Podcast
Questions and Answers
What is the characteristic appearance of asbestos bodies in the lung?
What is the characteristic appearance of asbestos bodies in the lung?
- Glassy and beaded rods with a golden brown color (correct)
- Rod-shaped and beaded fibers with a silver color
- Fibrous and beaded rods with a dark brown color
- Fibrous and coiled rods with a white color
What is the primary site of asbestos-induced disease?
What is the primary site of asbestos-induced disease?
- Visceral pleura
- Lung parenchyma
- Pleura (correct)
- Skin
What is the term used to describe the asbestos-induced formation of scar tissue in the lung?
What is the term used to describe the asbestos-induced formation of scar tissue in the lung?
- Granuloma
- Asbestosis (correct)
- Pleural plaque
- Fibrosis
In which of the following sites are asbestos bodies NOT typically found?
In which of the following sites are asbestos bodies NOT typically found?
What is the characteristic feature of asbestos-induced pleural disease?
What is the characteristic feature of asbestos-induced pleural disease?
Which of the following is a common feature of asbestos-induced disease?
Which of the following is a common feature of asbestos-induced disease?
What is the term used to describe the type of collagen deposited in asbestos-induced disease?
What is the term used to describe the type of collagen deposited in asbestos-induced disease?
What is the characteristic appearance of asbestos-induced pleural plaques?
What is the characteristic appearance of asbestos-induced pleural plaques?
What is the primary characteristic of the lung surface in patients with "cobblestoned" lungs?
What is the primary characteristic of the lung surface in patients with "cobblestoned" lungs?
Which of the following statements accurately describes the survival rates in patients diagnosed with "cobblestoned" lungs?
Which of the following statements accurately describes the survival rates in patients diagnosed with "cobblestoned" lungs?
What is the primary underlying microscopic feature observed in patients with "cobblestoned" lungs?
What is the primary underlying microscopic feature observed in patients with "cobblestoned" lungs?
What is the primary treatment approach for patients with "cobblestoned" lungs?
What is the primary treatment approach for patients with "cobblestoned" lungs?
Which of the following conditions is NOT mentioned as a potential cause of "cobblestoned" lungs?
Which of the following conditions is NOT mentioned as a potential cause of "cobblestoned" lungs?
What is the significance of early and late "cobblestone" lesions in the differential diagnosis?
What is the significance of early and late "cobblestone" lesions in the differential diagnosis?
What is the implication of the statement that "cobblestone" lesions "become more collagenous and less cellular over time"?
What is the implication of the statement that "cobblestone" lesions "become more collagenous and less cellular over time"?
What is the main reason why "cobblestone" lesions should be carefully considered in the differential diagnosis of pulmonary fibrosis?
What is the main reason why "cobblestone" lesions should be carefully considered in the differential diagnosis of pulmonary fibrosis?
What major health condition is estimated to cause 50,000 deaths per year in the United States?
What major health condition is estimated to cause 50,000 deaths per year in the United States?
In hypoxemia, which condition is likely a result of decreased cardiac output?
In hypoxemia, which condition is likely a result of decreased cardiac output?
What fraction of hospitalized patients are diagnosed with a specific condition related to hypoxemia?
What fraction of hospitalized patients are diagnosed with a specific condition related to hypoxemia?
Which complication is associated with hypoxemia according to the content?
Which complication is associated with hypoxemia according to the content?
What is the incidence of pulmonary embolism as described in the passage?
What is the incidence of pulmonary embolism as described in the passage?
What diagnostic challenge is highlighted regarding patients with hypoxemia?
What diagnostic challenge is highlighted regarding patients with hypoxemia?
What is the potential consequence of a large embolus lodging in the pulmonary artery bifurcation?
What is the potential consequence of a large embolus lodging in the pulmonary artery bifurcation?
What is the primary reason for prolonged bed rest being a risk factor for pulmonary embolism?
What is the primary reason for prolonged bed rest being a risk factor for pulmonary embolism?
Which of the following is NOT a potential source of antigens causing hypersensitivity pneumonitis?
Which of the following is NOT a potential source of antigens causing hypersensitivity pneumonitis?
What is the most likely outcome for a small embolus lodging in a medium-sized pulmonary artery?
What is the most likely outcome for a small embolus lodging in a medium-sized pulmonary artery?
Which of the following is a potential consequence of ischemic damage to the lung tissue due to a pulmonary embolism?
Which of the following is a potential consequence of ischemic damage to the lung tissue due to a pulmonary embolism?
What is the primary mechanism by which a pulmonary embolism causes death?
What is the primary mechanism by which a pulmonary embolism causes death?
Which of the following is NOT a typical symptom of a pulmonary embolism?
Which of the following is NOT a typical symptom of a pulmonary embolism?
What is the significance of the term 'saddle embolus' in relation to pulmonary embolism?
What is the significance of the term 'saddle embolus' in relation to pulmonary embolism?
Which of the following is NOT a contributing factor to the development of pulmonary fibrosis, according to the passage?
Which of the following is NOT a contributing factor to the development of pulmonary fibrosis, according to the passage?
What is the primary function of surfactant in the context of pulmonary fibrosis?
