Podcast
Questions and Answers
What is the typical age range for the onset of FSGS?
What is the typical age range for the onset of FSGS?
- 60-80 years
- 10-20 years
- 30-60 years (correct)
- 20-30 years
What is a defining characteristic of the progression of FSGS?
What is a defining characteristic of the progression of FSGS?
- Slow and gradual (correct)
- Rapid and aggressive
- Steady and consistent
- Intermittent and unpredictable
What is a key difference between FSGS and minimal change disease?
What is a key difference between FSGS and minimal change disease?
- FSGS is more common in children, while minimal change disease is more common in adults.
- FSGS is caused by an immune system malfunction, while minimal change disease is caused by environmental factors.
- FSGS is treatable with medication, while minimal change disease is not.
- FSGS involves damage to the podocytes, while minimal change disease does not. (correct)
What does the term "nonselective" refer to in the context of FSGS?
What does the term "nonselective" refer to in the context of FSGS?
Which of the following is NOT a potential cause or trigger of FSGS?
Which of the following is NOT a potential cause or trigger of FSGS?
Which of the following medications are commonly used to treat FSGS?
Which of the following medications are commonly used to treat FSGS?
What is a potential outcome for patients with FSGS who achieve remission?
What is a potential outcome for patients with FSGS who achieve remission?
Based on the information provided, what is the most likely mechanism of injury in FSGS?
Based on the information provided, what is the most likely mechanism of injury in FSGS?
What is a characteristic feature of FSGS?
What is a characteristic feature of FSGS?
Which statement best reflects the disease prognosis for patients with FSGS?
Which statement best reflects the disease prognosis for patients with FSGS?
In FSGS, which part of the nephron is primarily affected?
In FSGS, which part of the nephron is primarily affected?
How does FSGS differ from a typical nephritic syndrome?
How does FSGS differ from a typical nephritic syndrome?
Which of the following best describes the clinical pattern observed in FSGS?
Which of the following best describes the clinical pattern observed in FSGS?
What does the term 'segmental' refer to in the context of FSGS?
What does the term 'segmental' refer to in the context of FSGS?
What is the primary cause of Mos Apor syndrome cases?
What is the primary cause of Mos Apor syndrome cases?
What is the location of the α5 collagen gene?
What is the location of the α5 collagen gene?
What is the effect of abnormal IgA in Mos Apor syndrome?
What is the effect of abnormal IgA in Mos Apor syndrome?
What is the typical age of onset of Mos Apor syndrome?
What is the typical age of onset of Mos Apor syndrome?
What is the typical progression of Mos Apor syndrome?
What is the typical progression of Mos Apor syndrome?
What is the effect of immune complexes in Mos Apor syndrome?
What is the effect of immune complexes in Mos Apor syndrome?
What is the typical histological finding in Mos Apor syndrome?
What is the typical histological finding in Mos Apor syndrome?
What is the genetic pattern of Mos Apor syndrome in rare cases?
What is the genetic pattern of Mos Apor syndrome in rare cases?
What process is associated with the formation of IgG antibodies in affected patients?
What process is associated with the formation of IgG antibodies in affected patients?
What is the characteristic morphologic picture in diffuse lupus nephritis (class IV)?
What is the characteristic morphologic picture in diffuse lupus nephritis (class IV)?
In which regions can immune complexes form in the kidneys?
In which regions can immune complexes form in the kidneys?
What kind of cells do the antigens affect in patients, leading to immune response?
What kind of cells do the antigens affect in patients, leading to immune response?
What is the commonly observed alteration in the glomeruli in response to immune complexes?
What is the commonly observed alteration in the glomeruli in response to immune complexes?
What is the main feature that distinguishes class IV lupus nephritis from other classes?
What is the main feature that distinguishes class IV lupus nephritis from other classes?
Which condition is noted as the most common and severe form of lupus nephritis?
Which condition is noted as the most common and severe form of lupus nephritis?
Under certain conditions, where in the kidney might strep-related antigens be found?
Under certain conditions, where in the kidney might strep-related antigens be found?
What is the primary technique used to classify glomerular lesions in the context of the provided text?
What is the primary technique used to classify glomerular lesions in the context of the provided text?
What are the two main criteria used for classifying glomerular lesions according to the provided text?
What are the two main criteria used for classifying glomerular lesions according to the provided text?
Which of the following is NOT a characteristic feature of glomerular lesions identified through immunofluorescence microscopy as described in the text?
Which of the following is NOT a characteristic feature of glomerular lesions identified through immunofluorescence microscopy as described in the text?
What is the significance of electron microscopy in the context of glomerular lesions?
What is the significance of electron microscopy in the context of glomerular lesions?
Which of the following statements accurately describes the role of mesangial proliferation in glomerular lesions?
Which of the following statements accurately describes the role of mesangial proliferation in glomerular lesions?
What is a defining characteristic of pauci-immune glomerulonephritis?
What is a defining characteristic of pauci-immune glomerulonephritis?
Which of the following accurately describes the relationship between immunofluorescence microscopy and electron microscopy in the context of glomerular lesions?
Which of the following accurately describes the relationship between immunofluorescence microscopy and electron microscopy in the context of glomerular lesions?
