Podcast
Questions and Answers
What is the most critical complication that may arise from traumatic post-partum hemorrhage?
What is the most critical complication that may arise from traumatic post-partum hemorrhage?
- Failure of lactation
- Sepsis
- Acute renal failure
- Maternal death (correct)
What color is typically associated with bleeding due to traumatic post-partum hemorrhage?
What color is typically associated with bleeding due to traumatic post-partum hemorrhage?
- Pink
- Brownish red
- Dark red
- Bright red (correct)
Which of the following management strategies is NOT typically employed during the postpartum period?
Which of the following management strategies is NOT typically employed during the postpartum period?
- Bladder catheterization
- Administration of uterotonic drugs
- Uterine massage
- Delayed placental delivery (correct)
What is a common symptom indicating the need for immediate anti-shock measures?
What is a common symptom indicating the need for immediate anti-shock measures?
What is a potential treatment for retained parts of the placenta?
What is a potential treatment for retained parts of the placenta?
Which intervention is specifically recommended for a uterine atony during post-partum care?
Which intervention is specifically recommended for a uterine atony during post-partum care?
What is the definition of postpartum hemorrhage?
What is the definition of postpartum hemorrhage?
Which time frame is considered for assessing postpartum hemorrhage?
Which time frame is considered for assessing postpartum hemorrhage?
What is the minimum volume of blood loss defined as postpartum hemorrhage?
What is the minimum volume of blood loss defined as postpartum hemorrhage?
Which of the following scenarios would NOT qualify as postpartum hemorrhage?
Which of the following scenarios would NOT qualify as postpartum hemorrhage?
Why is it important to define postpartum hemorrhage clearly?
Why is it important to define postpartum hemorrhage clearly?
In gynecology and obstetrics nursing, how is postpartum hemorrhage typically quantified?
In gynecology and obstetrics nursing, how is postpartum hemorrhage typically quantified?
Which of these is a potential consequence of untreated postpartum hemorrhage?
Which of these is a potential consequence of untreated postpartum hemorrhage?
Which monitoring method is crucial in the early detection of postpartum hemorrhage?
Which monitoring method is crucial in the early detection of postpartum hemorrhage?
What is the main cause of primary hemorrhage after delivery?
What is the main cause of primary hemorrhage after delivery?
Which condition is NOT a factor affecting uterine atony?
Which condition is NOT a factor affecting uterine atony?
Secondary hemorrhage occurs after how many hours of delivery?
Secondary hemorrhage occurs after how many hours of delivery?
What is a major consequence of retained placenta after delivery?
What is a major consequence of retained placenta after delivery?
Which of the following is a potential risk factor for developing uterine atony?
Which of the following is a potential risk factor for developing uterine atony?
Which of the following is NOT related to primary hemorrhage causes?
Which of the following is NOT related to primary hemorrhage causes?
What is represented by the term 'primary hemorrhage'?
What is represented by the term 'primary hemorrhage'?
What complication can occur due to uterine over distention?
What complication can occur due to uterine over distention?
What might severe anemia contribute to post-delivery?
What might severe anemia contribute to post-delivery?
Which of the following statements is true regarding secondary hemorrhage?
Which of the following statements is true regarding secondary hemorrhage?
Flashcards
Postpartum Hemorrhage
Postpartum Hemorrhage
Bleeding more than 500 ml of blood within 24 hours after childbirth.
What is postpartum hemorrhage?
What is postpartum hemorrhage?
A serious condition that occurs when a woman loses excessive blood after childbirth.
How is postpartum hemorrhage measured?
How is postpartum hemorrhage measured?
The amount of blood lost after childbirth is measured in milliliters (ml).
What is considered a high blood loss in postpartum hemorrhage?
What is considered a high blood loss in postpartum hemorrhage?
Signup and view all the flashcards
When does postpartum hemorrhage happen?
When does postpartum hemorrhage happen?
Signup and view all the flashcards
Why is postpartum hemorrhage concerning?
Why is postpartum hemorrhage concerning?
Signup and view all the flashcards
What is important for managing postpartum hemorrhage?
What is important for managing postpartum hemorrhage?
Signup and view all the flashcards
Can postpartum hemorrhage be treated?
Can postpartum hemorrhage be treated?
