the flashcards
Prostate-specific antigen (PSA)
Prostate-specific antigen (PSA)
Signup and view all the flashcards
Cowper's gland fluid
Cowper's gland fluid
Signup and view all the flashcards
Varicocele
Varicocele
Signup and view all the flashcards
Undescended testicle (Cryptorchidism)
Undescended testicle (Cryptorchidism)
Signup and view all the flashcards
Hormonal imbalance
Hormonal imbalance
Signup and view all the flashcards
Semen analysis
Semen analysis
Signup and view all the flashcards
Macroscopic evaluation of semen
Macroscopic evaluation of semen
Signup and view all the flashcards
ROS Half-Life
ROS Half-Life
Signup and view all the flashcards
Chemiluminescence
Chemiluminescence
Signup and view all the flashcards
Fluorescence Flow Cytometry
Fluorescence Flow Cytometry
Signup and view all the flashcards
Antioxidant Capacity
Antioxidant Capacity
Signup and view all the flashcards
Enzymatic Antioxidants
Enzymatic Antioxidants
Signup and view all the flashcards
Non-Enzymatic Antioxidants
Non-Enzymatic Antioxidants
Signup and view all the flashcards
Sperm DNA Damage
Sperm DNA Damage
Signup and view all the flashcards
Comet Assay
Comet Assay
Signup and view all the flashcards
Toluidine blue staining
Toluidine blue staining
Signup and view all the flashcards
Chromomycin A3 (CMA3) staining
Chromomycin A3 (CMA3) staining
Signup and view all the flashcards
Sperm Fertilization Capacity
Sperm Fertilization Capacity
Signup and view all the flashcards
Comet tail intensity
Comet tail intensity
Signup and view all the flashcards
Percentage of Deep Violet Sperm
Percentage of Deep Violet Sperm
Signup and view all the flashcards
CMA3 DNA Damage Percentage
CMA3 DNA Damage Percentage
Signup and view all the flashcards
CMA3 Staining Intensity
CMA3 Staining Intensity
Signup and view all the flashcards
What is a secondary oocyte?
What is a secondary oocyte?
Signup and view all the flashcards
How is oocyte quality determined?
How is oocyte quality determined?
Signup and view all the flashcards
What are cumulus cells and their role?
What are cumulus cells and their role?
Signup and view all the flashcards
What does cumulus expansion indicate?
What does cumulus expansion indicate?
Signup and view all the flashcards
Why are MII oocytes suitable for ICSI?
Why are MII oocytes suitable for ICSI?
Signup and view all the flashcards
Why are MI and GV oocytes not suitable for ICSI?
Why are MI and GV oocytes not suitable for ICSI?
Signup and view all the flashcards
What are some key structures assessed during oocyte quality evaluation?
What are some key structures assessed during oocyte quality evaluation?
Signup and view all the flashcards
What does the OCCC structure tell us?
What does the OCCC structure tell us?
Signup and view all the flashcards
Sperm Activation
Sperm Activation
Signup and view all the flashcards
Sperm Mitochondria Function
Sperm Mitochondria Function
Signup and view all the flashcards
JC-1 Dye: Measuring Sperm Mitochondrial Health
JC-1 Dye: Measuring Sperm Mitochondrial Health
Signup and view all the flashcards
In Vivo Sperm Selection
In Vivo Sperm Selection
Signup and view all the flashcards
Zona Pellucida: Selective Barrier in IVF
Zona Pellucida: Selective Barrier in IVF
Signup and view all the flashcards
ICSI: Bypassing Natural Selection
ICSI: Bypassing Natural Selection
Signup and view all the flashcards
Sperm Mitochondrial Membrane Potential (MMP)
Sperm Mitochondrial Membrane Potential (MMP)
Signup and view all the flashcards
JC-1 Dye: Potential-Dependent Accumulation
JC-1 Dye: Potential-Dependent Accumulation
Signup and view all the flashcards
Study Notes
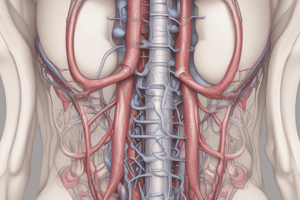
Fertility Analysis - Male Reproductive System
- The male reproductive system includes the following structures: urinary bladder, ureter, seminal vesicle, bulbourethral gland, prostate gland, ductus deferens, epididymis, testis, urethra, and glans of penis.
