Podcast
Questions and Answers
What occurs during a tension pneumothorax?
What occurs during a tension pneumothorax?
- Blood accumulates in the pleural space.
- Lung elasticity is unaffected.
- Air can exit the pleural space during expiration.
- Air enters the pleural space and cannot exit, increasing pressure. (correct)
Which condition is characterized by multiple rib fractures leading to paradoxical chest wall movement?
Which condition is characterized by multiple rib fractures leading to paradoxical chest wall movement?
- Pneumothorax
- Tension pneumothorax
- Flail chest (correct)
- Hemothorax
What is the main consequence of a mediastinal shift caused by a tension pneumothorax?
What is the main consequence of a mediastinal shift caused by a tension pneumothorax?
- Reduced pressure in the pleural space
- Decreased venous return (correct)
- Enhanced cardiac output
- Increased lung expansion
Which of the following is a risk factor for developing a pneumothorax?
Which of the following is a risk factor for developing a pneumothorax?
What typically triggers a spontaneous pneumothorax?
What typically triggers a spontaneous pneumothorax?
What is a common physical assessment finding in a patient experiencing respiratory distress?
What is a common physical assessment finding in a patient experiencing respiratory distress?
In a patient with a tension pneumothorax, what would you expect to find upon percussion of the chest?
In a patient with a tension pneumothorax, what would you expect to find upon percussion of the chest?
Which laboratory finding is indicative of hypoxemia in a patient?
Which laboratory finding is indicative of hypoxemia in a patient?
What is a significant assessment finding that suggests the presence of subcutaneous emphysema?
What is a significant assessment finding that suggests the presence of subcutaneous emphysema?
Which of the following is not a manifestation of respiratory distress?
Which of the following is not a manifestation of respiratory distress?
What is the primary purpose of performing a chest x-ray in cases of suspected pneumothorax or hemothorax?
What is the primary purpose of performing a chest x-ray in cases of suspected pneumothorax or hemothorax?
Which nursing action is NOT a responsibility during a thoracentesis procedure?
Which nursing action is NOT a responsibility during a thoracentesis procedure?
What should a patient be instructed to do during the thoracentesis procedure?
What should a patient be instructed to do during the thoracentesis procedure?
What sensation might a patient experience when the needle is inserted into the pleural space during thoracentesis?
What sensation might a patient experience when the needle is inserted into the pleural space during thoracentesis?
What is the role of the nurse in assisting with the client's positioning for thoracentesis?
What is the role of the nurse in assisting with the client's positioning for thoracentesis?
What is a recommended nursing action to enhance a patient's ventilation?
What is a recommended nursing action to enhance a patient's ventilation?
Which of the following assessments should be performed every 4 hours?
Which of the following assessments should be performed every 4 hours?
What is the primary purpose of administering emotional support to a client?
What is the primary purpose of administering emotional support to a client?
What should be done if there is evidence of infection in a patient?
What should be done if there is evidence of infection in a patient?
Which intervention is appropriate for a patient receiving mechanical ventilation?
Which intervention is appropriate for a patient receiving mechanical ventilation?
What are the primary receptors activated by opioid agonists like morphine sulfate and fentanyl?
What are the primary receptors activated by opioid agonists like morphine sulfate and fentanyl?
Which assessment indicates a need to stop opioid medication immediately?
Which assessment indicates a need to stop opioid medication immediately?
What is the recommended action for a client receiving a fentanyl patch?
What is the recommended action for a client receiving a fentanyl patch?
What is a significant nursing action to monitor when a client is on opioid medications?
What is a significant nursing action to monitor when a client is on opioid medications?
Which statement regarding patient-controlled analgesia (PCA) is true for the client?
Which statement regarding patient-controlled analgesia (PCA) is true for the client?
Which nursing action is essential when monitoring a client receiving benzodiazepines?
Which nursing action is essential when monitoring a client receiving benzodiazepines?
What should be included in client education regarding the effects of benzodiazepines?
What should be included in client education regarding the effects of benzodiazepines?
Which interprofessional service is appropriate for a client requiring airway management following sedative administration?
Which interprofessional service is appropriate for a client requiring airway management following sedative administration?
