Podcast
Questions and Answers
What condition is characterized by dilated centrilobular sinusoids and pressure atrophy of hepatocytes?
What condition is characterized by dilated centrilobular sinusoids and pressure atrophy of hepatocytes?
- Acute Hepatitis
- Fatty Liver Disease
- Hepatic Cirrhosis
- Chronic Passive Congestion (correct)
Which clinical feature is associated with pulmonary venous congestion?
Which clinical feature is associated with pulmonary venous congestion?
- Peripheral Edema
- Jugular Venous Distension
- Ascites
- Dyspnea (correct)
What is the appearance of a liver affected by right heart failure?
What is the appearance of a liver affected by right heart failure?
- Uniformly enlarged and smooth
- Bright red with hemorrhagic spots
- Pale and fibrotic
- Nutmeg pattern with centrilobular necrosis (correct)
What clinical features are typically observed in patients with deep vein thrombosis (DVT)?
What clinical features are typically observed in patients with deep vein thrombosis (DVT)?
Which organs are typically associated with white infarcts?
Which organs are typically associated with white infarcts?
What type of venous congestion is associated with constrictive pericarditis?
What type of venous congestion is associated with constrictive pericarditis?
What distinguishes red infarcts from white infarcts?
What distinguishes red infarcts from white infarcts?
Which of the following is NOT a common clinical feature of hepatic congestion?
Which of the following is NOT a common clinical feature of hepatic congestion?
What primarily influences the capillary oncotic pressure (πc) that pulls fluid back into the capillary?
What primarily influences the capillary oncotic pressure (πc) that pulls fluid back into the capillary?
What condition can lead to increased hydrostatic pressure causing edema in the body?
What condition can lead to increased hydrostatic pressure causing edema in the body?
Which endocrine disorder is associated with increased sodium retention that may contribute to edema?
Which endocrine disorder is associated with increased sodium retention that may contribute to edema?
What is a potential consequence of decreased oncotic pressure in the blood?
What is a potential consequence of decreased oncotic pressure in the blood?
What role does the lymphatic system play in preventing edema?
What role does the lymphatic system play in preventing edema?
Which of the following is NOT a cause of edema related to decreased venous drainage?
Which of the following is NOT a cause of edema related to decreased venous drainage?
Which condition is characterized by excessive leakage of protein from the glomerulus, contributing to decreased oncotic pressure?
Which condition is characterized by excessive leakage of protein from the glomerulus, contributing to decreased oncotic pressure?
What can excessive leukocyte activity at the endothelial level generally lead to?
What can excessive leukocyte activity at the endothelial level generally lead to?
What is the primary reason that shock can be fatal?
What is the primary reason that shock can be fatal?
Which of the following correctly describes the vasodilation effect in septic shock?
Which of the following correctly describes the vasodilation effect in septic shock?
During which stage of shock is the body still able to maintain normal blood pressure but exhibits tachycardia?
During which stage of shock is the body still able to maintain normal blood pressure but exhibits tachycardia?
What happens during Stage II – decompensated shock?
What happens during Stage II – decompensated shock?
What critical physiological change occurs as a consequence of high pro-inflammatory cytokine levels?
What critical physiological change occurs as a consequence of high pro-inflammatory cytokine levels?
What characterizes Stage III – irreversible shock?
What characterizes Stage III – irreversible shock?
What is anasarca?
What is anasarca?
Which of the following best describes the movement of leukocytes in septic shock?
Which of the following best describes the movement of leukocytes in septic shock?
What is a significant risk associated with the failure of compensatory mechanisms in septic shock?
What is a significant risk associated with the failure of compensatory mechanisms in septic shock?
What distinguishes hyperemia from congestion?
What distinguishes hyperemia from congestion?
Which condition is associated with hemosiderin deposition?
Which condition is associated with hemosiderin deposition?
What is the primary cause of pulmonary edema?
What is the primary cause of pulmonary edema?
What can chronic passive congestion in the lungs lead to?
What can chronic passive congestion in the lungs lead to?
What would NOT be a clinical feature of edema?
What would NOT be a clinical feature of edema?
What color do congested tissues typically appear due to blood stasis?
What color do congested tissues typically appear due to blood stasis?
Which of the following best describes the consequence of long-term pulmonary congestion?
Which of the following best describes the consequence of long-term pulmonary congestion?
What type of edema results specifically from heart failure?
What type of edema results specifically from heart failure?
In the case of hepatic congestion, which feature is typically observed?
In the case of hepatic congestion, which feature is typically observed?
What is the most common cause of ischemic heart disease?
What is the most common cause of ischemic heart disease?
Which of the following symptoms is indicative of hypovolemic or cardiogenic shock?