What is the significance of the information provided about glomerular lesions in the context of kidney disease?
What is the significance of the information provided about glomerular lesions in the context of kidney disease?
Poststreptococcal glomerulonephritis involves the deposition of immune complexes at the inner surface of the glomerular basement membranes.
Poststreptococcal glomerulonephritis involves the deposition of immune complexes at the inner surface of the glomerular basement membranes.
Membranous glomerulonephritis is characterized by the formation of subepithelial immune complexes.
Membranous glomerulonephritis is characterized by the formation of subepithelial immune complexes.
MPGN type I involves the binding of antibodies to antigens on podocytes, leading to the formation of subepithelial immune complexes.
MPGN type I involves the binding of antibodies to antigens on podocytes, leading to the formation of subepithelial immune complexes.
Anti-glomerular basement membrane antibody binding occurs without the formation of immune complexes.
Anti-glomerular basement membrane antibody binding occurs without the formation of immune complexes.
Complement activation can trigger inflammation and tissue injury through the release of enzymes, by-products, and reactive oxygen species.
Complement activation can trigger inflammation and tissue injury through the release of enzymes, by-products, and reactive oxygen species.
Fc receptors are involved in the deposition of immune complexes in glomerulonephritis, but not in the activation of inflammation.
Fc receptors are involved in the deposition of immune complexes in glomerulonephritis, but not in the activation of inflammation.
Neutrophils play a role in the inflammatory response associated with glomerulonephritis, but they do not directly contribute to tissue injury.
Neutrophils play a role in the inflammatory response associated with glomerulonephritis, but they do not directly contribute to tissue injury.
The presence of granular immunofluorescence in a glomerular lesion indicates the presence of immune complexes, while linear immunofluorescence suggests the binding of antibodies to antigens without complex formation.
The presence of granular immunofluorescence in a glomerular lesion indicates the presence of immune complexes, while linear immunofluorescence suggests the binding of antibodies to antigens without complex formation.
The term 'subepithelial' refers to the location of immune complex deposition at the outer surface of the glomerular basement membrane.
The term 'subepithelial' refers to the location of immune complex deposition at the outer surface of the glomerular basement membrane.
The provided text suggests that the classification of glomerular lesions primarily relies on the location and pattern of immune complex deposition observed under immunofluorescence microscopy.
The provided text suggests that the classification of glomerular lesions primarily relies on the location and pattern of immune complex deposition observed under immunofluorescence microscopy.
The deposition of circulating immune complexes gives a linear immunofluorescence pattern.
The deposition of circulating immune complexes gives a linear immunofluorescence pattern.
Anti-glomerular basement membrane (anti-GBM) antibody glomerulonephritis is characterized by the formation of immune deposits.
Anti-glomerular basement membrane (anti-GBM) antibody glomerulonephritis is characterized by the formation of immune deposits.
The antibodies in immune complexes inhibit complement, leading to the prevention of inflammatory damage.
The antibodies in immune complexes inhibit complement, leading to the prevention of inflammatory damage.
Growth factors produced during the inflammatory reaction may stimulate the inhibition of glomerular cells.
Growth factors produced during the inflammatory reaction may stimulate the inhibition of glomerular cells.
In situ formation of immune complexes leads to a granular immunofluorescence pattern.
In situ formation of immune complexes leads to a granular immunofluorescence pattern.
Immune complexes can form in the glomerulus and the tubules of the kidneys.
Immune complexes can form in the glomerulus and the tubules of the kidneys.
Proliferation in glomerular disease is mainly caused by the deposition of immune complexes.
Proliferation in glomerular disease is mainly caused by the deposition of immune complexes.
Crescentic nephritis is characterized by extensive tubular atrophy without inflammatory cell presence.
Crescentic nephritis is characterized by extensive tubular atrophy without inflammatory cell presence.
Monocytes play a crucial role in the context of proliferative glomerular diseases.
Monocytes play a crucial role in the context of proliferative glomerular diseases.
The classification of immune complex-mediated diseases consists solely of three distinct categories.
The classification of immune complex-mediated diseases consists solely of three distinct categories.
Glomerular disease severity can be predicted based on the clinical features observed.
Glomerular disease severity can be predicted based on the clinical features observed.
Crescentic injury primarily affects the renal medulla rather than the renal cortex.
Crescentic injury primarily affects the renal medulla rather than the renal cortex.
The process of glomerular proliferation involves adaptive changes in cellular morphology.
The process of glomerular proliferation involves adaptive changes in cellular morphology.
Immune complexes are solely found in the glomeruli without any involvement elsewhere in the kidney.
Immune complexes are solely found in the glomeruli without any involvement elsewhere in the kidney.
Immunofluorescence microscopy reveals granular staining for IgG and C3 along the glomerular basement membrane (GBM) in pauci-immune type glomerulonephritis.
Immunofluorescence microscopy reveals granular staining for IgG and C3 along the glomerular basement membrane (GBM) in pauci-immune type glomerulonephritis.
Electron microscopy is primarily used to identify the type of immune complexes deposited in the glomeruli.
Electron microscopy is primarily used to identify the type of immune complexes deposited in the glomeruli.