What is the primary purpose of inserting a chest tube?
What is the primary purpose of inserting a chest tube?
What is a nursing responsibility during chest tube management?
What is a nursing responsibility during chest tube management?
What is an essential practice to prevent infection for clients recovering from respiratory conditions?
What is an essential practice to prevent infection for clients recovering from respiratory conditions?
Which action should be recommended to aid lung expansion in a client?
Which action should be recommended to aid lung expansion in a client?
What type of immunizations should clients obtain to prevent respiratory complications?
What type of immunizations should clients obtain to prevent respiratory complications?
What should clients report to their healthcare provider during recovery from pneumothorax or hemothorax?
What should clients report to their healthcare provider during recovery from pneumothorax or hemothorax?
What aspect of recovery involves psychological support for patients?
What aspect of recovery involves psychological support for patients?
Which nursing action is essential during chest tube management?
Which nursing action is essential during chest tube management?
What client education should be provided to promote lung expansion during recovery?
What client education should be provided to promote lung expansion during recovery?
Which of the following symptoms should a client report to their provider during recovery?
Which of the following symptoms should a client report to their provider during recovery?
Which of the following is NOT a recommended nursing action after chest tube insertion?
Which of the following is NOT a recommended nursing action after chest tube insertion?
What is a primary nursing action when a patient experiences decreased cardiac output due to increased intrathoracic pressure?
What is a primary nursing action when a patient experiences decreased cardiac output due to increased intrathoracic pressure?
Which nursing action is appropriate to take in response to respiratory failure caused by lung collapse?
Which nursing action is appropriate to take in response to respiratory failure caused by lung collapse?
What vital sign should be closely monitored to assess the effects of decreased cardiac output?
What vital sign should be closely monitored to assess the effects of decreased cardiac output?
When monitoring intake and output for a patient with respiratory complications, which specific output is significant?
When monitoring intake and output for a patient with respiratory complications, which specific output is significant?
What is an expected consequence of inadequate gas exchange due to lung collapse?
What is an expected consequence of inadequate gas exchange due to lung collapse?
What is an expected finding in a patient with flail chest?
What is an expected finding in a patient with flail chest?
Which nursing intervention is essential for promoting lung expansion in a patient with flail chest?
Which nursing intervention is essential for promoting lung expansion in a patient with flail chest?
What is a common physiological response observed in a patient with flail chest?
What is a common physiological response observed in a patient with flail chest?
Which of the following findings indicates paradoxical movement of the chest wall?
Which of the following findings indicates paradoxical movement of the chest wall?
In the management of a patient with flail chest, which action is important when administering pain medication?
In the management of a patient with flail chest, which action is important when administering pain medication?
Flashcards
Pneumothorax
Pneumothorax
Air or gas in the pleural space, causing lung collapse.
Tension Pneumothorax
Tension Pneumothorax
Air trapped in the pleural space, preventing its escape, putting pressure on heart and lungs.
Hemothorax
Hemothorax
Blood in the pleural space.
