Podcast
Questions and Answers
Which of the following is NOT a characteristic of peripheral nerves?
Which of the following is NOT a characteristic of peripheral nerves?
- They are bundles of nerve fibers.
- They are all similar in structure.
- They are always myelinated. (correct)
- They conduct impulses from one part of the body to another.
What is the basic unit of all nerves?
What is the basic unit of all nerves?
- Axon
- Neuron (correct)
- Schwann cell
- Myelin sheath
What is the function of the neurotransmitters released at the terminal enlargements of nociceptive afferent neurons?
What is the function of the neurotransmitters released at the terminal enlargements of nociceptive afferent neurons?
- To prevent the release of sensitizing chemicals
- To conduct impulses to the CNS
- To activate effector organs (correct)
- To provide structural support for the neuron
What are the three types of fibers found in peripheral nerves?
What are the three types of fibers found in peripheral nerves?
Which of the following is NOT a type of peripheral nerve based on anatomical location?
Which of the following is NOT a type of peripheral nerve based on anatomical location?
Which of the following statements accurately describes the role of the Na+/K+ pump in maintaining the resting membrane potential?
Which of the following statements accurately describes the role of the Na+/K+ pump in maintaining the resting membrane potential?
What is the primary function of the proteins embedded within the lipid bilayer of a nerve cell membrane?
What is the primary function of the proteins embedded within the lipid bilayer of a nerve cell membrane?
What happens during the depolarization phase of an action potential?
What happens during the depolarization phase of an action potential?
What is the threshold level in the context of an action potential?
What is the threshold level in the context of an action potential?
How do local anesthetics work to block the propagation of nerve impulses?
How do local anesthetics work to block the propagation of nerve impulses?
Which ion movement is responsible for the depolarization phase of an action potential?
Which ion movement is responsible for the depolarization phase of an action potential?
What is the primary role of the inward sodium ($Na^+$) current in the action potential?
What is the primary role of the inward sodium ($Na^+$) current in the action potential?
Which of the following is TRUE regarding the repolarization phase of an action potential?
Which of the following is TRUE regarding the repolarization phase of an action potential?
What is the relationship between the outward potassium ($K^+$) current and the rate of repolarization?
What is the relationship between the outward potassium ($K^+$) current and the rate of repolarization?
What is the main difference between the inward sodium ($Na^+$) current and the outward potassium ($K^+$) current in terms of their role in the action potential?
What is the main difference between the inward sodium ($Na^+$) current and the outward potassium ($K^+$) current in terms of their role in the action potential?
Which of these local anesthetics is classified as an amide?
Which of these local anesthetics is classified as an amide?
Which of the following is NOT a factor influencing plasma concentration of local anesthetics?
Which of the following is NOT a factor influencing plasma concentration of local anesthetics?
What is the maximum safe dose of bupivacaine for a 70 kg patient?
What is the maximum safe dose of bupivacaine for a 70 kg patient?
Which of the following is an early sign of local anesthetic systemic toxicity (LAST)?
Which of the following is an early sign of local anesthetic systemic toxicity (LAST)?
What is the recommended treatment for hypotension associated with spinal anesthesia?
What is the recommended treatment for hypotension associated with spinal anesthesia?
Which of the following is a common complication of spinal anesthesia?
Which of the following is a common complication of spinal anesthesia?
How long should a patient discontinue taking clopidogrel (Plavix) before undergoing a neuraxial block?
How long should a patient discontinue taking clopidogrel (Plavix) before undergoing a neuraxial block?
What is the mechanism by which spinal anesthesia causes hypotension?
What is the mechanism by which spinal anesthesia causes hypotension?
What is the recommended hold time for low-dose LMWH (Lovenox) before placing or removing a neuraxial catheter?
What is the recommended hold time for low-dose LMWH (Lovenox) before placing or removing a neuraxial catheter?
Which of the following is a true statement regarding the Bezold-Jarisch reflex?