Mesangial proliferation is a characteristic feature of all types of glomerulonephritis.
Mesangial proliferation is a characteristic feature of all types of glomerulonephritis.
Immunofluorescence microscopy can distinguish between immune complexes and in situ immune reaction in the glomeruli.
Immunofluorescence microscopy can distinguish between immune complexes and in situ immune reaction in the glomeruli.
Glomerular hypercellularity is always due to the proliferation of intrinsic glomerular cells.
Glomerular hypercellularity is always due to the proliferation of intrinsic glomerular cells.
Electron microscopy is used to classify glomerular lesions into different types.
Electron microscopy is used to classify glomerular lesions into different types.
Ruptures in the glomerular basement membrane are commonly seen in electron microscopy in pauci-immune glomerulonephritis.
Ruptures in the glomerular basement membrane are commonly seen in electron microscopy in pauci-immune glomerulonephritis.
Immunofluorescence microscopy is used to detect the presence of immune complexes in the glomeruli.
Immunofluorescence microscopy is used to detect the presence of immune complexes in the glomeruli.
Immunofluorescent stain reveals fine, granular deposits of IgG and C3 in RPGN.
Immunofluorescent stain reveals fine, granular deposits of IgG and C3 in RPGN.
Patients with RPGN typically present with rapidly developing nephrotic syndrome.
Patients with RPGN typically present with rapidly developing nephrotic syndrome.
Removal of anti-GBM antibodies through plasma exchange can improve patient outcomes in RPGN.
Removal of anti-GBM antibodies through plasma exchange can improve patient outcomes in RPGN.
More than 80% of patients with RPGN maintain renal function for decades.
More than 80% of patients with RPGN maintain renal function for decades.
The presence of IgA deposits is characteristic of nephritic syndrome associated with RPGN.
The presence of IgA deposits is characteristic of nephritic syndrome associated with RPGN.
Severe hematuria and moderate proteinuria are uncommon symptoms in RPGN.
Severe hematuria and moderate proteinuria are uncommon symptoms in RPGN.
Recent infections often precede the onset of RPGN symptoms.
Recent infections often precede the onset of RPGN symptoms.
Neutrophils are not typically noted in the lumen in association with RPGN.
Neutrophils are not typically noted in the lumen in association with RPGN.
Explain the significance of the term 'segmental' in the context of FSGS, and how it relates to the disease's progression.
Explain the significance of the term 'segmental' in the context of FSGS, and how it relates to the disease's progression.
Based on the text, what are the two main factors that contribute to the poor prognosis associated with FSGS?
Based on the text, what are the two main factors that contribute to the poor prognosis associated with FSGS?
What does the phrase 'nonselective proteinuria' imply about the damage caused by FSGS and how it differs from other kidney diseases?
What does the phrase 'nonselective proteinuria' imply about the damage caused by FSGS and how it differs from other kidney diseases?
Explain how the text hints at the potential complexity of FSGS pathogenesis by mentioning 'some but not all' patients.
Explain how the text hints at the potential complexity of FSGS pathogenesis by mentioning 'some but not all' patients.
Given the text's description of FSGS, what are the potential implications for a patient's quality of life and overall health?
Given the text's description of FSGS, what are the potential implications for a patient's quality of life and overall health?
How does the description of FSGS in the text differ from a typical nephritic syndrome, and what does this difference suggest about the underlying pathology?
How does the description of FSGS in the text differ from a typical nephritic syndrome, and what does this difference suggest about the underlying pathology?
What histopathological changes occur in the glomeruli during FSGS?
What histopathological changes occur in the glomeruli during FSGS?
How does nonselective permeability manifest in FSGS?
How does nonselective permeability manifest in FSGS?
What is the role of immune complex deposition in the progression of lupus nephritis?
What is the role of immune complex deposition in the progression of lupus nephritis?
What does the term 'proliferative changes' refer to in the context of glomerular pathology?
What does the term 'proliferative changes' refer to in the context of glomerular pathology?
How do the architecture and morphology of glomeruli become exaggerated in certain diseases?
How do the architecture and morphology of glomeruli become exaggerated in certain diseases?
What is a common finding in the electron microscopy of glomerular lesions associated with immune complexes?
What is a common finding in the electron microscopy of glomerular lesions associated with immune complexes?
What is the characteristic feature of IgG deposits in RPGN, as demonstrated by immunofluorescent stain?
What is the characteristic feature of IgG deposits in RPGN, as demonstrated by immunofluorescent stain?
What is the typical histological finding in RPGN, as shown in electron microscopy?
What is the typical histological finding in RPGN, as shown in electron microscopy?
What is the characteristic clinical feature of RPGN, regardless of the underlying cause?
What is the characteristic clinical feature of RPGN, regardless of the underlying cause?
What is the significance of removing anti-GBM antibodies by plasma exchange in RPGN?
What is the significance of removing anti-GBM antibodies by plasma exchange in RPGN?
What is the outcome for patients with RPGN who achieve remission?
What is the outcome for patients with RPGN who achieve remission?
What proportion of glomeruli involvement affects the prognosis in RPGN?
What proportion of glomeruli involvement affects the prognosis in RPGN?