Which of the following symptoms is indicative of hypovolemic or cardiogenic shock?
What pathological process leads to ischemic heart disease through sudden occlusion?
What pathological process leads to ischemic heart disease through sudden occlusion?
Which of the following factors does NOT acutely influence the heart's metabolic demands?
Which of the following factors does NOT acutely influence the heart's metabolic demands?
Which condition describes the inadequate blood supply to the myocardium for its metabolic needs?
Which condition describes the inadequate blood supply to the myocardium for its metabolic needs?
What physiological change occurs due to the progressive narrowing of coronary arteries?
What physiological change occurs due to the progressive narrowing of coronary arteries?
Which of the following best describes the appearance of skin during septic shock?
Which of the following best describes the appearance of skin during septic shock?
What does Laplace’s law indicate about wall tension in the heart?
What does Laplace’s law indicate about wall tension in the heart?
What characterizes stable angina compared to unstable angina?
What characterizes stable angina compared to unstable angina?
What is a key distinction in the treatment approaches for stable angina compared to unstable angina?
What is a key distinction in the treatment approaches for stable angina compared to unstable angina?
Which treatment is most effective for Prinzmetal angina?
Which treatment is most effective for Prinzmetal angina?
In which scenario would resting blood flow to the myocardium be significantly affected?
In which scenario would resting blood flow to the myocardium be significantly affected?
Which treatment is considered beneficial specifically for myocardial infarction patients with STEMI?
Which treatment is considered beneficial specifically for myocardial infarction patients with STEMI?
What is a common feature associated with acute coronary syndromes?
What is a common feature associated with acute coronary syndromes?
What is the primary purpose of using ASA (acetylsalicylic acid) in the management of ischemic heart disease?
What is the primary purpose of using ASA (acetylsalicylic acid) in the management of ischemic heart disease?
Which of the following statements about the management of heart disease is MOST accurate?
Which of the following statements about the management of heart disease is MOST accurate?
Which condition primarily leads to ischemic heart disease in most cases?
Which condition primarily leads to ischemic heart disease in most cases?
What is the main concern that leads to high mortality soon after a myocardial infarction?
What is the main concern that leads to high mortality soon after a myocardial infarction?
Which physiological change can indicate the development of ischemic cardiomyopathy?
Which physiological change can indicate the development of ischemic cardiomyopathy?
What can exacerbate oxygen delivery during episodes of ischemia in heart disease?
What can exacerbate oxygen delivery during episodes of ischemia in heart disease?
How do beta blockers primarily contribute to the management of ischemic heart disease?
How do beta blockers primarily contribute to the management of ischemic heart disease?
What happens when the lumen of a coronary artery is reduced by 80-90%?
What happens when the lumen of a coronary artery is reduced by 80-90%?
What is the role of nitroglycerin in managing heart conditions?
What is the role of nitroglycerin in managing heart conditions?
What differentiates NSTEMI from STEMI in terms of treatment options?
What differentiates NSTEMI from STEMI in terms of treatment options?
What differentiates unstable angina from stable angina in terms of symptom patterns?
What differentiates unstable angina from stable angina in terms of symptom patterns?
Which of the following treatment strategies is most appropriate for managing stable angina?
Which of the following treatment strategies is most appropriate for managing stable angina?
During which condition is sudden cardiac death most commonly associated?
During which condition is sudden cardiac death most commonly associated?
Which of the following pharmacologic agents is primarily used in the acute treatment of angina symptoms?
Which of the following pharmacologic agents is primarily used in the acute treatment of angina symptoms?
What is the most appropriate first-line medication for a patient diagnosed with unstable angina?
What is the most appropriate first-line medication for a patient diagnosed with unstable angina?
Which condition is characterized by intermittent chest pain that resolves with rest and often correlates with exertional activities?
Which condition is characterized by intermittent chest pain that resolves with rest and often correlates with exertional activities?
In the management of ischemic heart disease, what is the primary goal of therapy for patients with unstable angina?
In the management of ischemic heart disease, what is the primary goal of therapy for patients with unstable angina?
Which clinical feature would most likely suggest the transition from stable angina to unstable angina?
Which clinical feature would most likely suggest the transition from stable angina to unstable angina?
Flashcards are hidden until you start studying
Study Notes
Venous Side (Right)
- Capillary oncotic pressure (πc) pulls fluid back into the capillary from the interstitial space.
- Albumin is a key protein that drives πc.
- Excess fluid is absorbed by the lymphatic system to prevent tissue swelling (edema).
Edema Causes
- Increased hydrostatic pressure:
- Can be caused by generalized global increase in arteriolar blood pressure.
- Malignant hypertension is an example of extreme blood pressure increases that can overwhelm normal fluid movement.