Which of the following is a true statement regarding the Bezold-Jarisch reflex?
Which of the following medications is contraindicated within 4 weeks of surgery due to its potential for bleeding complications?
Which of the following medications is contraindicated within 4 weeks of surgery due to its potential for bleeding complications?
What is the recommended dose of lidocaine for a spinal anesthetic to T10?
What is the recommended dose of lidocaine for a spinal anesthetic to T10?
What is the recommended hold time for intravenous heparin (high dose >20,000 daily) before placing a neuraxial catheter?
What is the recommended hold time for intravenous heparin (high dose >20,000 daily) before placing a neuraxial catheter?
What is the typical onset of sensory block with a 3% chloroprocaine epidural?
What is the typical onset of sensory block with a 3% chloroprocaine epidural?
Which of the following signs or symptoms is NOT typically associated with inadvertent intrathecal placement of lidocaine during a spinal injection?
Which of the following signs or symptoms is NOT typically associated with inadvertent intrathecal placement of lidocaine during a spinal injection?
Which of the following medications is contraindicated in the treatment of LAST?
Which of the following medications is contraindicated in the treatment of LAST?
What is the recommended hold time for ginseng before a regional anesthesia procedure?
What is the recommended hold time for ginseng before a regional anesthesia procedure?
What is the recommended initial dose for an epidural anesthetic?
What is the recommended initial dose for an epidural anesthetic?
What is the purpose of a test dose for epidural anesthesia?
What is the purpose of a test dose for epidural anesthesia?
What is the recommended hold time for dabigatran (Pradaxa) before placing a neuraxial catheter?
What is the recommended hold time for dabigatran (Pradaxa) before placing a neuraxial catheter?
What is the recommended restarting time for low-dose LMWH after removal of a neuraxial catheter?
What is the recommended restarting time for low-dose LMWH after removal of a neuraxial catheter?
Which of the following is a common treatment for postdural puncture headache?
Which of the following is a common treatment for postdural puncture headache?
What is the recommended dose of intralipid for a 60 kg patient with LAST who is unresponsive to standard resuscitation procedures?
What is the recommended dose of intralipid for a 60 kg patient with LAST who is unresponsive to standard resuscitation procedures?
Which of the following medications is associated with an increased risk of bleeding when used in conjunction with neuraxial blocks?
Which of the following medications is associated with an increased risk of bleeding when used in conjunction with neuraxial blocks?
What is the appropriate action if blood is found in the catheter during neuraxial placement?
What is the appropriate action if blood is found in the catheter during neuraxial placement?
What is the primary mechanism of hypotension associated with spinal anesthesia?
What is the primary mechanism of hypotension associated with spinal anesthesia?
Which local anesthetic is typically used for short-acting spinal anesthesia at a 10% concentration?
Which local anesthetic is typically used for short-acting spinal anesthesia at a 10% concentration?
Which local anesthetic is known for its rapid onset and long duration of action, particularly when administered for spinal anesthesia?
Which local anesthetic is known for its rapid onset and long duration of action, particularly when administered for spinal anesthesia?
What is the primary application of Chloroprocaine, as mentioned in the text?
What is the primary application of Chloroprocaine, as mentioned in the text?
Which local anesthetic is the most widely used and has a broad range of applications, including infiltration, peripheral nerve blocks, spinal, and epidural anesthesia?
Which local anesthetic is the most widely used and has a broad range of applications, including infiltration, peripheral nerve blocks, spinal, and epidural anesthesia?
Which local anesthetic is known for its low potency, slow onset, and short duration of action, making it less frequently utilized for peripheral nerve blocks or epidurals?
Which local anesthetic is known for its low potency, slow onset, and short duration of action, making it less frequently utilized for peripheral nerve blocks or epidurals?
Which of these local anesthetics is a hyperbaric solution that requires mixing with 10% glucose?
Which of these local anesthetics is a hyperbaric solution that requires mixing with 10% glucose?