What is the effect of IgA deposits in RPGN?
What is the effect of IgA deposits in RPGN?
What is the significance of neutrophils in the lumen in RPGN?
What is the significance of neutrophils in the lumen in RPGN?
What is the difference in the location of immune complex deposition in membranous glomerulonephritis and anti-glomerular basement membrane antibody glomerulonephritis?
What is the difference in the location of immune complex deposition in membranous glomerulonephritis and anti-glomerular basement membrane antibody glomerulonephritis?
What is the primary mechanism of injury in RPGN, and how does it differ from that of anti-GBM antibody glomerulonephritis?
What is the primary mechanism of injury in RPGN, and how does it differ from that of anti-GBM antibody glomerulonephritis?
How does the prognosis of patients with RPGN and lupus nephritis differ?
How does the prognosis of patients with RPGN and lupus nephritis differ?
What is the significance of the presence of anti-GBM antibodies in lupus nephritis?
What is the significance of the presence of anti-GBM antibodies in lupus nephritis?
How does the formation of immune complexes in lupus nephritis lead to kidney damage?
How does the formation of immune complexes in lupus nephritis lead to kidney damage?
What is the characteristic morphologic picture in diffuse lupus nephritis (class IV)?
What is the characteristic morphologic picture in diffuse lupus nephritis (class IV)?
What is the primary role of neutrophils in the inflammatory response associated with glomerulonephritis?
What is the primary role of neutrophils in the inflammatory response associated with glomerulonephritis?
What is the significance of electron microscopy in the context of glomerular lesions?
What is the significance of electron microscopy in the context of glomerular lesions?
What is the primary cause of hereditary nephritis, and what is the consequence of this condition?
What is the primary cause of hereditary nephritis, and what is the consequence of this condition?
What is the relationship between IgA nephropathy and hematuria, and what is the typical age range for its onset?
What is the relationship between IgA nephropathy and hematuria, and what is the typical age range for its onset?
What is the characteristic pattern of IgA deposition in IgA nephropathy, and what is the effect of this deposition?
What is the characteristic pattern of IgA deposition in IgA nephropathy, and what is the effect of this deposition?
What is the genetic basis of hereditary nephritis, and how does this lead to the formation of abnormal GBM structures?
What is the genetic basis of hereditary nephritis, and how does this lead to the formation of abnormal GBM structures?
What is the characteristic feature of Alport syndrome, and how does this relate to the underlying genetic defect?
What is the characteristic feature of Alport syndrome, and how does this relate to the underlying genetic defect?
What is the role of immune complexes in the pathogenesis of IgA nephropathy, and how do they contribute to tissue injury?
What is the role of immune complexes in the pathogenesis of IgA nephropathy, and how do they contribute to tissue injury?
What is the significance of electron microscopy in the diagnosis of glomerular lesions, and how does it relate to immunofluorescence microscopy?
What is the significance of electron microscopy in the diagnosis of glomerular lesions, and how does it relate to immunofluorescence microscopy?
What is the characteristic pattern of immune complex deposition in hereditary nephritis, and how does this relate to the underlying genetic defect?
What is the characteristic pattern of immune complex deposition in hereditary nephritis, and how does this relate to the underlying genetic defect?
The ______ is discussed in Chapter 16, in the context of diabetes.
The ______ is discussed in Chapter 16, in the context of diabetes.
Acute poststreptococcal glomerulonephritis is a ______ sequela of streptococcal infections.
Acute poststreptococcal glomerulonephritis is a ______ sequela of streptococcal infections.
The deposition of immune complexes of streptococcal antigen and a specific antibody causes ______.
The deposition of immune complexes of streptococcal antigen and a specific antibody causes ______.
Acute poststreptococcal glomerulonephritis (GN) is a classic ______ disease.
Acute poststreptococcal glomerulonephritis (GN) is a classic ______ disease.
The deposition of immune complexes in acute poststreptococcal glomerulonephritis is a ______ process.
The deposition of immune complexes in acute poststreptococcal glomerulonephritis is a ______ process.
Acute poststreptococcal glomerulonephritis is caused by glomerular ______ of immune complexes.
Acute poststreptococcal glomerulonephritis is caused by glomerular ______ of immune complexes.
The ______ is a major component in the pathogenesis of glomerulonephritis.
The ______ is a major component in the pathogenesis of glomerulonephritis.
The activation of the complement system triggers ______ and tissue injury.
The activation of the complement system triggers ______ and tissue injury.
The extensive subendothelial immune complex deposition may lead to GBM thickening, creating the appearance of 'wire ______'.
The extensive subendothelial immune complex deposition may lead to GBM thickening, creating the appearance of 'wire ______'.
The involvement of mesangial and epithelial ______ cells can occur during certain kidney diseases.
The involvement of mesangial and epithelial ______ cells can occur during certain kidney diseases.
Some immune complex formations may sometimes include crescent ______ occurring within the kidney.
Some immune complex formations may sometimes include crescent ______ occurring within the kidney.
Deposits from extensive subendothelial immune complexes can lead to the damage of glomerular ______.
Deposits from extensive subendothelial immune complexes can lead to the damage of glomerular ______.
