Podcast
Questions and Answers
What is one of the primary criteria for patient recovery in the PACU?
What is one of the primary criteria for patient recovery in the PACU?
- Increase in body temperature
- Complete cessation of pain
- Return to baseline cognitive function (correct)
- Initiation of IV fluid therapy
Which condition requires the nurse to use critical care skills to prevent potential complications?
Which condition requires the nurse to use critical care skills to prevent potential complications?
- Hemorrhage or respiratory distress (correct)
- Stable heart rate
- Severe headache
- Mild nausea
Which assessment is NOT typically included when assessing a patient in the PACU?
Which assessment is NOT typically included when assessing a patient in the PACU?
- Blood glucose levels (correct)
- Airway patency
- Wound condition
- Level of consciousness
What is the recommended position for a patient in the PACU unless contraindicated?
What is the recommended position for a patient in the PACU unless contraindicated?
Which of the following is a primary cardiovascular complication monitored in the PACU?
Which of the following is a primary cardiovascular complication monitored in the PACU?
What intervention is important when a patient experiences vomiting in the PACU?
What intervention is important when a patient experiences vomiting in the PACU?
Which type of medication is primarily given for pain management in the PACU?
Which type of medication is primarily given for pain management in the PACU?
Which factor is NOT considered when maintaining cardiovascular stability in the PACU?
Which factor is NOT considered when maintaining cardiovascular stability in the PACU?
What is one of the primary responsibilities of the postoperative nurse during the immediate recovery phase in the PACU?
What is one of the primary responsibilities of the postoperative nurse during the immediate recovery phase in the PACU?
Which phase of postanesthesia care is characterized by intensive nursing care?
Which phase of postanesthesia care is characterized by intensive nursing care?
Which of the following actions is NOT part of postoperative nursing care?
Which of the following actions is NOT part of postoperative nursing care?
What does Phase II PACU primarily prepare the patient for?
What does Phase II PACU primarily prepare the patient for?
Who is responsible for transferring the postoperative patient from the OR to the PACU?
Who is responsible for transferring the postoperative patient from the OR to the PACU?
Which variable is least likely to affect wound healing post-surgery?
Which variable is least likely to affect wound healing post-surgery?
During patient transport to the PACU, which consideration is critical?
During patient transport to the PACU, which consideration is critical?
What is a key goal of nursing care in the postanesthesia care unit?
What is a key goal of nursing care in the postanesthesia care unit?
What is a common risk factor for postoperative nausea and vomiting (PONV)?
What is a common risk factor for postoperative nausea and vomiting (PONV)?
What is the typical Aldrete score range indicating that a patient is ready for discharge from the PACU?
What is the typical Aldrete score range indicating that a patient is ready for discharge from the PACU?
What nursing intervention is particularly important for older adults in the postanesthesia care unit?
What nursing intervention is particularly important for older adults in the postanesthesia care unit?
How is PONV primarily controlled in patients?
How is PONV primarily controlled in patients?
Which of the following is NOT considered a surgical risk associated with PONV?
Which of the following is NOT considered a surgical risk associated with PONV?
What should be included in the discharge planning for a patient leaving the PACU?
What should be included in the discharge planning for a patient leaving the PACU?
What symptom may occur postoperatively in older adults that requires monitoring?
What symptom may occur postoperatively in older adults that requires monitoring?
Which of the following is a potential consequence of PONV?
Which of the following is a potential consequence of PONV?
What is one of the immediate nursing interventions upon receiving a postoperative patient in the clinical unit?
What is one of the immediate nursing interventions upon receiving a postoperative patient in the clinical unit?
Which nursing diagnosis is related to pain management after surgery?
Which nursing diagnosis is related to pain management after surgery?
What is a common management strategy to relieve postoperative pain?
What is a common management strategy to relieve postoperative pain?
Which symptom would indicate possible impaired airway clearance in a postoperative patient?
Which symptom would indicate possible impaired airway clearance in a postoperative patient?
What is an important assessment to perform regarding IV sites in a postoperative patient?
What is an important assessment to perform regarding IV sites in a postoperative patient?
In managing postoperative patients, why is it necessary to reinforce deep breathing and leg exercises?