- Sperm is produced in the seminiferous tubules within the testes.
- The hypothalamic-pituitary-testicular axis regulates testosterone production, spermatogenesis, LH and FSH.
- GnRH (gonadotropin-releasing hormone) is synthesized by the hypothalamus and stimulates the anterior pituitary to release FSH and LH.
- FSH stimulates Sertoli cells which support spermatogenesis.
Fertility Analysis - Male Reproduction & Endocrinopathies
- Prolactin is a polypeptide hormone secreted from the anterior pituitary gland.
- Prolactin inhibits GnRH release, leading to decreased spermatogenesis and infertility in males, but this is considered pathologic.
- Normal prolactin levels in males are 2-18 ng/mL; 2-30 ng/mL in females; 10-210 ng/mL during pregnancy third trimester
- Inhibin B is a glycoprotein from the TGF-β family produced by Sertoli cells in response to FSH stimulation.
- Inhibin B controls FSH function via negative feedback and is a marker of Sertoli cell function.
- Inhibin suppresses GnRH-stimulated release of FSH.
Fertility Analysis - Male Infertility
- Varicocele: swelling of the testicular veins, contributing to 38% of male infertility cases. It results in decreased sperm count, motility, and abnormal morphology.
- Undescended testicle (Cryptorchidism): Inability of testicles to descend into the scrotum, occurring in 2-6% of newborns.
- Hormonal imbalance: Genetic conditions, gland malfunctions (hypothalamus, pituitary, thyroid, adrenal glands) and unhealthy weight can have impacts on sperm production and male fertility. Changes in LH, FSH, and testosterone levels can impact spermatogenesis.
Fertility Analysis - Evaluation of Male Infertility
- Important aspects of male infertility evaluation include: reproductive history, medical history, physical examination, semen analysis, endocrine evaluation, and advanced analysis.
Fertility Analysis - Semen Analysis
- Semen analysis is critical for assessing male fertility potential, providing a global measure of testicular/epididymal function, vasal patency and accessory sexual gland function.
- A normal semen volume is 2–6 mL after 2–7 days of abstinence.
- Color variations in semen can indicate potential issues.
- Greyish white color is considered normal, while red semen may point to prostate inflammation, and yellow/green to infections, jaundice, or vitamin/medication presence
- Aspermia: no ejaculate after orgasm; Hypospermia: under 0.5 mL of semen; Hyperspermia: over 6 mL of semen.
Fertility Analysis - Semen pH
- Normal semen pH is 7.2 - 8.2, increasing slightly after ejaculation.
- Variations in pH are typically due to prostate or seminal vesicle inflammation.
- A low semen volume and pH below 7.0 usually signals ejaculatory duct obstruction.
Fertility Analysis - Sperm Count & Morphology
- Sperm counts are reported as millions of sperm per milliliter (e.g., 15 million per mL). Total sperm count is the product of sperm concentration and semen volume.
- Conditions like normozoospermia (completely normal semen sample), oligozoospermia/oligospermia (<15 million/mL), and azoospermia (absence of sperm) are diagnosed based on total sperm count.
- Azoospermia can be obstructive or non-obstructive.
- Obstruction may be in the epididymis, vas deferens, or reproductive tract
- Non-obstruction suggests problems with sperm production or testicle structure/function.
Fertility Analysis - Sperm Motility
- Sperm motility is classified as rapid progressive, slow progressive, nonprogressive, and immotile.
- Rapid progressive motility (>25 μm/s at 37°C and >20 μm/s at 20°C) is essential for successful fertilization.
- For proper semen analysis at least 32% of sperm must be graded A and B (rapidly progressive motile spermatozoa).
- Reduced sperm motility may be a symptom of issues related to male accessory sex gland secretion or emptying.
- Asthenozoospermia describes the condition of reduced sperm motility due to various factors such as poor nutrition, varicocele, toxins, smoking, age, cancer treatments, and febrile episodes, among others.