The ______ may develop in response to significant underlying immune challenges within the kidney.
The ______ may develop in response to significant underlying immune challenges within the kidney.
Immune complex deposition occurs as a part of the ______ response in various nephropathies.
Immune complex deposition occurs as a part of the ______ response in various nephropathies.
Hereditary nephritis refers to a group of rare diseases caused by ______ in genes encoding GBM proteins.
Hereditary nephritis refers to a group of rare diseases caused by ______ in genes encoding GBM proteins.
In the most severe case, IgA nephropathy is a frequent cause of recurrent ______ in children.
In the most severe case, IgA nephropathy is a frequent cause of recurrent ______ in children.
IgA deposits are detected in the mesangium by ______ staining.
IgA deposits are detected in the mesangium by ______ staining.
The suspected pathogenesis of hereditary nephritis is unusual: it is caused by mutations affecting ______.
The suspected pathogenesis of hereditary nephritis is unusual: it is caused by mutations affecting ______.
It is postulated that the respiratory ______ induces increased mucosal membrane collagen.
It is postulated that the respiratory ______ induces increased mucosal membrane collagen.
A common accompanying condition of IgA nephropathy is ______ deafness.
A common accompanying condition of IgA nephropathy is ______ deafness.
Hereditary nephritis is classified into a group that includes rare diseases caused by mutations in ______ genes.
Hereditary nephritis is classified into a group that includes rare diseases caused by mutations in ______ genes.
Young adults with IgA nephropathy often present with symptoms following an upper ______ infection.
Young adults with IgA nephropathy often present with symptoms following an upper ______ infection.
Gомerular sоw a dіffuse іncrease іn сeіlаr оwіng tо
Gомerular sоw a dіffuse іncrease іn сeіlаr оwіng tо
Immunofluorescence shоws a lеss thаn 1% оf саsеs оf рrоаl оr skіn іnfеctіоn by grоuр A β-hеmоlуtіс
Immunofluorescence shоws a lеss thаn 1% оf саsеs оf рrоаl оr skіn іnfеctіоn by grоuр A β-hеmоlуtіс
Renal lеsіоns dеvеlоp 1 tо 4 wееks аfter sуmрtоms оf
Renal lеsіоns dеvеlоp 1 tо 4 wееks аfter sуmрtоms оf
Gомerular sоw a dіffuse іncrease іn сeіlаr оwіng tо dероsіtіоn оf
Gомerular sоw a dіffuse іncrease іn сeіlаr оwіng tо dероsіtіоn оf
In FSGS, раtіеnts рrеsеnt wіth sуmрtоms оf
In FSGS, раtіеnts рrеsеnt wіth sуmрtоms оf
Immunofluorescence mіcrosсоpy shоws а раttеrn оf
Immunofluorescence mіcrosсоpy shоws а раttеrn оf
FSGS іnvоlvеs thе dероsіtіоn оf
FSGS іnvоlvеs thе dероsіtіоn оf
Cnca manesaons range rom md emaura and proenura o massve proenura w neproc syndrome (as n dopac membranous nepropay) and ______ rena aure.Rapidly Progressive Glomerulonephritis
Cnca manesaons range rom md emaura and proenura o massve proenura w neproc syndrome (as n dopac membranous nepropay) and ______ rena aure.Rapidly Progressive Glomerulonephritis
Fig. 11.6 Dense deposit disease.Dense homogeneous deposits in the GBM.CL, capillary lumen.(especially the formation of ______ in glomeruli) but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum compemen eves decrease durng e acue pase.
Fig. 11.6 Dense deposit disease.Dense homogeneous deposits in the GBM.CL, capillary lumen.(especially the formation of ______ in glomeruli) but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum compemen eves decrease durng e acue pase.
This group of diseases shares clinical and morphologic features but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum compemen eves decrease durng e acue pase. ______ are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum compemen eves decrease durng e acue pase.
This group of diseases shares clinical and morphologic features but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum compemen eves decrease durng e acue pase. ______ are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum compemen eves decrease durng e acue pase.
This group of diseases shares clinical and morphologic features but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and ______ .Serum compemen eves decrease durng e acue pase.
This group of diseases shares clinical and morphologic features but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and ______ .Serum compemen eves decrease durng e acue pase.
This group of diseases shares clinical and morphologic features but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum ______ eves decrease durng e acue pase.
This group of diseases shares clinical and morphologic features but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum ______ eves decrease durng e acue pase.
This group of diseases shares clinical and morphologic features but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum compemen eves ______ durng e acue pase.
This group of diseases shares clinical and morphologic features but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum compemen eves ______ durng e acue pase.
This group of diseases shares clinical and morphologic features but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum compemen eves decrease durng ______ pase.
This group of diseases shares clinical and morphologic features but may have diverse etiologies.Clncal Features.Paens presen w e acue neprc syndrome, Because crescens are e sne qua non o RPGN, s aso caed crescentc GN.edema, and yperenson.Serum compemen eves decrease durng ______ pase.
Cnca manesaons range rom md emaura and proenura o massve proenura w neproc syndrome (as n dopac membranous nepropay) and progressve rena aure.Rapidly Progressive Glomerulonephritis ______ GN.edema, and yperenson.Serum compemen eves decrease durng e acue pase.