What is the reason all local anesthetics have a faster onset when administered for spinal anesthesia, compared to other methods like peripheral nerve blocks?
What is the reason all local anesthetics have a faster onset when administered for spinal anesthesia, compared to other methods like peripheral nerve blocks?
Which local anesthetic is commonly used for urologic procedures, as mentioned in the text?
Which local anesthetic is commonly used for urologic procedures, as mentioned in the text?
Flashcards
Fluid Mosaic Membrane
Fluid Mosaic Membrane
A cell membrane structure made of phospholipid bilayer with embedded proteins.
Hydrophilic and Hydrophobic
Hydrophilic and Hydrophobic
Hydrophilic substances attract water, while hydrophobic substances repel it.
Resting Membrane Potential
Resting Membrane Potential
The voltage potential across a cell's membrane when it's not actively firing, usually around -70mV.
Na+/K+ Pump
Na+/K+ Pump
Signup and view all the flashcards
Depolarization and Repolarization
Depolarization and Repolarization
Signup and view all the flashcards
Nociceptive Afferent Neurons
Nociceptive Afferent Neurons
Signup and view all the flashcards
Peripheral Nerves
Peripheral Nerves
Signup and view all the flashcards
Mixed Nerves
Mixed Nerves
Signup and view all the flashcards
Sensitizing Chemicals
Sensitizing Chemicals
Signup and view all the flashcards
Neuron Structure
Neuron Structure
Signup and view all the flashcards
Inward Na+ current
Inward Na+ current
Signup and view all the flashcards
Outward K+ current
Outward K+ current
Signup and view all the flashcards
Depolarization
Depolarization
Signup and view all the flashcards
Repolarization
Repolarization
Signup and view all the flashcards
Action potential
Action potential
Signup and view all the flashcards
Procaine
Procaine
Signup and view all the flashcards
Chloroprocaine
Chloroprocaine
Signup and view all the flashcards
Tetracaine
Tetracaine
Signup and view all the flashcards
Lidocaine
Lidocaine
Signup and view all the flashcards
Epidural Anesthesia
Epidural Anesthesia
Signup and view all the flashcards
Systemic Toxicity
Systemic Toxicity
Signup and view all the flashcards
Hypobaric and Hyperbaric Solutions
Hypobaric and Hyperbaric Solutions
Signup and view all the flashcards
Duration of Action
Duration of Action
Signup and view all the flashcards
Inadvertent Intrathecal Placement
Inadvertent Intrathecal Placement
Signup and view all the flashcards
Rapid Spinal Block Symptoms
Rapid Spinal Block Symptoms
Signup and view all the flashcards
Inadvertent Intravascular Placement
Inadvertent Intravascular Placement
Signup and view all the flashcards
Epinephrine As Marker
Epinephrine As Marker
Signup and view all the flashcards
Aspirin and NSAIDs Safety
Aspirin and NSAIDs Safety
Signup and view all the flashcards
Clopidogrel (Plavix) Guidelines
Clopidogrel (Plavix) Guidelines
Signup and view all the flashcards
Dabigatran (Pradaxa) Timing
Dabigatran (Pradaxa) Timing
Signup and view all the flashcards
IV Heparin Timing
IV Heparin Timing
Signup and view all the flashcards
Low Molecular Weight Heparin (LMWH)
Low Molecular Weight Heparin (LMWH)
Signup and view all the flashcards
Spinal Procedure Preparation
Spinal Procedure Preparation
Signup and view all the flashcards
Serum Concentration Factors
Serum Concentration Factors
Signup and view all the flashcards
Local Anesthetic Toxicity
Local Anesthetic Toxicity
Signup and view all the flashcards
Early Signs of LAST
Early Signs of LAST
Signup and view all the flashcards
Late Signs of LAST
Late Signs of LAST
Signup and view all the flashcards
Cardiovascular Effects of LA
Cardiovascular Effects of LA
Signup and view all the flashcards
Cardiac Response Sequence
Cardiac Response Sequence
Signup and view all the flashcards
Treatment for LAST
Treatment for LAST
Signup and view all the flashcards
Spinal Anesthesia Drug Doses
Spinal Anesthesia Drug Doses
Signup and view all the flashcards
Epidural Anesthesia Initial Dose
Epidural Anesthesia Initial Dose
Signup and view all the flashcards
Post-Dural Puncture Headache (PDPH)
Post-Dural Puncture Headache (PDPH)
Signup and view all the flashcards
Cauda Equina Syndrome
Cauda Equina Syndrome
Signup and view all the flashcards
Bezold-Jarisch Reflex
Bezold-Jarisch Reflex
Signup and view all the flashcards
Test Dose for Epidural Anesthesia
Test Dose for Epidural Anesthesia
Signup and view all the flashcards
Sympathectomy Effects
Sympathectomy Effects
Signup and view all the flashcards
Study Notes
Regional Exam 1 Objectives - Anatomy and Physiology
- Identify anatomical landmarks for neuraxial anesthesia (spinal, epidural, caudal).