Fertility Analysis - Sperm Viability & Necrosis
- Vitality is assessed through staining methods when sperm motility is less than 40%.
- Necrozoospermia refers to dead/necrotic sperm in a semen sample.
- Normal semen samples contain less than 30% necrotic sperm. Moderate necrozoospermia is 50-80% and Severe necrozoospermia is over 80%. Complete necrozoospermia involves almost all cells being dead/necrotic.
Fertility Analysis - Sperm Morphology
- Sperm morphology quantitatively evaluates normal and abnormal sperm forms in an ejaculate using WHO classification.
- Abnormalities are based on head, tail, and mid-piece characteristics from postcoital cervical mucus or zona pellucida surface.
- Teratozoospermia describes an increased percentage of abnormal sperm morphology in the semen exceeding 96%.
Fertility Analysis - Biochemical Markers (Semen)
- Fructose test assesses seminal vesicle function and is used to identify obstructive azoospermia in males with low ejaculate volume.
- Low levels of fructose (WHO defined lower limit 13 µmol per ejaculate) with low semen volume and low pH supports obstructive azoospermia diagnosis.
- Endtz test detects peroxidase within the neutrophils in a semen sample. This supports screening for granulocytes in unusual conditions.
Fertility Analysis - Biochemical Markers (Blood)
- Testosterone levels (300-1000 ng/dL) vary daily (best measured 8 AM-10 AM) and decline approximately 1% per year after age 35.
- Hypogonadism is defined as a serum testosterone level under 300 ng/dL, exhibiting various physical signs like increased body fat, reduced strength and muscle bulk, low bone mineral density, decreased energy/motivation and libido among other symptoms.
- Prolactin levels in males range from 2-18 ng/mL. Mild elevations don't typically cause infertility, while significant elevations can inhibit FSH & LH release from the pituitary gland, decreasing testosterone levels.
Fertility Analysis - Oxidative Stress & Antioxidant Capacity
- ROS (reactive oxygen species) refers to oxygen metabolism by-products.
- Free radicals, including superoxide and hydroxyl radicals, indicate potential oxidative stress due to unpaired electrons.
- Antioxidant capacity of seminal plasma includes enzymatic antioxidants and non-enzymatic antioxidants such as vitamin C, E and zinc, with non-enzymatic antioxidants contributing to about 65% of the total antioxidant capacity (TAC)
Fertility Analysis - Sperm DNA Damage
- Sperm DNA integrity is crucial for fertilization and transmitting genetic material.
- DNA Damage includes single or double stranded breaks, interstrand and intrastrand cross-linkage, DNA base modifications and protamine mispackaging. Often termed as DNA fragmentation
- Procedures like the Comet assay (a single-cell gel electrophoresis) can be used to measure DNA breaks in sperm.
Fertility Analysis - Oocyte & Sperm Assessment
- Oocyte maturation includes nuclear and cytoplasmic maturation.
- Mature eggs arrest in metaphase II until fertilization.
- Oocyte quality can be assessed through OCCC structure (measuring cumulus expansion for potential fertilization success), zona pellucida and polar body morphology.
- The hypo-osmotic swelling test (HOST) detects sperm viability issues, especially in samples with testicular or epididymal aspiration. PVP (Polyvinylpyrrolidone) is a common immobilization medium for ICSI, but may damage mitochondria
Fertility Analysis - Physical Exams
- Breast evaluation for symmetry, noting any evidence of galactorrhea (abnormal secretion from the breasts) which could point to pituitary lesions, in a fertility evaluation. Galactorrhea commonly involves bilateral multiple duct discharges in appearance.
- Hysterosalpingogram (HSG) checks fallopian tube patency and uterine cavity for normal function.
- Antral Follicle Count (AFC) evaluates the number or recruited follicles from both ovaries in the earlier phase of the cycle via ultrasound. It serves as a marker for ovarian reserve. Folliculometry tracks follicle growth and ovulation timing for 9-20 days into the cycle, to confirm that ovulation has occurred.
- Chlamydia antibody testing checks for previous infection as a cause of potential salpingitis (inflammation of the fallopian tubes.) This accounts for over 50% of tubal factor infertility.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.