- Endocrine causes: Hormonal imbalances that affect blood volume and vascular tone.
- Decreased venous drainage can be regional or global, and can increase hydrostatic pressure.
- Can be caused by generalized global increase in arteriolar blood pressure.
- Increased sodium and water retention:
- Sodium retention can occur after dietary increases.
- Kidney pathologies and decreased perfusion to the kidneys can impair sodium elimination.
- Endocrine causes: Syndrome of inappropriate ADH secretion and adrenal cortical pathologies with excess aldosterone.
- Reduced lymphatic drainage:
- Cancer that infiltrates lymph nodes, surgeries that resect lymph nodes, infections that cause fibrosis of lymph nodes, and parasitic infestations (filiariasis/elephantiasis).
- Decreased oncotic pressure:
- Albumin is the most important plasma protein for blood oncotic pressure.
- Nephrotic syndrome: Excess protein leakage from the glomerulus leads to decreased oncotic pressure. Protein filters from blood, enters the renal tubules, and is excreted in the urine.
- Hepatic failure, protein-losing enteropathies, and malnutrition can also cause decreased oncotic pressure.
- Damage to the endothelium or excessive leakiness can lead to edema, often associated with inflammation.
- Pulmonary edema due to damage to alveolar epithelium and capillary endothelium.
Edema Clinical Features
- Dependent edema is more noticeable in lower areas of the body, closer to the heart.
- Many renal diseases can cause generalized edema.
- Anasarca is a generalized edema that is particularly evident in areas with loosely connected tissue.
- Different from the massive edema of anaphylaxis.
- Pulmonary and brain edema are the most severe forms of edema.
- Edema is not just a symptom, but a causative factor in pathophysiology. Unique features of the microvasculature and air spaces (lungs) and inflexible cranial cavity (brain) result in severe consequences.
Hyperemia and Congestion
- Hyperemia: Increased blood flow from arteriolar dilation.
- Tissues turn red (erythema) due to engorged vessels with oxygenated blood.
- Example: Blood flow returning to tissue that is warming after being in the cold.
- Congestion: Passive process due to reduced outflow of blood from a tissue.
- Systemic (heart failure) or local (venous obstruction).
- Tissues take on a dusky reddish-blue color (cyanosis) due to red cell stasis and accumulation of deoxygenated blood.
- Red blood cells can extravasate, causing hemosiderin deposition.
- Hemosiderin is a degradation product of hemoglobin found mostly in macrophages.
Chronic Passive Congestion
- Long-standing congestion leads to chronic hypoxia.
- Cellular degeneration, death, tissue fibrosis, and small foci of hemorrhage can occur.
- Macrophages accumulate hemosiderin from phagocytosis of erythrocyte debris.
Congestion in Individual Tissues
- Pulmonary congestion:
- Acute: Alveolar capillaries become engorged with blood.
- Chronic: Septa thicken and become fibrotic; alveolar spaces contain hemosiderin-laden macrophages ("heart failure cells").
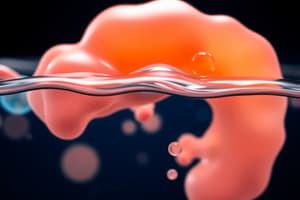
- Hepatic congestion:
- Acute: Hepatocytes degenerate; sinusoids and venules become distended with blood. Hepatocytes near the hepatic artery circulation experience less severe hypoxia and develop fatty change.
Venous Congestion
- Pulmonary congestion:
- Causes: Left heart failure, mitral stenosis, and mitral regurgitation.
- Appearance: Engorged pulmonary capillaries and venules, alveolar edema, heart failure cells, brown induration.
- Clinical features: Shortness of breath (dyspnea), wheezing, difficulty breathing while lying flat.
- Hepatic congestion:
- Causes: Right heart failure, constrictive pericarditis.
- Appearance: Enlarged liver, centrilobular necrosis, nutmeg liver.
- Clinical features: Right upper abdominal pain, elevated liver enzymes, ascites, peripheral edema, jugular venous distension.
- Deep Vein congestion:
- Causes: Blood clot formation (DVT), incompetent valves.
- Appearance: Dilated and tortuous veins, venous ulcers, potential thrombus formation.
- Clinical features: Swelling, pain, tenderness, skin changes.
White vs. Red Infarct
- White infarct: Organs with a single blood supply (e.g., kidney, spleen).
- Red infarct: Organs with a dual blood supply (e.g., lung, intestine, testis).
Septic Shock
- Infections cause widespread inflammation, resulting in dangerously low blood pressure and inadequate blood flow to vital organs.
- Fatal due to inadequate tissue perfusion, leading to cellular death, multiple organ dysfunction, systemic inflammatory responses, and failure of compensatory mechanisms.