What is the primary function of surfactant in the context of pulmonary fibrosis?
According to the passage, what is the role of telomerase mutations in the development of pulmonary fibrosis?
According to the passage, what is the role of telomerase mutations in the development of pulmonary fibrosis?
Which of the following correctly describes the sequence of events leading to pulmonary fibrosis, as explained in the passage?
Which of the following correctly describes the sequence of events leading to pulmonary fibrosis, as explained in the passage?
What is the primary function of the inflammasome in the context of pulmonary fibrosis?
What is the primary function of the inflammasome in the context of pulmonary fibrosis?
Which of the following is NOT directly mentioned in the passage as a consequence of chronic inflammation in the lungs?
Which of the following is NOT directly mentioned in the passage as a consequence of chronic inflammation in the lungs?
What is the primary difference between the innate and adaptive immune response in the context of this passage?
What is the primary difference between the innate and adaptive immune response in the context of this passage?
What is the primary role of the MUC5B variant in the development of pulmonary fibrosis?
What is the primary role of the MUC5B variant in the development of pulmonary fibrosis?
In addition, chronic inflammation may lead to a decrease in the production of collagen in the lung tissue.
In addition, chronic inflammation may lead to a decrease in the production of collagen in the lung tissue.
Asbestos bodies are typically found in the liver.
Asbestos bodies are typically found in the liver.
Tobacco smoking has a neutral effect on the development of fibrogenic diseases.
Tobacco smoking has a neutral effect on the development of fibrogenic diseases.
Coal workers' pneumoconiosis has increased in incidence as work in coal mines has decreased.
Coal workers' pneumoconiosis has increased in incidence as work in coal mines has decreased.
Asbestosis and silicosis are both examples of hypoxemic disorders.
Asbestosis and silicosis are both examples of hypoxemic disorders.
The primary site of asbestos-induced disease is the brain.
The primary site of asbestos-induced disease is the brain.
The formation of scar tissue in the lung is a protective mechanism against asbestos-induced damage.
The formation of scar tissue in the lung is a protective mechanism against asbestos-induced damage.
Asbestos-induced pleural disease is typically benign and asymptomatic.
Asbestos-induced pleural disease is typically benign and asymptomatic.
Asbestos bodies are a characteristic feature of silicosis.
Asbestos bodies are a characteristic feature of silicosis.
The primary mechanism by which asbestos induces fibrogenic disease is through the deposition of collagen.
The primary mechanism by which asbestos induces fibrogenic disease is through the deposition of collagen.
Asbestos-induced pleural disease is typically characterized by the formation of scar tissue in the lung.
Asbestos-induced pleural disease is typically characterized by the formation of scar tissue in the lung.
Asbestos-induced granulomas are surrounded by a zone of CD8+ T cells.
Asbestos-induced granulomas are surrounded by a zone of CD8+ T cells.
Silica, asbestos, and beryllium are more reactive than coal dust, resulting in a lower concentration of fibrotic reactions.
Silica, asbestos, and beryllium are more reactive than coal dust, resulting in a lower concentration of fibrotic reactions.
The formation of granulomas in response to asbestos is a protective mechanism against fibrogenic disease.
The formation of granulomas in response to asbestos is a protective mechanism against fibrogenic disease.
Asbestos-induced fibrogenic disease is typically asymptomatic.
Asbestos-induced fibrogenic disease is typically asymptomatic.
Telomerase mutations, surfactant mutations, and the MUC5B variant are all genetic factors that contribute to the development of pulmonary fibrosis.
Telomerase mutations, surfactant mutations, and the MUC5B variant are all genetic factors that contribute to the development of pulmonary fibrosis.
The inflammatory response to inhaled particles, such as silica, asbestos, and beryllium, is primarily driven by the innate immune system.
The inflammatory response to inhaled particles, such as silica, asbestos, and beryllium, is primarily driven by the innate immune system.
The primary site of asbestos-induced disease is the liver.
The primary site of asbestos-induced disease is the liver.
The inflammasome is a protein complex that is activated by phagocytosis of particles, leading to the release of cytokines such as IL-1, which further amplifies the inflammatory response.
The inflammasome is a protein complex that is activated by phagocytosis of particles, leading to the release of cytokines such as IL-1, which further amplifies the inflammatory response.
Tobacco smoking has a synergistic effect on the development of asbestos-induced fibrogenic disease.
Tobacco smoking has a synergistic effect on the development of asbestos-induced fibrogenic disease.
The MUC5B variant increases mucus production in the lungs, which can help to trap inhaled particles and prevent them from reaching the alveoli.
The MUC5B variant increases mucus production in the lungs, which can help to trap inhaled particles and prevent them from reaching the alveoli.
Persistent epithelial injury and activation of the innate and adaptive immune responses are key factors in the development of pulmonary fibrosis.
Persistent epithelial injury and activation of the innate and adaptive immune responses are key factors in the development of pulmonary fibrosis.
The inflammatory response triggered by silica, asbestos, and beryllium results in the production of cytokines such as IL-1, which promote tissue repair and fibrosis.
The inflammatory response triggered by silica, asbestos, and beryllium results in the production of cytokines such as IL-1, which promote tissue repair and fibrosis.