Spontaneous Pneumothorax
Spontaneous Pneumothorax
Signup and view all the flashcards
Flail Chest
Flail Chest
Signup and view all the flashcards
Pleuritic pain
Pleuritic pain
Signup and view all the flashcards
Respiratory distress
Respiratory distress
Signup and view all the flashcards
Tracheal deviation
Tracheal deviation
Signup and view all the flashcards
Reduced breath sounds
Reduced breath sounds
Signup and view all the flashcards
Hypoxemia
Hypoxemia
Signup and view all the flashcards
Chest X-ray
Chest X-ray
Signup and view all the flashcards
Thoracentesis
Thoracentesis
Signup and view all the flashcards
Thoracentesis purpose
Thoracentesis purpose
Signup and view all the flashcards
Thoracentesis Nursing Actions
Thoracentesis Nursing Actions
Signup and view all the flashcards
Thoracentesis Client Education
Thoracentesis Client Education
Signup and view all the flashcards
High-Fowler's Position
High-Fowler's Position
Signup and view all the flashcards
Oxygen Therapy
Oxygen Therapy
Signup and view all the flashcards
Vital Signs
Vital Signs
Signup and view all the flashcards
Mechanical Ventilation
Mechanical Ventilation
Signup and view all the flashcards
Emotional Support
Emotional Support
Signup and view all the flashcards
Opioid Agonists
Opioid Agonists
Signup and view all the flashcards
Morphine Sulfate and Fentanyl
Morphine Sulfate and Fentanyl
Signup and view all the flashcards
Respiratory Depression
Respiratory Depression
Signup and view all the flashcards
PCA Pump
PCA Pump
Signup and view all the flashcards
Fluid Intake for Opioid Users
Fluid Intake for Opioid Users
Signup and view all the flashcards
Benzodiazepine Use for Anxiety
Benzodiazepine Use for Anxiety
Signup and view all the flashcards
Monitoring Benzodiazepine Effects
Monitoring Benzodiazepine Effects
Signup and view all the flashcards
Chest Tube: Function
Chest Tube: Function
Signup and view all the flashcards
Chest Tube Nursing Actions
Chest Tube Nursing Actions
Signup and view all the flashcards
Rehabilitation Consultation
Rehabilitation Consultation
Signup and view all the flashcards
Deep breathing exercises
Deep breathing exercises
Signup and view all the flashcards
Rest periods
Rest periods
Signup and view all the flashcards
Hand hygiene
Hand hygiene
Signup and view all the flashcards
Incentive spirometry
Incentive spirometry
Signup and view all the flashcards
Follow-up care
Follow-up care
Signup and view all the flashcards
Chest Tube Insertion: Why?
Chest Tube Insertion: Why?
Signup and view all the flashcards
Recovery from a Pneumothorax
Recovery from a Pneumothorax
Signup and view all the flashcards
Upper Respiratory Infection: Warning Signs
Upper Respiratory Infection: Warning Signs
Signup and view all the flashcards
Decreased Cardiac Output
Decreased Cardiac Output
Signup and view all the flashcards
Hypotension
Hypotension
Signup and view all the flashcards
Respiratory Failure
Respiratory Failure
Signup and view all the flashcards
IV Fluid Adminstration
IV Fluid Adminstration
Signup and view all the flashcards
Monitor Heart Rate and Rhythm
Monitor Heart Rate and Rhythm
Signup and view all the flashcards
What is flail chest?
What is flail chest?
Signup and view all the flashcards
What are the main signs of flail chest?
What are the main signs of flail chest?
Signup and view all the flashcards
How is oxygenation compromised in flail chest?
How is oxygenation compromised in flail chest?
Signup and view all the flashcards
What is the primary nursing intervention for flail chest?
What is the primary nursing intervention for flail chest?
Signup and view all the flashcards
Why are pain medications important for flail chest patients?
Why are pain medications important for flail chest patients?
Signup and view all the flashcards
Study Notes
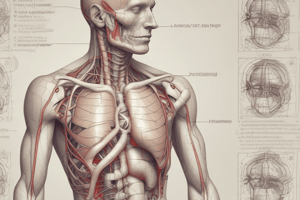
Pneumothorax
- Pneumothorax: Presence of air/gas in pleural space, causing lung collapse.
- Tension pneumothorax: Air enters pleural space during inspiration (one-way valve), cannot exit on expiration. Trapped air puts pressure on heart and lung. This increases pressure, compresses blood vessels, limits venous return, decreases cardiac output, and can lead to death if not treated immediately. Increased pressure and air in pleural cavity causes mediastinal shift.
Hemothorax
- Hemothorax: Accumulation of blood in pleural space.
Spontaneous Pneumothorax
- Spontaneous pneumothorax: Occurs without trauma. A small bleb on the lung ruptures, releasing air into pleural space.
Flail Chest
- Flail chest: At least two adjacent ribs (usually one side) sustain multiple fractures, causing chest wall instability and paradoxical chest wall movement. This significantly limits chest wall expansion.
Assessment and Risk Factors
- Risk factors: Blunt chest trauma, penetrating chest wounds, closed/occluded chest tube.
- Older adults: Reduced pulmonary reserves, decreased lung elasticity, and thickened alveoli.
- Chronic obstructive pulmonary disease (COPD): Increased risk.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.