In managing postoperative patients, why is it necessary to reinforce deep breathing and leg exercises?
What type of nutritional status risk is commonly associated with postoperative patients?
What type of nutritional status risk is commonly associated with postoperative patients?
Which condition can lead to impaired skin integrity in a postoperative patient?
Which condition can lead to impaired skin integrity in a postoperative patient?
What is the primary risk associated with opioid use postoperatively?
What is the primary risk associated with opioid use postoperatively?
Which of the following should be avoided in patients with head injuries during recovery?
Which of the following should be avoided in patients with head injuries during recovery?
Which type of analgesia allows the patient to control their pain relief?
Which type of analgesia allows the patient to control their pain relief?
What nursing management strategy is effective in preventing respiratory complications?
What nursing management strategy is effective in preventing respiratory complications?
What should be closely monitored for up to 24 hours post-surgery?
What should be closely monitored for up to 24 hours post-surgery?
Which exercise is recommended to prevent venous thromboembolism after surgery?
Which exercise is recommended to prevent venous thromboembolism after surgery?
What condition is characterized by an abnormal drop in blood pressure due to a change in position?
What condition is characterized by an abnormal drop in blood pressure due to a change in position?
What is a significant benefit of early ambulation postoperatively?
What is a significant benefit of early ambulation postoperatively?
What position should a patient be in to begin standing and walking after surgery?
What position should a patient be in to begin standing and walking after surgery?
Which of the following is NOT a sign of infection to assess for at the incision site?
Which of the following is NOT a sign of infection to assess for at the incision site?
What is the primary purpose of surgical drains?
What is the primary purpose of surgical drains?
What is a significant risk for patients regarding body temperature in the postoperative period?
What is a significant risk for patients regarding body temperature in the postoperative period?
Which strategy is suggested to prevent bowel distention after surgery?
Which strategy is suggested to prevent bowel distention after surgery?
What might increasing amounts of fresh blood on the surgical dressing indicate?
What might increasing amounts of fresh blood on the surgical dressing indicate?
Which method is used to detect bowel sounds postoperatively?
Which method is used to detect bowel sounds postoperatively?
Why may patients experience difficulty having a bowel movement after surgery?
Why may patients experience difficulty having a bowel movement after surgery?
Flashcards
Postoperative Period
Postoperative Period
The time from leaving the operating room until the last follow-up visit with the surgeon.
Postanesthesia Care Unit (PACU)
Postanesthesia Care Unit (PACU)
A specialized unit for patients recovering from anesthesia, offering intensive care and preparation for further care.
PACU Phases
PACU Phases
Stages of care in the PACU: Phase I (immediate recovery), Phase II (preparation for self-care).
PACU Admission
PACU Admission
Signup and view all the flashcards
Nursing Management (PACU)
Nursing Management (PACU)
Signup and view all the flashcards
Postoperative Complications
Postoperative Complications
Signup and view all the flashcards
Wound Healing
Wound Healing
Signup and view all the flashcards
Surgical Site Infections
Surgical Site Infections
Signup and view all the flashcards
PACU recovery criteria
PACU recovery criteria
Signup and view all the flashcards
PACU Nurse Responsibilities
PACU Nurse Responsibilities
Signup and view all the flashcards
Patient Airway Management
Patient Airway Management
Signup and view all the flashcards
Cardiac Monitoring in PACU
Cardiac Monitoring in PACU
Signup and view all the flashcards
PACU Pain Management
PACU Pain Management
Signup and view all the flashcards
Post-Op Patient Transfer
Post-Op Patient Transfer
Signup and view all the flashcards
Baseline Assessment in PACU
Baseline Assessment in PACU
Signup and view all the flashcards
PACU Monitoring of IV Lines
PACU Monitoring of IV Lines
Signup and view all the flashcards
Post-op Oxygen
Post-op Oxygen