Pulmonary fibrosis is a progressive disease that is characterized by the formation of scar tissue in the lungs, which can lead to respiratory failure.
Pulmonary fibrosis is a progressive disease that is characterized by the formation of scar tissue in the lungs, which can lead to respiratory failure.
Asbestos bodies are usually asymptomatic and detected by polarized microscopy, revealing birefringent silica on radiographs as circumscribed densities.
Asbestos bodies are usually asymptomatic and detected by polarized microscopy, revealing birefringent silica on radiographs as circumscribed densities.
The risk of developing lung carcinoma is about fivefold higher for asbestos workers compared to the general population.
The risk of developing lung carcinoma is about fivefold higher for asbestos workers compared to the general population.
The risk of developing mesothelioma is 1000 times greater for asbestos workers compared to individuals not exposed to asbestos.
The risk of developing mesothelioma is 1000 times greater for asbestos workers compared to individuals not exposed to asbestos.
The risk of lung cancer is significantly increased in asbestos workers who also smoke cigarettes, while the risk of mesothelioma remains unchanged.
The risk of lung cancer is significantly increased in asbestos workers who also smoke cigarettes, while the risk of mesothelioma remains unchanged.
The characteristic sign of asbestosis on chest x-ray is a fine nodularity in the upper lung zones.
The characteristic sign of asbestosis on chest x-ray is a fine nodularity in the upper lung zones.
Asbestosis, a lung disease caused by asbestos exposure, is primarily characterized by the formation of dense collagenous scar tissue in the lung parenchyma.
Asbestosis, a lung disease caused by asbestos exposure, is primarily characterized by the formation of dense collagenous scar tissue in the lung parenchyma.
Asbestosis can manifest as "cobblestone" lesions, which are small, circumscribed nodules of fibrotic tissue that coalesce and become more cellular over time.
Asbestosis can manifest as "cobblestone" lesions, which are small, circumscribed nodules of fibrotic tissue that coalesce and become more cellular over time.
The risk of developing "cobblestone" lesions is significantly reduced in asbestos workers who also smoke cigarettes.
The risk of developing "cobblestone" lesions is significantly reduced in asbestos workers who also smoke cigarettes.
In about two-thirds of cases, the onset of symptoms related to asbestos exposure is gradual.
In about two-thirds of cases, the onset of symptoms related to asbestos exposure is gradual.
The presence of asbestos bodies in the lung tissue is a definitive indicator of asbestos-related disease.
The presence of asbestos bodies in the lung tissue is a definitive indicator of asbestos-related disease.
Pleural plaques, a hallmark of asbestos-related disease, are typically small and easily missed on imaging studies.
Pleural plaques, a hallmark of asbestos-related disease, are typically small and easily missed on imaging studies.
Asbestos exposure primarily affects the upper respiratory tract, leading to conditions like laryngitis and sinusitis.
Asbestos exposure primarily affects the upper respiratory tract, leading to conditions like laryngitis and sinusitis.
The term "cobblestoned lungs" refers to a condition where the lung surface is characterized by small, smooth, and evenly spaced nodules.
The term "cobblestoned lungs" refers to a condition where the lung surface is characterized by small, smooth, and evenly spaced nodules.
The presence of "cobblestone" lesions in the lungs is a strong indicator of asbestos-related disease, as this pattern is specific to asbestos exposure.
The presence of "cobblestone" lesions in the lungs is a strong indicator of asbestos-related disease, as this pattern is specific to asbestos exposure.
The "cobblestone" lesions observed in the lungs tend to become more collagenous and less cellular over time, making them more difficult to treat.
The "cobblestone" lesions observed in the lungs tend to become more collagenous and less cellular over time, making them more difficult to treat.
The development of "cobblestone" lesions in the lungs is a rapid process that occurs within a few weeks of exposure to asbestos.
The development of "cobblestone" lesions in the lungs is a rapid process that occurs within a few weeks of exposure to asbestos.
What is the characteristic feature of idiopathic pulmonary fibrosis in terms of age?
What is the characteristic feature of idiopathic pulmonary fibrosis in terms of age?
What is the primary site where the affected genes are expressed in idiopathic pulmonary fibrosis?
What is the primary site where the affected genes are expressed in idiopathic pulmonary fibrosis?
What is the characteristic symptom of idiopathic pulmonary fibrosis?
What is the characteristic symptom of idiopathic pulmonary fibrosis?
What is the significance of 'dry' or 'Velcro-like' crackles in idiopathic pulmonary fibrosis?
What is the significance of 'dry' or 'Velcro-like' crackles in idiopathic pulmonary fibrosis?
What is the potential consequence of idiopathic pulmonary fibrosis in advanced stages?
What is the potential consequence of idiopathic pulmonary fibrosis in advanced stages?
What is the role of MUC5B in idiopathic pulmonary fibrosis?
What is the role of MUC5B in idiopathic pulmonary fibrosis?
What is the primary difference between idiopathic pulmonary fibrosis and other fibrotic diseases?
What is the primary difference between idiopathic pulmonary fibrosis and other fibrotic diseases?
What is the significance of telomerase mutations in idiopathic pulmonary fibrosis?