- C7: Most prominent cervical spinal process.
- T7: Opposite the inferior angle of the scapula.
- L4-L5: Line connecting the iliac crests (Tuffier's line).
- Lumbar region (midline): Skin to Tuffier's line = 4-6 cm.
- Tuffier's line = 5-6 mm (0.5 cm) thick.
- Epidural space in the sacral region (caudal space): Sacral portion of the epidural space.
- Needle inserted through sacrococcygeal ligament into the sacral hiatus.
- Sacral hiatus: Notch above the coccyx, between sacral cornua.
- Landmarks for caudal epidural space: Easier in children, more difficult/impossible in adults (calcification).
Spinal Anatomy: Midline Approach
- Skin.
- Subcutaneous tissue.
- Supraspinous ligament.
- Intraspinous ligament.
- Ligamentum flavum.
- Dura mater.
- Subdural space.
- Subarachnoid space.
- Arachnoid mater.
Spinal Anatomy: Paramedian Approach
- Similar to midline approach but from a paramedian position.
- Stops at ligamentum flavum, before the dura mater.
Spinal Curvature and Neuraxial Anesthesia
-
Spinal curvature in supine position:
- High points/apex (lordosis): C5 and L3-L5.
- Low points/trough (kyphosis): T4-T7 and S2.
-
Scoliosis: Lateral curvature of the spine.
-
Kyphosis: Excessive posterior curve.
-
Lordosis: Hollowing of the back (in obesity/pregnancy).
Spinal Anesthesia - Factors Affecting Local Anesthetic Spread
- Local anesthetic uptake from the subarachnoid space into neuronal tissue affected by 4 factors.
- Concentration in CSF.
- Dose of Local Anesthetic (LA).
- Density of LA in relation to CSF (hypobaric, isobaric, hyperbaric).
- Flow in CSF column.
Spinal Anesthesia - Dermatomal Levels and Clinical Relevance
- Dermatomes: Area of skin innervated by a single spinal nerve.
- T10: Umbilicus.
- T6: Xiphoid process.
- T4: Nipples.
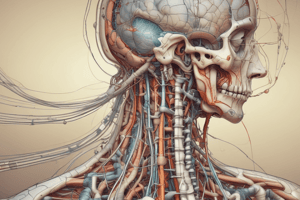
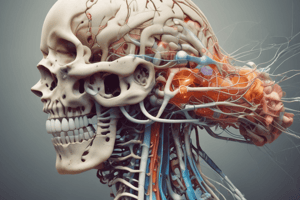
Peripheral Nerve Anatomy
- Peripheral nerves are bundles of nerve fibers (axons).
- Connective tissue layers organize nerve fibers into fascicles.
- Endoneurium: Surrounds individual nerve fibers.
- Perineurium: Surrounds fascicles.
- Epineurium: Covers the entire nerve.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.