Signup and view all the flashcards
Post-op Vital Sign Monitoring
Post-op Vital Sign Monitoring
Signup and view all the flashcards
Post-op Surgical Site
Post-op Surgical Site
Signup and view all the flashcards
Post-op Pain Management
Post-op Pain Management
Signup and view all the flashcards
Post-op Positioning
Post-op Positioning
Signup and view all the flashcards
Post-op Deep Breathing Exercises
Post-op Deep Breathing Exercises
Signup and view all the flashcards
Post-op Leg Exercises
Post-op Leg Exercises
Signup and view all the flashcards
Post-op Bladder Assessment
Post-op Bladder Assessment
Signup and view all the flashcards
PONV
PONV
Signup and view all the flashcards
PONV Risk Factors
PONV Risk Factors
Signup and view all the flashcards
PONV Complications
PONV Complications
Signup and view all the flashcards
Gerontologic Considerations (PACU)
Gerontologic Considerations (PACU)
Signup and view all the flashcards
Aldrete Score
Aldrete Score
Signup and view all the flashcards
PACU Discharge Readiness
PACU Discharge Readiness
Signup and view all the flashcards
Direct Discharge (Ambulatory Surgery)
Direct Discharge (Ambulatory Surgery)
Signup and view all the flashcards
Patient Education (Direct Discharge)
Patient Education (Direct Discharge)
Signup and view all the flashcards
Respiratory Complications Post-Op
Respiratory Complications Post-Op
Signup and view all the flashcards
Preventing Respiratory Complications
Preventing Respiratory Complications
Signup and view all the flashcards
Coughing Restrictions Post-Op
Coughing Restrictions Post-Op
Signup and view all the flashcards
Cardiac Output Concerns Post-Op
Cardiac Output Concerns Post-Op
Signup and view all the flashcards
Fluid Management Post-Op
Fluid Management Post-Op
Signup and view all the flashcards
Preventing Blood Clots Post-Op
Preventing Blood Clots Post-Op
Signup and view all the flashcards
Benefits of Early Ambulation
Benefits of Early Ambulation
Signup and view all the flashcards
Preventing Postural Hypotension
Preventing Postural Hypotension
Signup and view all the flashcards
Early Ambulation
Early Ambulation
Signup and view all the flashcards
Wound Care Post-Surgery
Wound Care Post-Surgery
Signup and view all the flashcards
What are signs of wound infection?
What are signs of wound infection?
Signup and view all the flashcards
What are surgical drains for?
What are surgical drains for?
Signup and view all the flashcards
Hypothermia Post-Surgery
Hypothermia Post-Surgery
Signup and view all the flashcards
Preventing Postoperative Hypothermia
Preventing Postoperative Hypothermia
Signup and view all the flashcards
Postoperative Bowel Issues
Postoperative Bowel Issues
Signup and view all the flashcards
Managing Postoperative Bowel Function
Managing Postoperative Bowel Function
Signup and view all the flashcards
Study Notes
Postoperative Nursing Management
- Postoperative care begins when the patient leaves the operating room and lasts until the final follow-up.
- Nursing care focuses on restoring physiological equilibrium, alleviating pain, preventing complications, and educating patients on self-care. Ongoing care may include telephone follow-up.
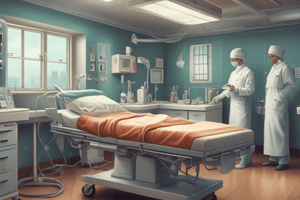
Post Anesthesia Care Unit (PACU) Care
- Patients are still under or recovering from anesthesia in the PACU.
- PACU care is divided into two phases:
- Phase I: Immediate recovery phase, providing intensive care. Patients transition to a nursing unit or Phase II PACU.
- Phase II: Preparation for self-care, transfer to an inpatient unit, extended care, or discharge.
Admitting Patients to the PACU
- The anesthesiologist or CRNA, along with other OR staff, is responsible for transferring patients.
- The anesthesia provider stays at the head of the stretcher during transport to maintain the airway, while another team member is at the opposite end.
- Crucial information, such as patient position, wounds, drains, parameters, and privacy, are considered.
- The PACU nurse reviews essential information with the anesthesiologist or CRNA.
Nursing Management in the PACU
- The goal is to monitor and provide care until patients recover.
- The criteria for recovery include: Return to baseline cognitive function, clear airway, controlled nausea/vomiting, and stabilized vital signs.
- Nurses use critical skills and training to identify early complications (e.g., hemorrhage or respiratory distress).
- Lengthy surgeries may result in direct transfer to the intensive care unit (ICU).