What is the significance of telomerase mutations in idiopathic pulmonary fibrosis?
What is the primary reason why asbestos exposure increases the risk of developing pleural plaques and lung carcinoma?
What is the primary reason why asbestos exposure increases the risk of developing pleural plaques and lung carcinoma?
What is the characteristic feature of asbestos-induced pleural plaques on radiographs?
What is the characteristic feature of asbestos-induced pleural plaques on radiographs?
How does the risk of developing mesothelioma increase in asbestos workers?
How does the risk of developing mesothelioma increase in asbestos workers?
What is the effect of concomitant cigarette smoking on the risk of developing lung carcinoma in asbestos workers?
What is the effect of concomitant cigarette smoking on the risk of developing lung carcinoma in asbestos workers?
What is the characteristic feature of asbestos-induced lung disease on radiographs?
What is the characteristic feature of asbestos-induced lung disease on radiographs?
What is the primary mechanism by which asbestos induces fibrogenic disease?
What is the primary mechanism by which asbestos induces fibrogenic disease?
How does the risk of developing asbestos-induced lung disease change over time?
How does the risk of developing asbestos-induced lung disease change over time?
What is the significance of asbestos bodies in the diagnosis of asbestos-induced lung disease?
What is the significance of asbestos bodies in the diagnosis of asbestos-induced lung disease?
Explain why the size, shape, solubility, and reactivity of particles are crucial factors in determining the potential for lung damage due to dust exposure.
Explain why the size, shape, solubility, and reactivity of particles are crucial factors in determining the potential for lung damage due to dust exposure.
Describe the characteristics of coal dust that make it relatively inert and less likely to cause lung disease compared to other types of dust.
Describe the characteristics of coal dust that make it relatively inert and less likely to cause lung disease compared to other types of dust.
Based on the passage, why are particles between 1 and 5 micrometers in diameter considered particularly dangerous in terms of lung damage?
Based on the passage, why are particles between 1 and 5 micrometers in diameter considered particularly dangerous in terms of lung damage?
Explain the concept of 'at-risk epithelium' and its significance in the development of lung diseases.
Explain the concept of 'at-risk epithelium' and its significance in the development of lung diseases.
Describe the connection between chronic inflammation and the development of pulmonary fibrosis. Explain why this process is often irreversible.
Describe the connection between chronic inflammation and the development of pulmonary fibrosis. Explain why this process is often irreversible.
What is the role of surfactant in the context of pulmonary fibrosis, and how does its impairment contribute to the disease progression?
What is the role of surfactant in the context of pulmonary fibrosis, and how does its impairment contribute to the disease progression?
Explain how telomerase mutations might contribute to the development of pulmonary fibrosis. What does this suggest about the potential role of genetic factors in this disease?
Explain how telomerase mutations might contribute to the development of pulmonary fibrosis. What does this suggest about the potential role of genetic factors in this disease?
Discuss the differences between the innate and adaptive immune responses in the context of pulmonary fibrosis. Explain how both types of responses can contribute to disease progression.
Discuss the differences between the innate and adaptive immune responses in the context of pulmonary fibrosis. Explain how both types of responses can contribute to disease progression.
What are the primary diseases associated with exposure to coal dust?
What are the primary diseases associated with exposure to coal dust?
Identify two common occupational exposures that can lead to silicosis.
Identify two common occupational exposures that can lead to silicosis.
What condition is characterized by pleural effusions and fibrosis due to asbestos exposure?
What condition is characterized by pleural effusions and fibrosis due to asbestos exposure?
What serious health risks are associated with chronic exposure to asbestos aside from asbestosis?
What serious health risks are associated with chronic exposure to asbestos aside from asbestosis?
How do collagen fibers appear in the lung tissue of patients with usual interstitial pneumonia?
How do collagen fibers appear in the lung tissue of patients with usual interstitial pneumonia?
In which occupations is asbestos exposure primarily encountered?
In which occupations is asbestos exposure primarily encountered?
What is the pathophysiological mechanism by which silica causes damage in silicosis?
What is the pathophysiological mechanism by which silica causes damage in silicosis?
What are the major distinguishing features of complicated pneumoconiosis as compared to simple pneumoconiosis?
What are the major distinguishing features of complicated pneumoconiosis as compared to simple pneumoconiosis?
What is the incidence rate of pulmonary embolism as mentioned in the content?
What is the incidence rate of pulmonary embolism as mentioned in the content?
Explain how the lungs are oxygenated according to the content.
Explain how the lungs are oxygenated according to the content.
What is the exception to the 30% incidence of the hospitalized population dying from a specific condition?
What is the exception to the 30% incidence of the hospitalized population dying from a specific condition?
Identify the risk factors associated with compromised bronchial circulation.
Identify the risk factors associated with compromised bronchial circulation.
What complications arise from blood clots occluding large pulmonary arteries?
What complications arise from blood clots occluding large pulmonary arteries?
Explain the significance of cardiac dysregulation in pulmonary embolism risk.
Explain the significance of cardiac dysregulation in pulmonary embolism risk.
How does ischemic necrosis relate to the incidence of dying from pulmonary conditions?