Signup and view all the flashcards
Postpartum Hemorrhage (PPH)
Postpartum Hemorrhage (PPH)
Signup and view all the flashcards
Atonic PPH
Atonic PPH
Signup and view all the flashcards
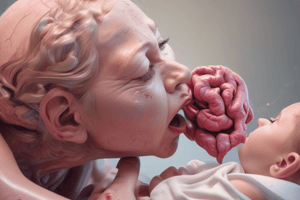
Traumatic PPH
Traumatic PPH
Signup and view all the flashcards
Shock (in PPH)
Shock (in PPH)
Signup and view all the flashcards
Endometritis
Endometritis
Signup and view all the flashcards
Subinvolution of the Uterus
Subinvolution of the Uterus
Signup and view all the flashcards
Primary Postpartum Hemorrhage
Primary Postpartum Hemorrhage
Signup and view all the flashcards
Secondary Postpartum Hemorrhage
Secondary Postpartum Hemorrhage
Signup and view all the flashcards
Uterine Atony
Uterine Atony
Signup and view all the flashcards
Antepartum Hemorrhage
Antepartum Hemorrhage
Signup and view all the flashcards
Severe Anemia
Severe Anemia
Signup and view all the flashcards
Prolonged Labor and Anesthesia
Prolonged Labor and Anesthesia
Signup and view all the flashcards
Uterine Myomas
Uterine Myomas
Signup and view all the flashcards
Retained Placenta
Retained Placenta
Signup and view all the flashcards
Coagulation Factors
Coagulation Factors
Signup and view all the flashcards
Study Notes
Postpartum Hemorrhage
- Definition: Bleeding more than 500 ml of blood within 24 hours after delivery.
- Normal Blood Loss Ranges:
- Normal labor: Less than 500 ml
- Cesarean section: Less than 1000 ml
- Effect of Excessive Blood Loss: More than 600 ml can impact a patient's overall condition.
- Types of Postpartum Hemorrhage:
- Primary: Bleeding during the third stage of labor.
- Secondary: Bleeding 24 hours or more after delivery, up to six to eight weeks postpartum.
Causes of Primary Hemorrhage
- Placental Site Bleeding:
- Uterine Atony: The most common cause (90% of cases). This refers to a uterus that is unable to contract properly after delivery.
- Factors Contributing to Uterine Atony:
- Antepartum hemorrhage
- Severe anemia
- Prolonged labor and anesthesia
- Uterine fibroids (myomas)
- Over-distended uterus
- Retained portions of the placenta
- Coagulation factor deficiencies (e.g., hypo-fibrinogenemia)
Causes of Traumatic Postpartum Hemorrhage
- Definition: Bleeding due to lacerations of the vulva, vagina, cervix, or uterus.
- Diagnosis: Assessment relies on observed blood loss and associated bodily responses, such as shock (hypotension, rapid pulse).
- Physical Examinations: (General examination)
- Assessing vital signs and color/pallor.
- (Abdominal Examination)
- Size & feel of the uterus. (atony vs trauma)
- (Vaginal examination)
- Nature & amount of bleeding
- Location of potential injuries
- (Abdominal Examination)
- Assessing vital signs and color/pallor.
Management of Postpartum Hemorrhage
- During Pregnancy:
- Detecting and treating anemia.
- Ensuring hospital delivery with crossmatched blood.
- Addressing antepartum hemorrhage.
- Labor and Postpartum:
- Using oxytocin appropriately to prevent prolonged labor.
- Avoiding unnecessary lacerations (proper anesthesia).
- Monitoring for and managing the placenta’s expulsion
- Routine examination of the placenta and membranes.
- Exploration of the birth canal (cervix) in cases of difficult deliveries.
- Careful monitoring for the first 1-2 hours post-delivery.
- Treatment:
- Immediate Anti-shock Measures: Managing blood loss.
- Depending on the cause:
- Placenta Site Bleeding:
- Immediate delivery of the placenta if in progress.
- Administering ergometrine (and other uterotonic drugs) with gentle pressure to contract the uterus.
- Brandt-Andrews maneuver, Credé's method (pressure to uterus).
- Manual removal of the retained placenta pieces.
- Traumatic Postpartum Hemorrhage: Repairing lacerations.
- Placenta Site Bleeding:
Secondary Postpartum Hemorrhage
- Causes:
- Uterus not shrinking down after birth.
- Infections, especially after C-section or other abdominal wounds.
- Retained placental fragments.
- Malignant tumors associated with trophoblastic disease (like choriocarcinoma).
- Infective conditions.
- Management:
- Treat the cause.
- Use uterotonic medications.
- Consider hysterectomy if bleeding is severe and resistant to other treatments.
- Use blood products. Avoid excess blood loss.
- Manage shock.
Clinical Presentation & Nursing Management of Postpartum Hemorrhage
- Clinical Pictures:
- Sudden estrogen withdrawal
- Bright red bleeding
- Uterus not shrinking down, or atonic uterus
- Sepsis / Infection
- Anemia
- Treatment dependent on cause:
- Retained placenta parts >> antibiotics
- Infection >> antibiotics and possibly the uterotonic medication, ergometrine
- Other causes >> treat the root cause
- Nursing Assessment:
- Vital signs and general condition
- Condition of the uterus
- Nature of bleeding (color, amount)
- Signs and symptoms of blood loss
- Amount and color of blood loss
Complications
- Maternal Death: Approximately 10% of cases.
- Acute Renal Failure
- Sepsis
- Embolism
- Anemia
- Failure of Lactation
- Sheena’s syndrome
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.