Septic Shock Pathophysiology
- No single diagnostic test, but scoring systems are used to identify high-risk patients.
- General characteristics:
- Dysregulated vascular reflexes: Inappropriate vasodilation and potential edema due to endothelium damage.
- Increased pro-inflammatory cytokines: Adverse impacts on tissues like the heart and kidneys.
- Leukocyte movement into organs: Organ dysfunction.
- Activation of coagulation and complement cascades.
Stages of Shock
- Stage I (Compensated): Tachycardia, but blood pressure is normal.
- Stage II (Decompensated): Body is no longer compensating for reduced tissue flow; tachycardia and hypotension, difficult to reverse.
- Stage III (Irreversible): Death likely if not corrected quickly - Difficult to treat; high tachycardia or bradycardia, hypotension, decreased organ function (renal failure, impaired heart function, decreased level of consciousness).
Multi-Organ Dysfunction
- Multiple organs fail due to lack of oxygen and blood.
- Prognosis is poor.
General Shock Clinical Findings
- Hypovolemic and cardiogenic Shock: Hypotension, weak and rapid pulse, tachypnea, cool, clammy, cyanotic skin.
- Septic shock: Same as above, but skin may initially be warm and flushed due to peripheral vasodilation.
Ischemic Heart Disease
- Inadequate blood supply to the myocardium to meet its metabolic demands.
- Most commonly caused by atherosclerosis of the coronary arteries.
- Other causes: Aneurysms, autoimmune attacks, coronary vasospasm.
- Leading cause of death worldwide.
Pathogenesis of Ischemic Heart Disease
- Progressive narrowing of coronary arteries: Leads to hypoperfusion of myocardium and potential heart failure.
- Sudden occlusion of a major coronary artery: Atherosclerotic plaque rupture causes acute clot formation, blocking the artery or creating an embolus that blocks blood flow downstream, leading to an infarct.
- Exacerbated by increased heart metabolic activity.
Factors Affecting Heart Metabolic Demand
- Heart rate: Faster heart rate uses more energy.
- Wall tension: Determined by volume and pressure within the heart chambers.
- A dilated heart requires more energy than a normal-sized heart.
- Laplace's Law: 𝝈= 𝑷 ∙𝒓 / 𝒉
- Contractility: Influenced by intracellular calcium ions.
Causes of IHD
- Coronary atherosclerosis is the most common primary cause
- Other factors often exacerbate oxygen delivery or cardiac oxygen consumption
Pathogenesis - Influence of Atherosclerosis
- Atherosclerosis is the major cause of ischemic heart disease (IHC), representing 90% of cases
- With a 50-75% reduction in lumen size of a large coronary artery, there are usually IHC symptoms during increased activity.
- When 80-90% reduction is observed, there are often symptoms at rest.
- Often, there is more than one cause for IHC
- i.e., hypertension and a hypertrophic heart in combination with atherosclerotic coronary arteries.
General Pathophysiologic Concepts
- A healthy person has a substantial coronary flow reserve, and myocardial perfusion can increase to five times resting levels with intense exercise.
- Myocardial circulation is mainly controlled by constriction and dilation of small, intramyocardial branches less than 400 μm in diameter.
- Reduction in blood pressure distal to the narrowed zone occurs in advanced atherosclerosis of the main epicardial coronary arteries.
- Maximal blood flow to the myocardium is not impaired until about 75% of the cross-sectional area of an epicardial coronary artery is compromised by atherosclerosis.
- Resting blood flow is not reduced until greater than 90% of the lumen is occluded.
Pathophysiology - Types of IHD Presentation
- Stable angina: When there is a plaque or thrombosis causing occlusion, the obstruction is thought to be stable.
- Acute coronary syndromes (ACS):
- Unstable angina: Could be a thrombus that forms and breaks down constantly over a plaque. Could be a very significant stable occlusion that limits flow. Other rare conditions, like vasospastic angina, could be the cause.
- **Non-ST elevation myocardial infarction (NSTEMI) **
- ST-elevation myocardial infarction (STEMI)
Pathophysiology - Unstable Angina
- Prinzmetal angina (vasospastic or variant angina):
- Technically a type of unstable angina with better prognosis
- Caused by coronary artery spasm
- Occurs early morning; unrelated to exertion
- Usually doesn’t cause infarction
- Responds well to vasodilators (nitroglycerine, calcium channel blockers)
- Typical patient population: younger ( less than 60 years), women.
Adaptations to Chronic Ischemia in the Heart
- Hypertrophy and changes to the molecular mechanisms of contraction in cardiac myocytes (more on this later)
- Ischemic cardiomyopathy
- Development of coronary collateral circulation
Hmmmm…
- Intracelular Ca2+
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.