How does ischemic necrosis relate to the incidence of dying from pulmonary conditions?
Discuss how large veins above the thigh contribute to the risk of pulmonary embolism.
Discuss how large veins above the thigh contribute to the risk of pulmonary embolism.
Pleural plaques are usually ______ and are detected by polarized microscopy.
Pleural plaques are usually ______ and are detected by polarized microscopy.
The risk for developing lung carcinoma is increased about ______ -fold for asbestos workers.
The risk for developing lung carcinoma is increased about ______ -fold for asbestos workers.
As the disease progresses, individual nodules coalesce into ______ scars.
As the disease progresses, individual nodules coalesce into ______ scars.
The risk for mesothelioma, normally a very rare tumor, is more than ______ times greater.
The risk for mesothelioma, normally a very rare tumor, is more than ______ times greater.
Concomitant cigarette smoking greatly increases the risk for lung carcinoma but not for ______.
Concomitant cigarette smoking greatly increases the risk for lung carcinoma but not for ______.
Silicosis is usually detected on routine chest ______, which show a fine nodularity in the upper lung zones.
Silicosis is usually detected on routine chest ______, which show a fine nodularity in the upper lung zones.
A ______ embolus lodging in the pulmonary artery bifurcation can cause death.
A ______ embolus lodging in the pulmonary artery bifurcation can cause death.
Prolonged bed rest is a risk factor for pulmonary embolism because of decreased ______ output.
Prolonged bed rest is a risk factor for pulmonary embolism because of decreased ______ output.
Asbestos causes unknown, but appears to involve some exposure that produces ______ crystals.
Asbestos causes unknown, but appears to involve some exposure that produces ______ crystals.
Once phagocytosed by macrophages, asbestos fibers activate the ______ and damage phagolysosomal membranes.
Once phagocytosed by macrophages, asbestos fibers activate the ______ and damage phagolysosomal membranes.
The oncogenic effects of asbestos may be mediated by reactive ______ generated by asbestos fibers.
The oncogenic effects of asbestos may be mediated by reactive ______ generated by asbestos fibers.
Asbestos fibers preferentially localize in the ______ lung.
Asbestos fibers preferentially localize in the ______ lung.
The clustering of asbestos-related cases suggests the involvement of ______ factors.
The clustering of asbestos-related cases suggests the involvement of ______ factors.
Carcinogens that are adsorbed onto asbestos fibers may trigger the development of ______ in the lung.
Carcinogens that are adsorbed onto asbestos fibers may trigger the development of ______ in the lung.
Asbestos-related inflammation stimulates the release of pro-inflammatory and ______ mediators.
Asbestos-related inflammation stimulates the release of pro-inflammatory and ______ mediators.
The formation of non-caseating granulomas is a characteristic feature of ______ disease.
The formation of non-caseating granulomas is a characteristic feature of ______ disease.
A ______ diagnosis does not exist, and establishing the diagnosis requires the presence of clinical and radiologic findings that are consistent with the disease.
A ______ diagnosis does not exist, and establishing the diagnosis requires the presence of clinical and radiologic findings that are consistent with the disease.
In particular, ______ must be excluded.
In particular, ______ must be excluded.
Sarcoidosis is unpredictable: It may be chronic and progressive or have periods of activity interspersed with ______.
Sarcoidosis is unpredictable: It may be chronic and progressive or have periods of activity interspersed with ______.
Overall, 65% to 70% of affected individuals recover with minimal or no ______ manifestations.
Overall, 65% to 70% of affected individuals recover with minimal or no ______ manifestations.
Hypersensitivity pneumonitis is an immunologically mediated ______ lung disease that primarily affects the alveoli and is therefore often called allergic alveolitis.
Hypersensitivity pneumonitis is an immunologically mediated ______ lung disease that primarily affects the alveoli and is therefore often called allergic alveolitis.
The ______ may become more collagenous and less cellular over time.
The ______ may become more collagenous and less cellular over time.
The ______ variant is associated with a higher risk of developing pulmonary fibrosis.
The ______ variant is associated with a higher risk of developing pulmonary fibrosis.
Chronic inflammation may lead to a decrease in the production of ______ in the lung tissue.
Chronic inflammation may lead to a decrease in the production of ______ in the lung tissue.
Pneumoconiosis is a term coined to describe lung disorders caused by inhalation of mineral ______.
Pneumoconiosis is a term coined to describe lung disorders caused by inhalation of mineral ______.
Asbestos-induced diseases involve the formation of scar tissue in the lung known as ______.
Asbestos-induced diseases involve the formation of scar tissue in the lung known as ______.
Secondary vascular changes due to superimposed pulmonary ______ can occur in pneumoconiosis.
Secondary vascular changes due to superimposed pulmonary ______ can occur in pneumoconiosis.
Common dusts contributing to pneumoconiosis include coal dust, ______, and asbestos.
Common dusts contributing to pneumoconiosis include coal dust, ______, and asbestos.
Environmental factors can influence the development of lung ______ in those exposed to mineral dusts.
Environmental factors can influence the development of lung ______ in those exposed to mineral dusts.
Pneumoconiosis is often characterized by a type of lung tissue reaction called ______ fibrosis.