Assessing the Patient (PACU)
- A baseline assessment includes airway, level of consciousness, cardiac and respiratory status, wound condition, and pain.
- All drainage tubes are checked to ensure proper connection and function.
- Current IV fluids and medications are verified.
Maintaining a Patent Airway (PACU)
- Administer supplemental oxygen as prescribed.
- Monitor respiratory rate, depth, ease of breathing, oxygen saturation, and breath sounds.
- Elevate the head of the bed 15-30 degrees unless contraindicated.
- Position patients on their side if vomiting occurs to prevent aspiration.
Maintaining Cardiovascular Stability (PACU)
- Monitor the patient's level of consciousness (LOC), vital signs, cardiac rhythm, skin temperature, colour, and moisture, and urine output (UOP).
- Key cardiovascular complications monitored in the PACU include hypotension, shock, hemorrhage, hypertension, and arrhythmias.
- The nurse assesses the patency of all IV lines.
Relieving Pain and Anxiety (PACU)
- Monitor a patient's physiological status and manage pain to ease fears and concerns.
- Opioid analgesics are commonly administered intravenously.
- Non-pharmacological interventions should also be considered.
Controlling Nausea and Vomiting (PONV)
- Around 30%-50% of surgical patients experience Postoperative Nausea and Vomiting (PONV).
- It's managed with medications, both intra- and postoperatively.
- Risk Factors: female gender, age under 50, history of PONV, and opioid use.
Gerontologic Considerations (PACU)
- Older adults are more susceptible to hypothermia. Regularly adjust the patient’s position to stimulate respiration, promote circulation and maintain comfort.
- Carefully monitor for cardiopulmonary deficits.
- Be alert for and plan for postoperative confusion and delirium.
Determining Readiness for PACU Discharge
- Patients remain in the PACU until fully recovered from the anesthetic agent.
- Indicators of recovery: Stable blood pressure (BP), adequate respiratory function, and acceptable oxygen saturation(O2 sat).
- The Aldrete score is utilized to assess readiness for transfer from the PACU (scores typically between 7 and 10).
Preparing Postoperative Patients for Direct Discharge
- Ambulatory procedures often transition patients directly home from a step-down PACU
- Patient education is crucial, encompassing verbal and written instructions about postoperative changes and expected outcomes.
- The patient and caregiver should receive clear information about possible complications. Includes recovery time, prescriptions, and care instructions.
Care of the Hospitalized Postoperative Patient
- Most surgical patients requiring hospital stays have multiple needs and require frequent assessment and care interventions.
- Immediate interventions upon admission to the clinical unit include assessing breathing and administering supplemental oxygen as needed; monitoring vital signs and assessing skin color, warmth, and moisture; assessing surgical sites and wound drainage systems; connecting and monitoring closed drainage systems; assessing level of consciousness, orientation, and mobility; and evaluating pain level.
Surgical Drains
- Drains are tubes to remove fluids and prevent infection, either into a portable system or the dressings.
- Nursing care focuses on monitoring and recording drainage output frequently.
Maintaining Normal Body Temperature
- Postoperative patients are at risk for hypothermia.
- Measures to maintain a comfortable temperature include keeping the room environment warm. Blanket coverage, hydration and nutrition are also important.
Managing Gastrointestinal Function
- Decreased mobility, decreased oral intake and analgesic medications can result in difficulty with bowel movements.
- Manipulation of the abdominal organs during surgery can disrupt peristalsis (normal bowel activity) for up to 48 hours.
- Managing GI function includes monitoring bowel sounds, encouraging frequent positioning and movement (exercise), and administering stool softeners. A nasogastric tube might be used to manage vomiting and distention.
Managing Voiding
- Patients are typically expected to urinate within 8 hours of surgery.
- Encourage voiding by providing access to a bedpan or urinal and, if needed, providing fluids.
- Intermittent catheterization may be necessary if the patient cannot urinate.
Maintaining a Safe Environment
- In the immediate postoperative period, keep two-side rails up for safety.
- Position the bed at a low level.
- Assess the patient's level of consciousness and orientation.
- Maintain a call light within reach.
- Restraints may be required, following agency policy.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.