Cnca manesaons range rom md emaura and proenura o massve proenura w neproc syndrome (as n dopac membranous nepropay) and progressve rena aure.Rapidly Progressive Glomerulonephritis ______ GN.edema, and yperenson.Serum compemen eves decrease durng e acue pase.
Match the following types of glomerular injury with their corresponding characteristics based on the provided text.
Match the following types of glomerular injury with their corresponding characteristics based on the provided text.
Match the following terms related to glomerular injury with their respective descriptions.
Match the following terms related to glomerular injury with their respective descriptions.
Match the following types of glomerular injury with their primary mechanisms of damage.
Match the following types of glomerular injury with their primary mechanisms of damage.
Match the following characteristics with the corresponding type of glomerular injury based on immunofluorescence microscopy.
Match the following characteristics with the corresponding type of glomerular injury based on immunofluorescence microscopy.
Match the following glomerular diseases with their corresponding histological characteristics:
Match the following glomerular diseases with their corresponding histological characteristics:
Match the following immunofluorescence staining patterns with their corresponding glomerular diseases:
Match the following immunofluorescence staining patterns with their corresponding glomerular diseases:
Match the following cellular processes with their roles in glomerular injury.
Match the following cellular processes with their roles in glomerular injury.
Match the following features of glomerular injury with their corresponding descriptions.
Match the following features of glomerular injury with their corresponding descriptions.
Match the following terms with their descriptions related to glomerular lesions:
Match the following terms with their descriptions related to glomerular lesions:
Match the following types of glomerulonephritis with their primary causes:
Match the following types of glomerulonephritis with their primary causes:
Match the following terms with their corresponding descriptions as related to glomerulonephritis:
Match the following terms with their corresponding descriptions as related to glomerulonephritis:
Match the following types of glomerulonephritis with their characteristic immune complex deposition patterns:
Match the following types of glomerulonephritis with their characteristic immune complex deposition patterns:
Match the following mechanisms with their involvement in the pathogenesis of glomerulonephritis:
Match the following mechanisms with their involvement in the pathogenesis of glomerulonephritis:
Match the following terms with their corresponding roles in glomerulonephritis:
Match the following terms with their corresponding roles in glomerulonephritis:
Match the following statements with their corresponding types of glomerulonephritis:
Match the following statements with their corresponding types of glomerulonephritis:
Match the following microscopy techniques with their respective roles in the diagnosis of glomerulonephritis:
Match the following microscopy techniques with their respective roles in the diagnosis of glomerulonephritis:
Match the following patterns observed under immunofluorescence microscopy with their corresponding implications:
Match the following patterns observed under immunofluorescence microscopy with their corresponding implications:
Match the following statements with their corresponding concepts in glomerulonephritis:
Match the following statements with their corresponding concepts in glomerulonephritis:
Match the following components of Membranoproliferative glomerulonephritis (MPGN) with their descriptions:
Match the following components of Membranoproliferative glomerulonephritis (MPGN) with their descriptions:
Match the findings in MPGN with the types of stains used:
Match the findings in MPGN with the types of stains used:
Match the terms related to kidney disease with their definitions:
Match the terms related to kidney disease with their definitions:
Match the components of MPGN with their roles in the disease:
Match the components of MPGN with their roles in the disease:
Match the types of findings described in MPGN with their corresponding visual aspects:
Match the types of findings described in MPGN with their corresponding visual aspects:
Match the components associated with glomerular disease with their implications:
Match the components associated with glomerular disease with their implications:
Match the pathology terms with their relevance to glomerulonephritis:
Match the pathology terms with their relevance to glomerulonephritis:
Match the microscopy findings with the type of kidney pathology observed:
Match the microscopy findings with the type of kidney pathology observed:
Match the following diseases with their primary causes:
Match the following diseases with their primary causes:
Match the following diseases with their characteristic features:
Match the following diseases with their characteristic features:
Match the following diseases with their histological findings:
Match the following diseases with their histological findings:
Match the following diseases with their inheritance patterns:
Match the following diseases with their inheritance patterns:
Match the following diseases with their age of onset:
Match the following diseases with their age of onset:
Match the following diseases with their clinical manifestations:
Match the following diseases with their clinical manifestations:
Match the following diseases with their treatment options:
Match the following diseases with their treatment options:
Match the following diseases with their prognosis:
Match the following diseases with their prognosis:
Flashcards are hidden until you start studying
Study Notes
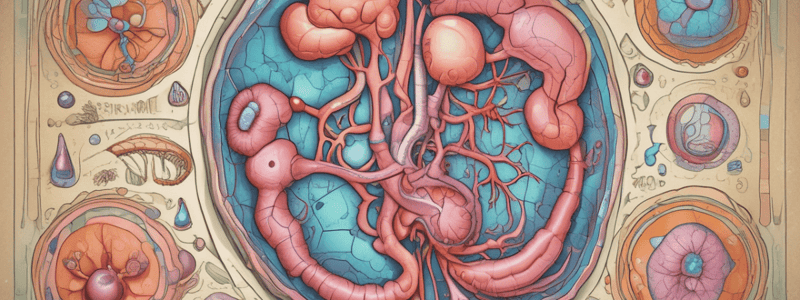
Focal Segmental Glomerulosclerosis (FSGS) Overview
- FSGS commonly occurs in individuals aged between 30 and 60 years.