Pneumoconiosis is often characterized by a type of lung tissue reaction called ______ fibrosis.
Asbestosis is a diagnosis of exclusion associated with ______ exposure.
Asbestosis is a diagnosis of exclusion associated with ______ exposure.
Pathogeneses involved in the conditions related to mineral dusts include the formation of ______.
Pathogeneses involved in the conditions related to mineral dusts include the formation of ______.
Hypersensitivity pneumonitis is usually an ______ disease.
Hypersensitivity pneumonitis is usually an ______ disease.
Hypersensitivity pneumonitis results from ______ sensitivity to certain inhaled antigens.
Hypersensitivity pneumonitis results from ______ sensitivity to certain inhaled antigens.
Hypersensitivity pneumonitis manifests predominantly as a ______ disease.
Hypersensitivity pneumonitis manifests predominantly as a ______ disease.
The response to antigens usually involves both ______ cells.
The response to antigens usually involves both ______ cells.
The response to antigens usually involves both B cells and ______ cells.
The response to antigens usually involves both B cells and ______ cells.
The responsible occupational and household ______ are diverse.
The responsible occupational and household ______ are diverse.
The associated syndromes are similar and probably have a common ______ basis.
The associated syndromes are similar and probably have a common ______ basis.
Loose, poorly formed granulomas are found in the ______ of two-thirds of affected patients.
Loose, poorly formed granulomas are found in the ______ of two-thirds of affected patients.
Match the following terms with their correct definitions as they relate to the passage.
Match the following terms with their correct definitions as they relate to the passage.
Match the following terms with their corresponding definitions based on the provided text:
Match the following terms with their corresponding definitions based on the provided text:
Match the following characteristics with the corresponding lung conditions mentioned in the text:
Match the following characteristics with the corresponding lung conditions mentioned in the text:
Match the following types of pulmonary fibrosis with their primary causes:
Match the following types of pulmonary fibrosis with their primary causes:
Match the following events in the development of pulmonary fibrosis with their corresponding roles:
Match the following events in the development of pulmonary fibrosis with their corresponding roles:
Match the following terms with their corresponding descriptions based on the provided text:
Match the following terms with their corresponding descriptions based on the provided text:
Match the following risk factors for pulmonary embolism with their corresponding mechanisms:
Match the following risk factors for pulmonary embolism with their corresponding mechanisms:
Match the following complications of pulmonary embolism with their potential consequences:
Match the following complications of pulmonary embolism with their potential consequences:
Match the following characteristics with the corresponding lung conditions mentioned in the text:
Match the following characteristics with the corresponding lung conditions mentioned in the text:
Match the following terms related to asbestos-induced lung disease with their corresponding descriptions.
Match the following terms related to asbestos-induced lung disease with their corresponding descriptions.
Match the following statements about asbestos-induced lung disease with their corresponding facts.
Match the following statements about asbestos-induced lung disease with their corresponding facts.
Match the following aspects of asbestos-induced lung disease with their corresponding features.
Match the following aspects of asbestos-induced lung disease with their corresponding features.
Match the following statements about asbestos-induced lung disease with their corresponding explanations.
Match the following statements about asbestos-induced lung disease with their corresponding explanations.
Match the following conditions with their primary associated risk factor:
Match the following conditions with their primary associated risk factor:
Match the following pulmonary diseases with their characteristic microscopic features:
Match the following pulmonary diseases with their characteristic microscopic features:
Match the following health conditions with their potential consequences:
Match the following health conditions with their potential consequences:
Match the following factors with their impact on the development of pulmonary fibrosis:
Match the following factors with their impact on the development of pulmonary fibrosis:
Match the following terms with their definitions:
Match the following terms with their definitions:
Match the following statements with their corresponding conditions:
Match the following statements with their corresponding conditions:
Match the following risk factors with the pulmonary diseases they are associated with:
Match the following risk factors with the pulmonary diseases they are associated with:
Match the following diseases with their primary pathological features:
Match the following diseases with their primary pathological features:
Match the following terms with their corresponding descriptions:
Match the following terms with their corresponding descriptions:
Match the following conditions with their primary cause:
Match the following conditions with their primary cause:
Match the following features with their corresponding disease:
Match the following features with their corresponding disease:
Match the following microscopic features with their corresponding disease:
Match the following microscopic features with their corresponding disease:
Match the following symptoms with their corresponding disease:
Match the following symptoms with their corresponding disease:
Match the following risk factors with their corresponding disease:
Match the following risk factors with their corresponding disease:
Match the following treatments with their corresponding disease:
Match the following treatments with their corresponding disease:
Match the following complications with their corresponding disease:
Match the following complications with their corresponding disease:
Flashcards are hidden until you start studying
Study Notes
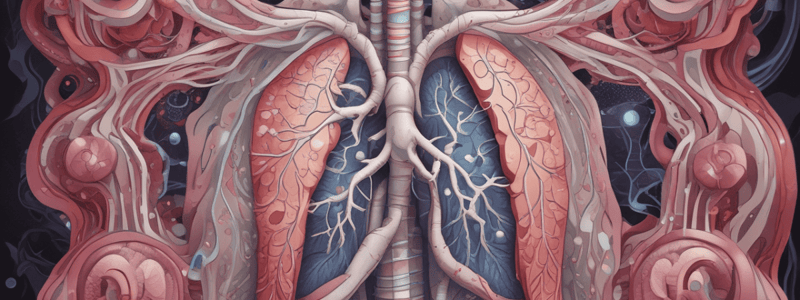
Pulmonary Fibrosis Overview
- The pleural surface of the lungs exhibits "cobblesoned" outcomes due to clinical trials leading to approved treatments.
- Survival rates post-diagnosis range from 3 to 5 years with lung transplantation for fibrotic areas.
- Microscopic analysis shows that idiopathic pulmonary fibrosis is the only definitive treatment for this condition.
Other Rare Pulmonary Diseases
- Fibrosis can vary in intensity and is associated with systemic rheumatologic diseases, such as systemic sclerosis and rheumatoid arthritis.
- Exuberant fibrosis leads to progressive scarring, negatively impacting pulmonary function over time.
Genetic Factors
- Genetics play a significant role in the development of fibrosis, particularly mutations in telomerase and surfactant proteins.
- The MUC5B variant is associated with chronic inflammation and lung injury, leading to fibrosis.
Immune Response
- Both innate and adaptive immune responses contribute to pulmonary fibrosis, with specific cytokine production facilitating inflammation.
- Granulomas replace damaged tissue, leading to scarring which can obscure lung functionality.
Clinical Features and Diagnosis
- Asymptomatic in many cases, pulmonary fibrosis may only be discovered incidentally during routine chest imaging.
- Complications include hypoxemia, resulting from multiple mechanisms such as decreased cardiac output or increased thromboembolic events.
Causes of Thromboembolism
- Risk factors for pulmonary embolism include prolonged bed rest, particularly in immobilized patients, and major branches or areas of vascular bifurcation.
- Notably, large emboli can lead to sudden death, emphasizing the need for vigilance in high-risk patients.
Antigen Sources in Hypersensitivity
- Common antigen sources leading to hypersensitivity alterations in lung function include bacteria, particularly linked to exposure in agricultural settings like dairy barns.
- Appropriate circulation and bronchiolar blood flow are crucial to prevent ischemic damage and maintain lung viability during episodes of embolism.
Reactive Minerals and Fibrotic Reactions
- Silica, asbestos, and beryllium are more reactive than coal dust.
- Genetic sequences can result in fibrotic reactions at lower concentrations.
Immune System and Inflammatory Response
- Pulmonary alveolar macrophages are central to inflammation and lung injury, influenced by surfactant mutations.
- Telomerase mutations can perpetuate inflammation, contributing to lung injury and fibrosis.
- MUC5B variant is associated with bronchiectasis caused by macrophages; particles activate the inflammasome and produce cytokines such as IL-1, initiating inflammatory responses.
- Damage to phagolysosomal membranes due to particles leads to cell injury and amplifies inflammatory reactions.
Chronic Inflammation and Fibrogenesis
- Chronic inflammation causes increased proliferation of fibroblasts and collagen deposition in the lungs.
- Tobacco smoking exacerbates harmful effects of inhaled mineral dusts, especially asbestos.
- Incidence of coal worker’s pneumoconiosis has declined due to reduced coal mining activities; however, silicosis and asbestosis remain prevalent.
Asbestos-related Pathologies
- Pleural plaques are typically asymptomatic and detected via polarized microscopy.
- Nodules can coalesce into larger lesions; the risk for lung carcinoma is increased fivefold among asbestos workers.
- Mesothelioma, a rare tumor, shows significantly higher risk—approximately 1000 times greater—in individuals with asbestos exposure.
Clinical Features and Diagnosis
- Asbestosis is usually identified on routine chest radiographs showing nodular densities, particularly in upper lung zones.
- Cardiorespiratory features may showcase the role of asbestos fibers in the pathogenesis of granulomatous diseases.
- Tobacco smoke carcinogens can adsorb onto asbestos fibers contributing to synergistic effects that heighten cancer risk in exposed individuals.
Morphological Manifestations
- Clinical features may include lymphadenopathy, cutaneous lesions, and potential eye involvement.
- Clinical findings in asymptomatic cases present with gradual onset of chronic respiratory symptoms, including fixed signs over time.
Lung and Upper Respiratory Tract Overview
- MUC5B mucin is associated with idiopathic pulmonary fibrosis, which has a germline mutation linked to particular genes.
- Idiopathic pulmonary fibrosis is more prevalent in individuals over 50 years and affects lung epithelium.
- Symptoms include a nonproductive cough, progressive dyspnea, and upon examination, "dry" or "Velcro-like" crackles are noted during inspiration.
- Cyanosis and cor pulmonale can develop in later stages of the disease.
- Antifibrotic therapies show positive outcomes in treatment.
Environmental and Occupational Exposures
- Lung responses to mineral dusts vary according to the size, shape, solubility, and reactivity of particles.
- Particles 1 to 5 μm in diameter are particularly hazardous as they can lodge in distal airways.
- Common sources of exposure include:
- Coal dust from mining leading to pneumoconiosis.