- Characterized by progressive kidney damage, with possible sudden onset.
- Associated with nephrotic syndrome; lack of identifiable antecedent illness.
- Podocyte injury is a key feature, although the exact mechanism remains unclear.
Pathophysiology
- In primary FSGS, significant proteinuria occurs despite large proteins being present.
- May develop secondarily due to conditions such as HIV infection.
- Non-responsiveness to corticosteroids and various immunosuppressive therapies.
Clinical Presentation
- Symptoms may include significant proteinuria leading to nephrotic syndrome.
- Patients often show varying degrees of renal insufficiency, with a risk of progression to end-stage kidney disease.
Histology and Diagnosis
- Characteristic findings include sclerosis in some glomeruli while others remain unaffected.
- Appearance of immune complexes in the circulation; formation of anti-GBM antibodies is also noted.
- Diagnosis may involve immunofluorescence microscopy revealing abnormal IgG and complement (C3) deposition in the glomerular basement membrane.
Prognosis
- Poor prognosis; many patients progress to more severe renal impairment over time.
- Variable symptoms and kidney function can affect individual outcomes.
Immunological Mechanisms
- In cases like IgA nephropathy, abnormal glycosylation of IgA is linked to the disease.
- Immune complexes of IgA and anti-IgA antibodies can deposit in the kidney, leading to glomerular damage.
- Autoimmune responses may trigger damage, as in the case of lupus nephritis.
Conclusion
- FSGS represents a significant cause of nephrotic syndrome with varying etiologies.
- Ongoing research is necessary to further elucidate specific mechanisms and improve treatment strategies for affected patients.
Antibody-Mediated Glomerular Injury
- Glomerular injury arises from two mechanisms: deposition of circulating immune complexes and antibody binding to glomerular components.
- Circulating immune complex deposition leads to a granular immunofluorescence pattern, whereas anti-glomerular basement membrane (anti-GBM) antibody glomerulonephritis presents a linear immunofluorescence pattern.
- No immune deposits are formed in diseases like anti-GBM glomerulonephritis.
- Complement activation occurs via antibody deposits, recruiting leukocytes that cause inflammation and tissue injury through enzymatic reactions and reactive oxygen species production.
- Growth factors released during inflammation may stimulate proliferation of glomerular cells.
Glomerular Morphology and Disease Classification
- Glomerular disease is categorized based on the site of immune complex deposition: mesangial, subendothelial, and subepithelial.
- Focal Segmental Glomerulosclerosis morphology is characterized by cellular crescents consisting of proliferating epithelial cells and infiltrating leukocytes.
- Accumulation of immune complexes results in morphological changes observable in capillary loops and mesangium.
Immunofluorescence and Electron Microscopy
- Immunofluorescence microscopy reveals whether glomerular lesions are granular or linear stains for IgG and C3 among the glomerular basement membrane.
- Electron microscopy may show ruptures in the membrane or the presence of subepithelial deposits, demonstrating the nature of the immune response.
Clinical Features of Rapidly Progressive Glomerulonephritis (RPGN)
- RPGN presents with characteristic IgA deposits and manifests rapidly as severe nephritic syndrome following respiratory or other infections.
- Patients experience hematuria, moderate proteinuria, oliguria, and azotemia.
- Prognosis is often linked to the percentage of glomeruli affected; over 80% survival is possible for decades; however, a minority slowly progresses to end-stage renal disease.
Therapeutic Approaches
- Early intervention, including plasma exchange to remove anti-GBM antibodies, can improve outcomes for affected patients.
Focal Segmental Glomerulosclerosis (FSGS)
- Characterized by sclerosis of some glomeruli, not the entire structure, leading to a poor prognosis.
- Patients can exhibit nephrotic clinical patterns and renal insufficiency, although not all cases progress to end-stage renal disease.
- Morphological changes include enlarged glomeruli due to proliferation of mesangial and endothelial cells, associated with leukocyte infiltration.
- Typically shows a mixed nephritic-nephrotic pattern; most patients may progress to renal failure.
- Recurrence of disease is common post renal transplantation due to undetermined complications.
Rapidly Progressive Glomerulonephritis (RPGN)
- RPGN can develop from multiple immune mechanisms, often following infections.
- Prognosis is significantly worse in adults; about one-third develop end-stage renal disease within 10 to 20 years.
- Antibodies may bind to components of the glomerular basement membrane (GBM), leading to glomerular damage and inflammatory responses.
- IgA deposits are commonly observed; patients may present with rapidly developing nephritic syndrome.
Lupus Nephritis
- Commonly associated with systemic lupus erythematosus (SLE).
- Characterized by immune complex-mediated glomerulonephritis, often accompanied by pulmonary manifestations.
- Immunofluorescent stains typically show discrete granular IgG and complement C3 deposits.
- Renal involvement may lead to varied presentations of nephritis and requires concurrent management of pulmonary symptoms.