- Silica from activities like sandblasting and stone cutting causing silicosis.
- Asbestos leading to asbestosis, mesothelioma, and lung carcinoma from exposure during mining and construction work.
Asbestos and Lung Disease Risks
- Asbestos exposure increases the risk of developing lung carcinoma approximately fivefold and the risk of mesothelioma significantly.
- Asymptomatic pleural plaques can be detected through polarizing microscopy, often revealing silica deposits.
Clinical Features of Lung Diseases
- Silicosis is typically discovered via routine chest radiographs showing nodular patterns in the upper lung zones.
- Autopsy data indicate silicosis incidence may vary, reflecting environmental and occupational conditions.
- Increased lung cancer risk is associated with asbestos exposure, amplified by concomitant smoking habits.
Pathogenesis and Diagnosis
- Blood clots can obstruct pulmonary arteries, commonly occurring due to underlying pulmonary diseases or from deep vein thrombosis.
- Clinical manifestations may involve a range of symptoms depending on the extent of exposure or disease progression.
General Overview
- Pneumoconiosis refers to lung disorders caused by inhalation of mineral dust, particularly coal dust and silica.
- Characterized by hyperplastic epithelium and honeycomb fibrosis, it results in secondary vascular changes from pulmonary hypertension.
Types and Causes
- Common causes include exposure to mineral dusts and asbestos.
- Various industrial sectors contribute to dust exposure, leading to different forms of pneumoconiosis.
- Pathogenetic features often include progressive lung damage and fibrosis.
Diagnostic Features
- Diagnosis relies on clinical and radiographic findings; there’s no definitive test solely for pneumoconiosis.
- Radiography typically reveals nodularities in upper lung zones, confirmed by polarized microscopy.
- Presence of non-caseating granulomas may indicate exposure and immune response to asbestos fibers.
Risk Factors
- Increased risk of lung carcinoma for asbestos workers and a significant rise in mesothelioma incidence—over 1000 times greater in these populations.
- Cigarette smoking significantly exacerbates the risk of lung carcinoma but does not appear to affect mesothelioma risk.
Clinical Presentation
- Symptoms often arise as the disease progresses, leading to restrictive lung disease and decreased lung function.
- Asbestos-related diseases manifest through hard, collagenous scars that progress to a honeycomb lung pattern.
- Individuals may experience varying outcomes, with a significant proportion showing minimal symptoms upon recovery.
Hypersensitivity Pneumonitis
- An immunologic reaction primarily affecting alveoli and often called allergic alveolitis.
- Generally an occupational disease elicited by sensitization to specific antigens.
- Involves both B and T lymphocyte responses, leading to inflammatory processes in the lungs.
Prognosis
- The prognosis varies, with 65% to 70% of affected individuals recovering without significant residual manifestations.
- About 20% develop permanent lung dysfunction, with a small percentage progressing to pulmonary fibrosis.
- Monitoring and management are crucial for improving outcomes and managing complications associated with lung disorders.
Lung Fibrosis and Related Conditions
- Pleuron Surface: Characterized by a "cobblestroned" appearance due to treatment outcomes.
- Progression: Survival tends to be limited to 3-5 years after diagnosis involving fibrotic areas in the lung.
- Fibrosis Types: Different rare pulmonary diseases show variable fibrotic intensity. Exuberant fibroblast proliferation can be evident.
Diagnostic Considerations
- Differential Diagnosis: Rheumatologic diseases such as systemic sclerosis and rheumatoid arthritis should be considered in diagnosing pulmonary fibrosis.
- Asbestos Exposure: Supratentorial nodules may indicate fibrotic changes; the risk of lung carcinoma increases significantly, particularly in asbestos workers.
Pathophysiological Factors
- Chronic Inflammation: Leads to fibroblast proliferation and collagen deposition, exacerbating pulmonary damage.
- Pro-fibrogenic Factors: Exposure to mineral dusts, especially asbestos, is more detrimental than other particles like coal.
Risk Factors and Statistics
- Occupational Exposure: Incidence of pneumoconiosis has declined in coal miners, yet asbestos-related diseases remain prevalent.
- Pleural Plaques: Usually asymptomatic, detected via X-rays showing circumscripted densities, indicative of progressed disease.
Clinical Features and Symptoms
- Common Symptoms: May involve interstitial lung disease characterized by nodular density in upper lung zones. Skin and eye involvement can also occur.
- Asbestos Exposure: Associated with interstitial pulmonary fibrosis and increased cancer risk, namely lung and pleural cancers.
Pathogenesis of Related Diseases
- Sarcoidosis: A global incidence with higher prevalence in adults under 40.
- Occupational Hazards: Hypersensitivity pneumonitis may arise from occupational exposure; it is predominantly a restrictive lung disease caused by allergen exposure.
Importance of Work and Environmental History
- Exposure Risks: Identification of workplace and household exposure is crucial for diagnosis and prevention.
- Response to Antigens: Immune response is often mediated by both B and T cells, leading to poor cellular formation and granulation tissue.
Appendices
- Visual Guides: Provides illustrations of conditions like saddle embolus and pathological findings in affected lung areas for better understanding.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.