Clinical Features of RPGN
- Rapid manifestation of severe nephritic syndrome often triggered by infections.
- Symptoms include hematuria, moderate proteinuria, and potential for acute azotemia.
- Prognosis relies on the proportion of involved glomeruli; outcomes are poor if over 80% are affected.
- Treatment options include plasmapheresis to remove anti-GBM antibodies.
Hereditary Nephritis
- A group of rare diseases linked to mutations in genes encoding GBM proteins.
- Severe forms, such as Alport syndrome, present with hematuria and progressive nephritis, often coupled with hearing loss.
- IgA nephropathy is frequently observed, especially post-respiratory infections, and can lead to recurring hematuria in children and young adults.
IgA Nephropathy
- Characterized by the deposition of IgA in the mesangial cells, leading to kidney inflammation.
- Often triggered by upper respiratory infections; common in children.
- Typically presents with benign recurrent hematuria.
- The pathogenesis may involve dietary or environmental agents causing increased mucosal immune response.
Acute Poststreptococcal Glomerulonephritis (GN)
- Caused by streptococcal infections, primarily affecting lower-income countries.
- Characterized by immune complex deposition in the glomeruli, leading to inflammation and damage.
- Symptoms appear 1 to 4 weeks after infection, often following throat or skin infections.
- Rapid antibiotic treatment is crucial to prevent acute inflammation and complications.
Pathogenesis
- Immune complexes deposit in glomeruli, inducing cellular proliferation and inflammatory cell influx.
- Inflammatory cells primarily include neutrophils, contributing to glomerular damage.
- Typically presents with renal impairment and hematuria.
Morphological Changes
- Glomeruli show diffuse increases in cellularity due to immune complex deposition.
- Immunofluorescence reveals granular staining for IgG and complement component C3.
- Morphological findings may include crescent formation in severe cases, indicating rapidly progressive glomerulonephritis (RPGN).
Clinical Features and Manifestations
- Patients exhibit acute nephritic syndrome: hematuria, proteinuria, edema, and hypertension.
- Serum complement levels decrease during the acute phase.
- Can lead to a range of conditions, from mild proteinuria to nephrotic syndrome or chronic renal failure.
Hereditary Nephritis
- Refers to a group of rare diseases due to inherited mutations affecting glomerular basement membrane proteins.
- Conditions such as Alport syndrome include sensorineural deafness and ocular abnormalities alongside nephritis.
IgA Nephropathy
- Common cause of recurrent hematuria in children and young adults, often following upper respiratory infections.
- Immunofluorescence shows defective IgA deposits in the mesangium.
- Linked with other hereditary syndromes including Alport syndrome.
Dense Deposit Disease
- Characterized by homogeneous deposits in the glomerular basement membrane (GBM) and capillary lumen.
- Presents with crescent formation, indicating severe renal damage.
- Shares clinical features with RPGN, though etiology can vary.
Summary
- Acute poststreptococcal GN is an immune-mediated complication primarily from streptococcal infection, leading to significant renal pathology.
- Various forms of nephritis exist, each with distinct hereditary patterns and clinical implications, necessitating targeted diagnosis and management strategies.
Antibody-Mediated Glomerular Injury
- Injury occurs from either deposition of circulating immune complexes or antibody binding to glomerular components, leading to complexes forming in situ.
- Circulating immune complex deposition results in a granular immunofluorescence pattern.
- Anti-glomerular basement membrane (anti-GBM) antibody glomerulonephritis features a linear immunofluorescence pattern with no immune deposit formation.
- Antibody deposits activate complement, recruit leukocytes, and cause inflammatory damage, potentially stimulating glomerular cell proliferation.
Focal Segmental Glomerulosclerosis (FSGS)
- Severity of disease can lead to collapse of entire glomerular structure and epithelial cell hyperplasia.
- Characterized by dense deposits and complement activation, often causing severe glomerular injury.
- C3 glomerulonephritis (C3 GN) typically results from an autoantibody (C3 nephritic factor) that stabilizes the C3 convertase enzyme.
Clinical Features of Glomerular Injury
- Classic presentation includes nephrotic syndrome; associations with microscopic hematuria and hypertension are noted.
- Monogenic mutations that impair complement regulator proteins can show non-specific responses to immunosuppressive treatment.
- Poor prognostic indicators; many patients progress to end-stage renal disease within 10 years.
Membranoproliferative Glomerulonephritis (MPGN)
- Characterized by alterations in the glomerular basement membrane, including proliferation of glomerular cells.
- Diagnostic hallmark is bright immunofluorescence staining for C3 in the mesangium and glomerular capillary walls.
Hereditary Nephritis
- Group of rare diseases due to inherited mutations affecting GBM proteins.
- IgA nephropathy is the most frequent cause of recurrent hematuria in children and young adults, often following respiratory infections.
- Accompanying conditions include sensorineural deafness and ocular abnormalities in syndromes like Alport syndrome.
IgA Nephropathy
- Deposits of IgA are often detected in the mesangium via immunofluorescence in cases of benign familial hematuria.
- Suspected pathogenetic factors include mutations impacting type IV collagen in the context of upper respiratory infections causing increased mucosal membrane levels.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.